
A more recent article on acute and chronic prostatitis is available.
Am Fam Physician. 2010;82(4):397-406
Patient information: See related handout on prostatitis.
Author disclosure: Nothing to disclose.
Prostatitis ranges from a straightforward clinical entity in its acute form to a complex, debilitating condition when chronic. It is often a source of frustration for the treating physician and patient. There are four classifications of prostatitis: acute bacterial, chronic bacterial, chronic prostatitis/chronic pelvic pain syndrome, and asymptomatic. Diagnosis of acute and chronic bacterial prostatitis is primarily based on history, physical examination, urine culture, and urine specimen testing pre- and post-prostatic massage. The differential diagnosis of prostatitis includes acute cystitis, benign prostatic hyperplasia, urinary tract stones, bladder cancer, prostatic abscess, enterovesical fistula, and foreign body within the urinary tract. The mainstay of therapy is an antimicrobial regimen. Chronic pelvic pain syndrome is a more challenging entity, in part because its pathology is poorly understood. Diagnosis is often based on exclusion of other urologic conditions (e.g., voiding dysfunction, bladder cancer) in association with its presentation. Commonly used medications include antimicrobials, alpha blockers, and anti-inflammatory agents, but the effectiveness of these agents has not been supported in clinical trials. Small studies provide limited support for the use of nonpharmacologic modalities. Asymptomatic prostatitis is an incidental finding in a patient being evaluated for other urologic problems.
The prevalence of prostatitis is approximately 8.2 percent (range: 2.2 to 9.7 percent).1 It accounts for 8 percent of visits to urologists, and up to 1 percent of visits to primary care physicians.2 In 2000, the estimated cost to diagnose and treat prostatitis was $84 million, not including pharmaceutical spending.3 Men with chronic prostatitis experience impairment in mental and physical domains of health-related quality of life as measured through validated questionnaires.4 In 2002, approximately 14 percent of men with a medical claim for prostatitis missed work.3 These statistics clearly underscore the broad and far-reaching effect of prostatitis on patient quality of life and the economic impact of the condition.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| The 2-glass pre- and post-prostatic massage test is a reasonable alternative to the preferred Meares-Stamey 4-glass test for diagnosing prostatitis. | C | 7 |
