
Am Fam Physician. 2012;86(6):535-541
A more recent article on lice and scabies is available.
Related letter: Additional Techniques for Diagnosing Scabies
Patient information: See related handout on lice and scabies.
Author disclosure: No relevant financial affiliations to disclose.
Pediculosis and scabies are caused by ectoparasites. Pruritus is the most common presenting symptom. Head and pubic lice infestations are diagnosed by visualization of live lice. Finding nits (louse egg shells) alone indicates a historical infestation. A “no nit” policy for schools and day care centers no longer is recommended because nits can persist after successful treatment with no risk of transmission. First-line pharmacologic treatment of pediculosis is permethrin 1% lotion or shampoo. Multiple novel treatments have shown limited evidence of effectiveness superior to permethrin. Wet combing is an effective nonpharmacologic treatment option. Finding pubic lice should prompt an evaluation for other sexually transmitted infections. Body lice infestation should be suspected when a patient with poor hygiene presents with pruritus. Washing affected clothing and bedding is essential if lice infestation is found, but no other environmental decontamination is necessary. Scabies in adults is recognized as a pruritic, papular rash with excoriations in a typical distribution pattern. In infants, children, and immunocompromised adults, the rash also can be vesicular, pustular, or nodular. First-line treatment of scabies is topical permethrin 5% cream. Clothing and bedding of persons with scabies should be washed in hot water and dried in a hot dryer.
Pediculosis and scabies are caused by ectoparasites. Pruritus is the most common presenting symptom in persons with either condition. Determining the etiology is important and straightforward based on history and physical examination; however, pediculosis may be overdiagnosed by anxious patients and overtreated by physicians without an office evaluation. An accurate diagnosis may have an impact on reducing resistance of lice to currently available treatments.
| Clinical recommendation | Evidence rating | References | Comments |
|---|---|---|---|
| Schools and day care facilities should abandon “no nit” policies for the treatment and prevention of head lice because finding nits alone does not indicate active infestation. | C | 7 | Recommendation from evidence-based guidelines based on basic knowledge of lice life cycle |
| Topical therapies should be used twice, at day 0 and again at day 7 to 10, to fully eradicate lice. | C | 3, 7, 8 | Recommendation from consensus review based on known lice life cycle |
| Inappropriate retreatment may result in resistance or lack of effectiveness | |||
| Permethrin 1% lotion or shampoo (Nix) is first-line treatment for pediculosis, except in places with known permethrin resistance. | C | 3, 7 | Evidence-based guidelines from information in the United States, balancing effectiveness and toxicity |
| Physicians should consider the diagnosis of scabies when evaluating a patient with a papular, pruritic rash. | C | 27–30 | Scabies may not always present as the classic burrows in webs and creases |
| Ivermectin (Stromectol) should be reserved for patients with classic scabies who do not improve with topical permethrin treatment. | C | 18 | Guidelines using consensus agreement in area of little clinical research |
Pediculosis
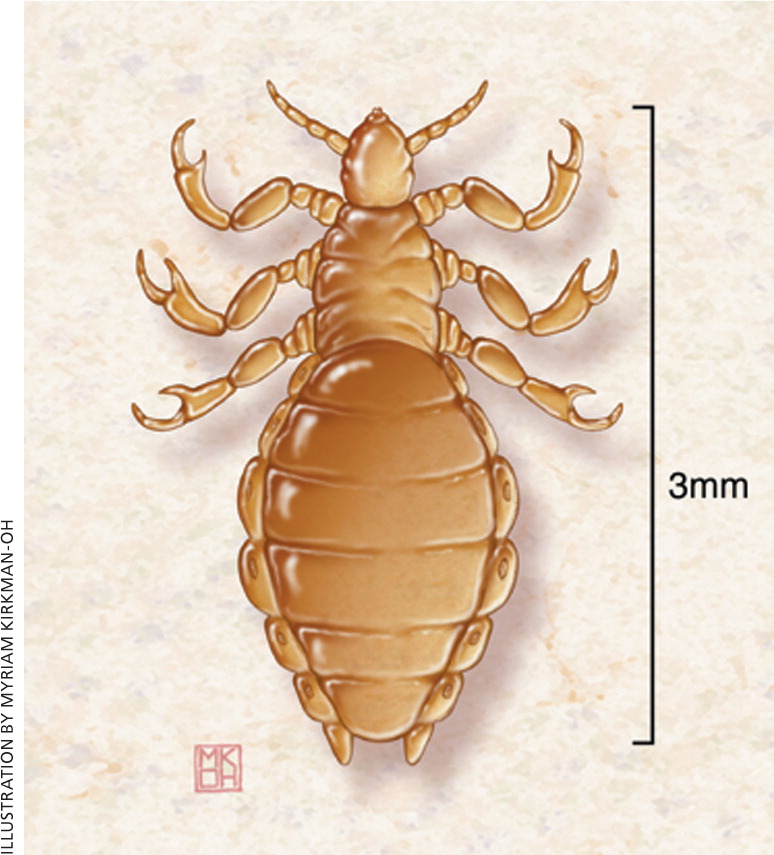
Lice are obligate, blood-sucking parasites that can infest the head (Pediculus humanus var capitis), body (Pediculus humanus var corporis), and pubic region (Phthirus pubis).1 Body and scalp lice are approximately 1 to 3 mm long, or about the size of a sesame seed, and are flattened dorsoventrally. The pubic louse is much shorter. Lice are unable to jump or fly; consequently, transmission requires close contact.2 The female insect's life cycle lasts for one to three months, and she lays up to 300 eggs at the skin-hair junction that hatch and mature to adults in 20 days.1 Eggs are yellow to white in color, and can be found attached to the base of body hairs.
CLINICAL PRESENTATION
Persons with pediculosis typically present with pruritus. Pruritus associated with lice is a delayed hypersensitivity reaction. It may take two to six weeks to develop after the first exposure, with future episodes resulting in pruritus within one to two days of exposure.3 Intense itching leads to scratching, with subsequent excoriations and secondary cellulitis. In longstanding infestation, the skin may become lichenified and hyperpigmented, particularly on the trunk. Finding pubic lice should prompt an evaluation for other sexually transmitted infections.
DIAGNOSIS
Head lice infestation is diagnosed definitively by finding at least one live louse on visual inspection (Figure 14 ). Visualization can be improved by the use of a bright light, a magnifying lens, and combing the hair with a “lice comb” (fine-toothed comb) and examining the comb teeth.5 Lice are commonly found behind the ears and on the back of the neck.6
Misdiagnosis is common. Finding only nits (louse eggs that may or may not be viable) on examination is not enough to indicate current infestation. Diagnosis requires observation of live lice. Additionally, nits can be confused with dandruff, hair spray debris, or dirt particles. Nits may remain on the hair for months after successful treatment. For all of these reasons, school- or day care–based “no nit” polices are not recommended by the American Academy of Pediatrics, and are thought to be harmful because they can result in significant absence from school.7 When lice are found in one family member, the entire family should be examined and treated if live lice are found on the head. Fomite transmission of lice is controversial, but lice have been found on clothing, towels, and sheets. Washing these items in water that is at least 122°F (50°C) provides effective lice eradication. Sprays, carpet treatments, and other chemical environmental decontamination measures are not necessary and can be harmful.3
Pubic lice infestation is diagnosed by finding lice on the pubic hair (Figure 2). Body lice should be suspected in patients with pruritus living in conditions of crowding and poor hygiene. Diagnosis is confirmed by identification of body lice in the seams of clothing.