| Optimal duration of antibiotic treatment for acute bacterial prostatitis is six weeks. | B | 16, 17 |
| In acute bacterial prostatitis, patients should be evaluated with imaging for abscess if fevers persist more than 36 hours after appropriate antibiotic coverage. | C | 9, 17 |
| To prevent symptom flare-up, suppressive low-dose antibiotics should be considered in men with chronic bacterial prostatitis whose cultures remain positive. | C | 15, 16 |
Prostatitis is a broad diagnosis that encompasses four clinical entities, including acute illness requiring immediate attention (acute bacterial prostatitis), two chronic conditions (chronic bacterial prostatitis, chronic pelvic pain syndrome), and an incidental finding (asymptomatic prostatitis) noted during the evaluation and treatment of other urologic conditions. This article will familiarize primary care physicians with the categories of prostatitis as defined by the National Institutes of Health (NIH; Table 15) and elucidate the epidemiology, clinical presentation, diagnosis, and treatment of each.6
| Type of syndrome | Description | WBC count per HPF (400x) | Bacteria cultures | ||||
|---|---|---|---|---|---|---|---|
| VB1* | VB2† | EPS | VB3‡ | ||||
| I. Acute bacterial prostatitis | Acute infection of the prostate gland | > 10 | + | + | § | + | |
| II. Chronic bacterial prostatitis | Chronic infection of the prostate gland | > 10 | — | — | + | + | |
| III. Chronic pelvic pain syndrome | Chronic pelvic pain in the absence of bacteria localized to the prostate | > 10 | — | — | — | — | |
| A. Inflammatory | Significant WBC count in the EPS, VB3, or semen | ||||||
| B. Noninflammatory | Insignificant WBC count in the EPS, VB3, or semen | < 10 | — | — | — | — | |
| IV. Asymptomatic prostatitis | WBC count and/or bacteria in the EPS, VB3, semen, or histologic specimens of prostate gland in asymptomatic patients | > 10 | — | — | — | — | |
Diagnostic Testing
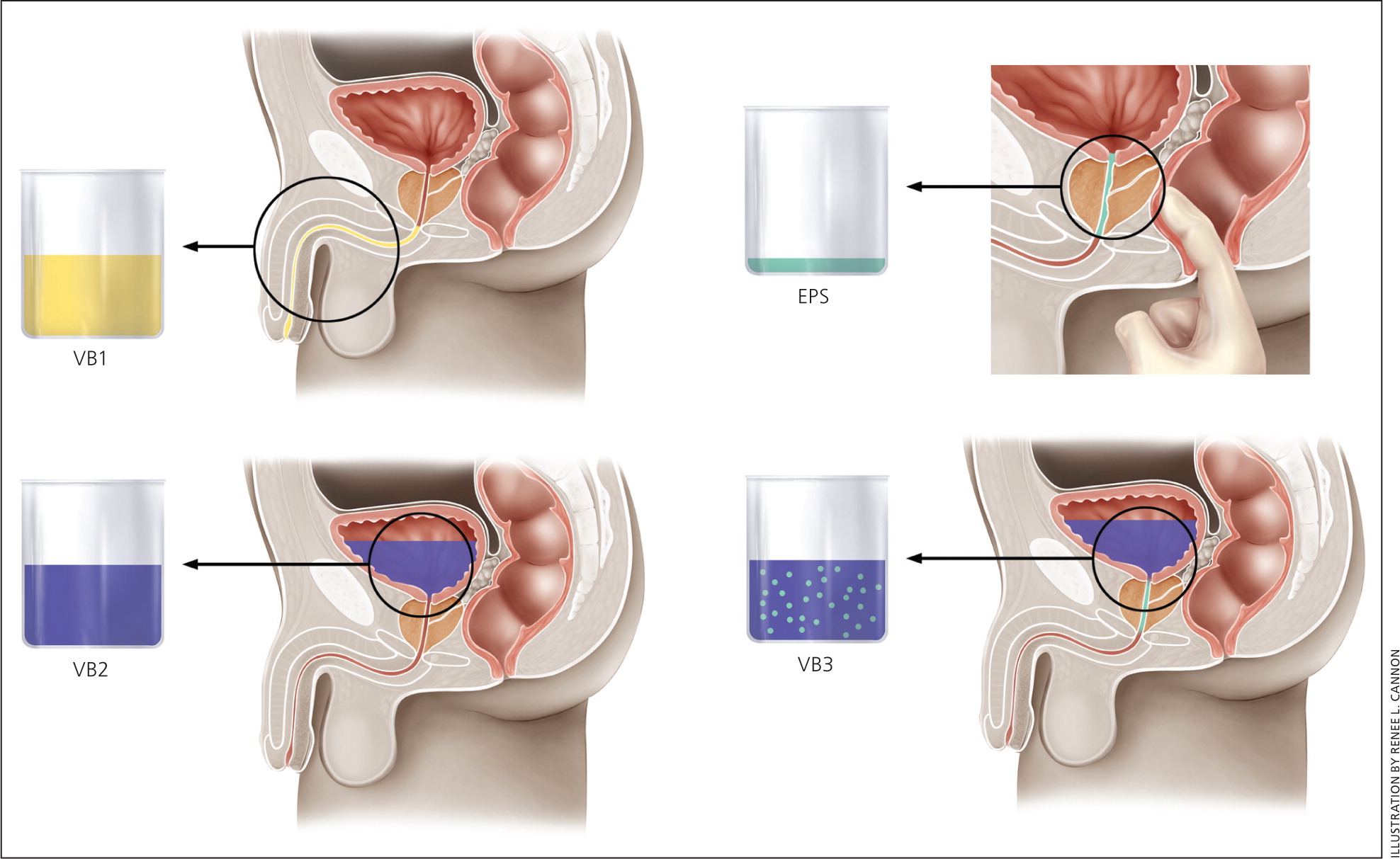
A number of diagnostic tests are available to differentiate and categorize the four types of prostatitis. These include localization tests and expressed prostatic secretions, the 2-glass pre- and post-prostatic massage and Meares-Stamey 4-glass tests (Table 27,8 and Figure 1), and urine Gram stain and culture. Measurement of postvoid residual urine is recommended when obstruction is suspected.