PHARMACOLOGIC TREATMENT (HEAD LICE)
Pharmacologic treatment of head lice infestation is focused on two general mechanisms: neurotoxicity that results in paralysis of the louse and suffocation via “coating” the louse. Most clinical trials use substances that work via neurotoxicity through topical products like lindane 1% shampoo, permethrin 1% lotion (Nix), pyrethrins 0.3%/piperonyl butoxide 4% shampoo or mousse (Rid), and malathion 0.5% lotion (Ovide) (Table 17 ). Permethrin is recommended as first-line treatment for pediculosis.7
| Treatment | Ovicidal | Directions | Cost* | Comments |
|---|---|---|---|---|
| Benzyl alcohol 5% lotion (Ulesfia) | No |
| $63 (227-g bottle) |
|
| Ivermectin (Stromectol; not FDA-approved for treatment of pediculosis) | Partial |
| $5 to $10 per 3-mg tablet (total cost dependent on weight) |
|
| Malathion 0.5% lotion (Ovide) | Partial |
| $185 (59-mL bottle) |
|
| Permethrin 1% lotion (Nix) | No |
| $20 for two 59-mL bottles |
|
| Pyrethrins 0.3%/piperonyl butoxide 4% shampoo or mousse (Rid) | No |
| $20 for 236 mL |
|
A key to formulating an effective treatment regimen is recognizing that available treatments destroy lice, but do not reliably destroy eggs. Repeat treatment typically is required for complete eradication, timed on the life cycle of the louse.8 The initial treatment followed by a second treatment seven to 10 days later should be sufficient to eradicate most nonresistant lice. Trials that use single-dose treatment may not fully evaluate the true effectiveness of the drugs.
Resistance to permethrin and pyrethrin/piperonyl butoxide can be significant in various communities, necessitating the use of malathion, which has maintained relatively low resistance because of limited use in the United States. In the United Kingdom, malathion is used often and resistance is common.7
Although lindane still is available by prescription in most of the United States, the U.S. Food and Drug Administration (FDA) has cautioned against its use because of neurotoxicity concerns. It is not available in California or in the United Kingdom. Lindane may be used as a second-line agent in adults, but should not be used in children, older persons, or adults weighing less than 110 lb (50 kg). It should not be used unless all other agents are contraindicated or ineffective. It should not be reapplied in any situation.9
In 2009, the first prescription suffocation treatment, a nonovicidal benzyl alcohol 5% lotion (Ulesfia), was approved by the FDA. This product prevents lice from closing their respiratory spiracles, which causes permanent obstruction and results in death.10 Benzyl alcohol appears to be comparable in effectiveness to pyrethrins/piperonyl butoxide.11
In early 2011, the FDA approved a pediculicidal topical suspension agent, spinosad 0.9% (Natroba), which provokes hyperexcitation and eventual death by paralysis.12 In two comparative trials, spinosad was found to have approximately twice the eradication rate of permethrin at 14 days (85 and 84 percent, compared with 45 and 43 percent).13 Spinosad has shown effectiveness (without nit combing) after a single treatment (93 percent eradication versus 62 percent eradication with permethrin); it may be beneficial in patients not adherent to other therapies.13
Ivermectin (Stromectol) is an oral anti-parasitic that has demonstrated effectiveness in clinical trials, but is not FDA-approved for the treatment of pediculosis. A trial of 812 patients older than two years compared ivermectin (400 mcg per kg) with malathion 0.5% lotion in patients with lice that are resistant to malathion or pyrethroid-based products. The results showed that 95 percent of patients taking ivermectin were lice-free at day 15, compared with 85 percent of patients using malathion. The authors suggest that ivermectin may be an appropriate second-line therapy when resistance to topical treatments is documented.14 No difference in adverse effects was noted between the groups.
NONPHARMACOLOGIC TREATMENT (HEAD LICE)
Wet combing involves moistening the hair with commercially available leave-in conditioner and systematically combing the hair from root to tip with a lice comb. Wet combing alone for treating pediculosis does not have adverse effects, and often is preferred by parents wanting to avoid a chemical treatment; however, it can be time consuming depending on hair length and thickness. Combing should be done every three days for two weeks. Cure rates vary considerably (47 to 75 percent), but may be improved by increasing the duration of combing to 24 days.15
Delivery of hot air to kill lice by desiccation has been attempted by numerous investigators with mixed results. Research is ongoing on this minimally invasive treatment option.16
Cetaphil Gentle Skin Cleanser has been studied as a dry-on, suffocation-based pediculicide lotion with a demonstrated eradication rate of 95 percent, although there is question about the design and rigor of the study.17 The recommended protocol involves applying the lotion to the scalp thoroughly and waiting two minutes before combing out all lotion, drying the hair with a hand-held hair dryer, and waiting a minimum of eight hours before shampooing with regular shampoo.