| Test | VB1† | VB2A‡ | EPS§ | VB3|| | Semen analysis | Comment |
|---|---|---|---|---|---|---|
| Meares-Stamey 4-glass | X | X | X | X | Preferred test; lack of validating evidence | |
| 2-glass pre- and post-prostatic massage | X | X | Good concordance with Meares-Stamey 4-glass test; reasonable alternative | |||
| Alternative (2 glasses)7 | X | X | Higher sensitivity than EPS for gram-negative organisms (97 vs. 84 percent) and higher sensitivity for gram-positive organisms (100 vs. 16 percent) Semen cultures recommended only if high index of suspicion for chronic bacterial infection despite negative urine cultures |
Semen analysis, prostate-specific antigen (PSA) level, and transrectal ultrasonography–guided biopsy are not specifically recommended in the evaluation of patients with prostatitis; however, these tests may already have been obtained in patients being evaluated for other urologic problems. Similarly, imaging has a role only in the exclusion of other urologic diagnoses,9 and when a patient with acute bacterial prostatitis does not respond appropriately to initial antimicrobial therapy. Other laboratory testing (e.g., complete blood count [CBC], electrolyte levels, blood culture) is not routine but may be performed as necessary in a patient who appears systemically ill or who may have impaired renal function and in whom antimicrobial therapy is being contemplated.
| Type of syndrome | Differential diagnosis | Symptoms | Physical examination | Diagnostic tests | Therapy | |
|---|---|---|---|---|---|---|
| I. Acute bacterial prostatitis | Acute cystitis, prostatic abscess | Urinary: straining, urgency, dysuria, hesitancy, frequency, obstruction, irritation Systemic: fever, malaise, arthralgia, myalgia, intense suprapubic pain, mildly to acutely ill appearance, chills, nausea, emesis, and signs of sepsis (tachycardia and hypotension) | Tender, boggy, enlarged prostate on digital rectal examination; distended bladder; prostatic massage contraindicated | Urine culture, postvoid residual | Antimicrobial therapy Hospitalization for severe cases of prostate infection | |
| II. Chronic bacterial prostatitis | Benign prostatic hyperplasia, stones or foreign body within the urinary tract, bladder cancer, prostatic abscess, enterovesical fistula | Irritative voiding symptoms; testicular, low back, or perineal pain; recurrent urinary tract infection; urethritis; epididymitis; distal penile pain | Prostatic massage; prostate can be normal, tender, or boggy on digital rectal examination | 2-glass pre- and post-prostatic massage test, postvoid residual | Antimicrobial therapy | |
| III. Chronic pelvic pain syndrome | Benign prostatic hyperplasia, voiding dysfunction, bladder or prostate cancer, prostatic or müllerian duct remnants, interstitial cystitis, radiation cystitis, eosinophilic cystitis, chronic proliferative cystitis, neuropathic pain, ejaculatory duct obstruction | Symptoms of chronic pelvic pain and possible voiding symptoms | Abdominal and digital rectal examination to exclude underlying pathology; no tenderness to diffuse tenderness; findings variable | National Institutes of Health Chronic Prostatitis Symptom Index,* 2-glass pre- and post-prostatic massage test | Multimodal: combination pharmacologic and nonpharmacologic | |
| A. Inflammatory | ||||||
| B. Noninflammatory | ||||||
| IV. Asymptomatic prostatitis | — | No symptoms; incidental finding during evaluation for other conditions (i.e., infertility or elevated prostate-specific antigen level) | No disease-specific abnormalities | Semen analysis, prostate biopsy | No specific therapy required; treatment depends on underlying conditions and reasons for initial evaluation | |
Acute Bacterial Prostatitis
EPIDEMIOLOGY AND PATHOGENESIS
Acute bacterial prostatitis, NIH type I, is an acute bacterial infection of the prostate; patients are typically seen in the outpatient setting or emergency department. Left untreated, it can lead to overwhelming sepsis or the development of prostatic abscess. The prevalence and incidence of acute bacterial prostatitis are not fully known.11 By definition, an organism must be identified on culture. Escherichia coli is the most commonly isolated organism, but other gram-negative organisms, such as Klebsiella, Proteus, and Pseudomonas, and gram-positive Enterococcus species are often isolated as well. Other gram-positive organisms, many of which comprise normal skin flora, have also been isolated from patients with suspected bacterial prostatitis and should be treated accordingly.12,13 Sexually active men younger than 35 years and older men who engage in high-risk sexual behaviors should be tested for Neisseria gonorrhoeae and Chlamydia trachomatis.
CLINICAL PRESENTATION
The diagnosis of acute bacterial prostatitis is often based on symptoms alone. Urinary symptoms may be irritative (e.g., urinary frequency, urgency, dysuria) or obstructive (e.g., hesitancy, poor or interrupted stream, straining to void, incomplete emptying). Pain may be present in the suprapubic or perineal region, or in the external genitalia. Systemic symptoms of fever, chills, malaise, nausea, emesis, and signs of sepsis (tachycardia and hypotension) may be present as well. On physical examination, the prostate should be gently palpated. Prostatic massage should not be performed and may be harmful14; the prostate is tender, enlarged, and boggy. On abdominal examination, a palpable, distended bladder indicates urinary retention.