PHARMACOLOGIC TREATMENT (BODY AND PUBIC LICE)
Treatment of pubic lice is similar to that of head lice. The 2010 guidelines from the Centers for Disease Control and Prevention (CDC) on sexually transmitted diseases recommend permethrin 1% or pyrethrins 0.3%/piperonyl butoxide 4% as first-line agents, and alternative regimens of malathion 0.5% lotion or oral ivermectin at 250 mcg per kg, repeated in two weeks.18 The mainstay of treatment for body lice is laundering clothing and bedding in hot water, and regular bathing. A pediculicide is not always necessary.19
Scabies
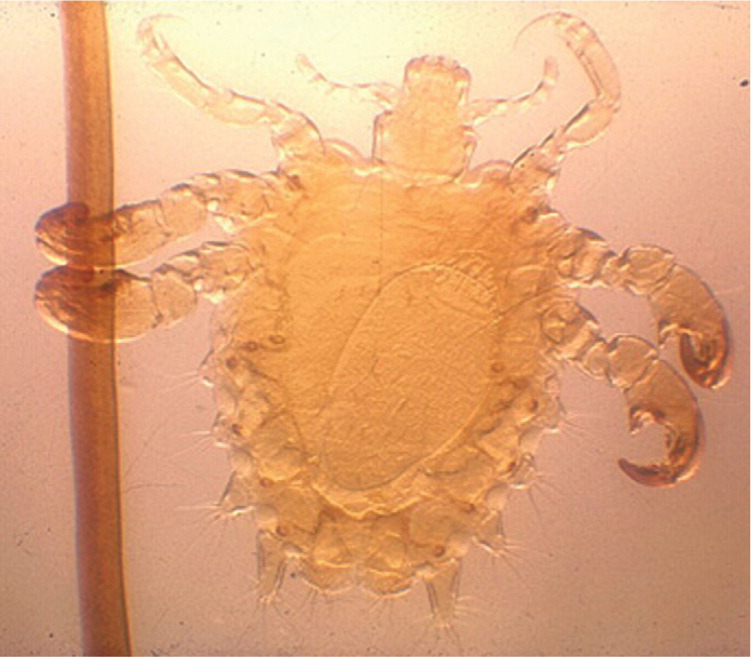
Scabies is a common public health problem, affecting approximately 300 million persons worldwide.20 It is caused by the mite Sarcoptes scabiei var hominis. The arthropod is an ovoid organism. The female is approximately 0.4 mm in size and the male is one-half this size. After mating on the skin surface, the male mite dies and the female mite begins to burrow under the skin, where she lays eggs for four to six weeks.21 Egg production occurs at a rate of one to three eggs per day; eggs hatch after three to four days, and then the new mites cut through the burrow to the skin surface to multiply.22
Female mites can travel up to 2.5 cm per minute,21 but they do not jump or fly. After exposure, mites can penetrate the epidermis within 30 minutes.23 Transmission occurs via direct skin-to-skin contact. A person with conventional scabies needs about 15 to 20 minutes of close contact to transfer the mite to another person.24 Fomite transmission is rare, so general contact precautions should be sufficient to prevent transmission.25,26