DIAGNOSIS
Midstream urine culture should be obtained. The presence of more than 10 white blood cells per high-power field suggests a positive diagnosis. Other laboratory testing (e.g., CBC, electrolyte levels, blood culture) is determined by the severity of the presentation. Residual urine should be documented if a patient has a palpable bladder or symptoms consistent with incomplete emptying.
TREATMENT
Empiric therapy should be started at the time of evaluation (Figure 2); coverage can be tailored to the isolated organisms once urine culture results are available. Mildly to moderately ill patients may be treated in the outpatient setting; severely ill patients or those with possible urosepsis require hospitalization and parenteral antibiotics. Once patients have become afebrile, they may be transitioned to oral antibiotics based on the culture results. Minimal duration of treatment is four weeks15; however, the optimal period has been shown to be six weeks, because of the possible persistence of bacteria, with repeat evaluation recommended at that time.16,17
If fever persists or the maximal temperature fails to show a downward trend after 36 hours, prostatic abscess should be suspected.9 Urology consultation should be obtained; if it is not immediately available, imaging may be performed with computed tomography, magnetic resonance imaging, or transrectal ultrasonography. Prostatic abscess requires urology consultation for drainage.17
SPECIAL CONSIDERATIONS
No specific guideline exists for the treatment of gram-positive organisms, but the fluoroquinolones have adequate gram-positive coverage, as well as excellent gram-negative coverage, and they penetrate the prostate well. C. trachomatis and N. gonorrhoeae are best treated with azithromycin (Zithromax) or doxycycline.18
Immunocompromised patients, especially those who have uncontrolled diabetes mellitus, among other immunodeficiencies, seem to be more susceptible to the development of acute bacterial prostatitis and prostatic abscess.19 Treatment is as outlined previously, including drainage with broad-spectrum antibiotic coverage.
Rarely, transrectal ultrasonography–guided biopsy of the prostate results in acute bacterial prostatitis and septicemia. These patients are often ill enough to warrant hospital admission and the initiation of parenteral therapy.20
Chronic Bacterial Prostatitis
Chronic bacterial prostatitis, NIH type II, is a persistent bacterial infection of the prostate lasting more than three months. Urine cultures obtained over the course of illness repeatedly grow the same bacterial strain. The NIH Chronic Prostatitis Symptom Index from the Chronic Prostatitis Collaborative Research Network (CPCRN) is a validated questionnaire available at http://www.prostatitis.org/symptomindex.html.
EPIDEMIOLOGY AND PATHOGENESIS
E. coli is the most commonly isolated organism, but other gram-negative organisms such as Klebsiella, Proteus, and Pseudomonas are also common.12,13 After E. coli, gram-positive Enterococcus is the next most commonly isolated pathogen.21 Research suggests that the E. coli strains often seen in chronic bacterial prostatitis have a higher virulence factor and greater degree of biofilm formation than the strains seen in uncomplicated urinary tract infections, which could explain why bacterial prostatitis is so difficult to treat.22 The pathogenesis of chronic bacterial prostatitis has not been scientifically proven, but it is assumed that the infection moves from the distal urethra to the prostate. Other possibilities include seeding from the bladder, bowel, blood, or lymphatic system.23 Suggested associations include presence of foreskin, sexual activity, benign prostatic hyperplasia, urethral stricture, bladder neck hypertrophy, previous instrumentation or catheterization, and anatomic predisposition for retrograde spread from intraprostatic ducts.24,25
CLINICAL PRESENTATION
In contrast to men with acute bacterial prostatitis, those with chronic bacterial prostatitis do not appear to be ill. They present with recurrent or relapsing urinary tract infections, urethritis, or epididymitis with the same bacterial strain. Between symptomatic episodes, detectable pathogens persist on localization tests. Patients may have irritative voiding symptoms and testicular, perineal, low back, and occasionally distal penile pain. On physical examination, patients are usually afebrile, and on digital rectal examination the prostate may feel normal, tender, or boggy.
DIAGNOSIS
TREATMENT
Because chronic bacterial prostatitis is a bacterial infection, an appropriate antibiotic with good tissue penetration in the prostate should be selected (Table 4). Fluoroquinolones have demonstrated the best tissue concentration and are recommended as first-line agents.26,27 Although trimethoprim/sulfamethoxazole (Bactrim, Septra) may be considered, the tissue penetration may not be as effective, and in many areas of the United States there is evidence of increasing uropathogenic resistance.27 Penicillin derivatives, commonly used to treat acute bacterial prostatitis, have not been shown to provide good symptom relief for chronic bacterial prostatitis.17 Second-line drugs include doxycycline, azithromycin, and clarithromycin (Biaxin). A four- to six-week course of therapy is usually recommended; however, a six- to 12-week course is often needed to eradicate the causative organism and to prevent recurrence, especially if symptoms persist after completion of the initial therapy. No guideline exists for treating gram-positive organisms, but ciprofloxacin (Cipro) and levofloxacin (Levaquin) have adequate gram-positive coverage, as well as excellent gram-negative coverage, and both medications penetrate the prostate tissue well.
| Drug | Dosage | Cost of generic (brand)* | In retail discount programs† | |
|---|---|---|---|---|
| First-line antibiotics | ||||
| Fluoroquinolones | ||||
| Ciprofloxacin (Cipro) | 500 mg twice daily | $28 ($354) | ✓ | |
| Levofloxacin (Levaquin) | 500 mg once daily | NA ($416) | ||
| Norfloxacin (Noroxin) | 400 mg twice daily | NA ($235) | ||
| Trimethoprim/sulfamethoxazole(Bactrim DS, Septra DS)e | 160 mg/800 mg twice daily | $40 ($146) | ✓ | |
| Second-line antibiotics | ||||
| Doxycycline | 100 mg twice daily | $20 to 40 ($392) | ✓ | |
| Azithromycin (Zithromax) | 500 mg once daily | $438 ($611) | ||
| Clarithromycin (Biaxin) | 500 mg twice daily | $219 ($324) | ||
SPECIAL CONSIDERATIONS
Patients who test positive for human immunodeficiency virus (HIV) infection deserve special mention because they are susceptible to additional pathogens, such as Serratia marcescens, Salmonella typhi, Mycobacterium tuberculosis, and Mycobacterium avium. Nonbacterial organisms (e.g., Candida, Cryptococcus, Histoplasma, and Aspergillus species) should also be considered.28 Recommended treatment for patients who are HIV positive is a four- to six-week course of antibiotics followed by suppressive antibiotics for an unspecified time.28
Chronic Prostatitis/Chronic Pelvic Pain Syndrome
EPIDEMIOLOGY
Chronic prostatitis/chronic pelvic pain syndrome is subdivided into two categories: NIH type IIIA (inflammatory) and IIIB (noninflammatory; Table 15). Differentiation between these groups has been made based on the presence of leukocytes in expressed and post-massage prostatic secretions, urine, or semen. One of the greatest challenges with the treatment of chronic prostatitis/chronic pelvic pain syndrome is that there is no clear understanding of the etiology; however, suggested explanations include infection, autoimmunity, and neuromuscular spasm.29
In 2006, the CPCRN published a prospective analysis of NIH type III prostatitis symptoms over two years.30 This group concluded that symptoms vary widely among patients, there is no evidence that the disease worsens, and approximately one third of patients will improve with or without treatment.
CLINICAL PRESENTATION
The hallmark symptom of chronic prostatitis/chronic pelvic pain syndrome is pain attributed to the prostate with no demonstrable evidence of infection. On examination, tenderness of the prostate, or less commonly the pelvis, is present in about one half of patients.31
DIAGNOSIS
Evaluation and diagnosis of chronic prostatitis/chronic pelvic pain syndrome can be confusing and challenging for the treating physician. Many of the diagnostic tests performed in affected patients are geared toward excluding other treatable pathology (e.g., benign prostatic hyperplasia, bladder cancer), and urology referral is often necessary.
In a series of two studies, the CPCRN evaluated the usefulness of leukocytes and bacterial counts to subcategorize patients with chronic prostatitis/chronic pelvic pain syndrome. The group found that leukocytes and bacterial counts did not correlate with symptoms,32 and positive findings were often present in asymptomatic control patients.33 The utility and importance of such tests on the treatment and outcome of patients with chronic prostatitis/chronic pelvic pain syndrome remain unclear.
| Type of testing | North American consensus34 | International consensus35 |
|---|---|---|
| Mandatory/basic evaluation | ||
| Clinical | History, physical examination (digital rectal examination) | History, physical examination (digital rectal examination) |
| Imaging | None | None |
| Laboratory | Urinalysis and midstream culture | Urinalysis and midstream culture |
| Urologic testing | None | None |
| Recommended/further testing | ||
| Clinical | NIH Chronic Prostatitis Symptom Index36 | NIH Chronic Prostatitis Symptom Index36 |
| Imaging | None | None |
| Laboratory | Lower urinary tract localization tests, urine cytology | Lower urinary tract localization tests |
| Urologic testing | Postvoid residual, flow rate | Postvoid residual, flow rate |
| Optional/selected patient populations | ||
| Clinical | None | International Prostate Symptom Score (http://www.usrf.org/questionnaires/AUA_SymptomScore.html) |
| Imaging | Transrectal ultrasonography–guided biopsy, abdominal/pelvic imaging (CT, MRI, ultrasonography) | Transrectal ultrasonography–guided biopsy, abdominal/pelvic imaging (CT, MRI, ultrasonography) |
| Laboratory | Semen analysis and culture, urethral swab, prostate-specific antigen level | Semen analysis and culture, urethral evaluation with first 10 mL of voided urine or swab for culture, urine cytology, prostate-specific antigen level |
| Urologic testing | Pressure flow study, video urodynamics (flow-electromyography), cystoscopy | Pressure flow study, video urodynamics (flow-electromyography), cystoscopy |
TREATMENT
There is no preferred first-line treatment for patients with chronic pelvic pain syndrome (Table 638–51 and Figure 338 ). It is reasonable to try antimicrobials, alpha blockers, or anti-inflammatory medications first; however, if a patient does not respond to treatment, repeated trials are not warranted. In addition, it is important to consider multimodal therapy with a combination of medications or possible adjunctive therapy with non-pharmacologic modalities. Men with chronic pelvic pain syndrome represent a highly complex group of patients, and urology referral is often necessary.
| Type of therapy | Dosage/treatment plan | Comments | |
|---|---|---|---|
| Pharmacologic | |||
| First-line | |||
| Antimicrobials | Ciprofloxacin (Cipro), 500 mg orally twice daily for four to six weeks Trimethoprim/sulfamethoxazole (Bactrim, Septra), 160 mg/800 mg orally twice daily for four to six weeks38 | No difference between ciprofloxacin and no ciprofloxacin (P = .15)38,39 | |
| Second-line | |||
| Alpha blockers | Tamsulosin (Flomax), 0.4 mg daily Alfuzosin (Uroxatral), 10 mg daily for 12 weeks | No difference compared with placebo39 Decline of National Institutes of Health Chronic Prostatitis Symptom Index score ≥ 4 showed no difference compared with placebo40 | |
| Third-line | |||
| Anti-inflammatory agents | Pentosan (Elmiron), 900 mg daily for 16 weeks Finasteride (Proscar), 5 mg daily for six months Quercetin (a bioflavonoid supplement), 500 mg twice daily for 30 days | Clinical global improvement: 36.7 vs.17.8 percent with placebo41 Global assessment improvement: 44 vs. 27 percent with placebo42 67 percent quercetin vs. 20 percent placebo showed > 25 percent improvement in symptoms43 | |
| Other | |||
| Anticonvulsants | Pregabalin (Lyrica) Gabapentin (Neurontin) | No specific data44 | |
| Tricyclic antidepressants | Nortriptyline (Pamelor), 10 mg daily at bedtime with titration up to 75 to 100 mg | No specific data45 | |
| Nonpharmacologic | |||
| Biofeedback | — | Small study, statistically significant improvement in American Urological Association symptom score, decrease in bother score, decrease in pain score46 | |
| Cognitive behavior therapy | — | No published data47 | |
| Physical therapy | — | Small pilot study, no difference in improvement between global massage therapy vs. myofascial physical therapy 48 | |
| Sacral neuromodulation | — | Two uncontrolled studies have shown some effectiveness49,50 | |
| Thermal therapy | Microwave and transurethral needle ablation | Little improvement, consider as last resort51 | |

Asymptomatic Prostatitis
Asymptomatic prostatitis, NIH type IV, is diagnosed when inflammatory cells are identified on prostate biopsy or leukocytes are noted on semen analysis during urologic evaluation for other reasons. The clinical significance of this type of prostatitis is uncertain, and treatment is based on the primary reason for the urologic evaluation. When the indication for biopsy is an elevated PSA level, it is important to remember that normalization of the PSA value after antibiotic or 5-alpha reductase inhibitor therapy does not rule out the diagnosis of prostate cancer, and continued urologic evaluation is warranted.