Although scabies is more common in young children, other predisposing factors include overcrowding, poor hygiene, poor nutritional status, homelessness, dementia, and sexual contact.27
CLINICAL PRESENTATION
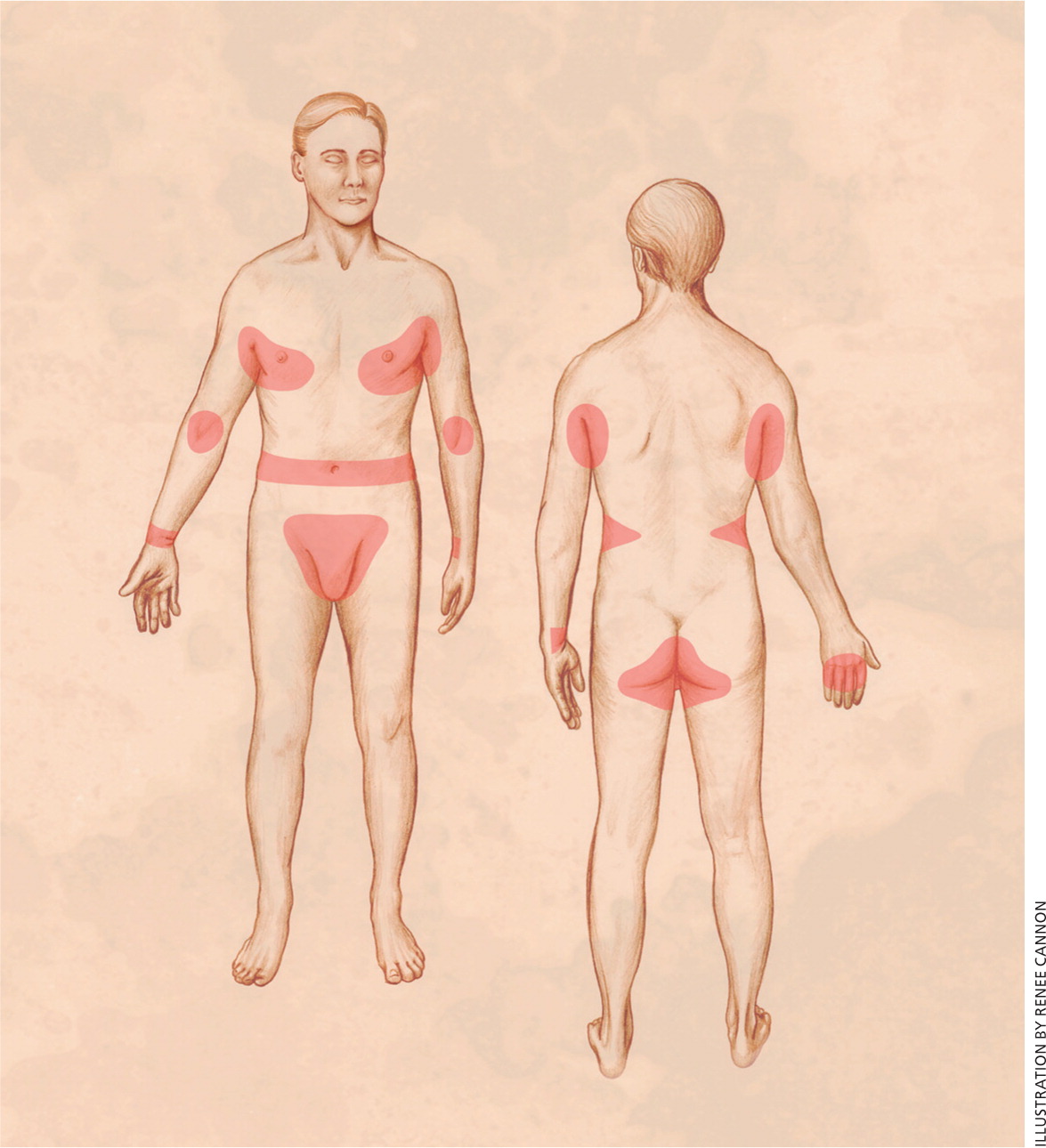
Persons with scabies typically present with an intense and generalized pruritic rash that is worse at night, with the face and neck unaffected. The primary skin lesions are inflammatory pruritic papules, pustules, vesicles, and nodules. The pathognomonic finding is a burrow, which may not always be evident. These are most commonly found on the hands and feet or in the finger webs, and appear as short, wavy, scaly gray lines on the skin surface.21 Nonspecific secondary skin findings may be excoriations, eczematization, and pyoderma. The characteristic body distribution of lesions in adults is illustrated in Figure 3.4 Infants may present with pustules on the palms and soles of the feet, and vesicles or lesions on the neck and face28 (Figure 4).

Crusted scabies (also called Norwegian scabies) is an extremely contagious atypical form of scabies occurring primarily in patients who are older, immunocompromised, or living in close quarters. Patients may present with thick, crusted lesions on the hands and feet, nail abnormalities, generalized erythematous scaling eruptions, and scalp involvement. Because pruritus is mild or absent in this form, scabies is often misdiagnosed, leading to large nosocomial outbreaks.28 In a typical case of scabies, 10 to 15 mites may be present. In crusted scabies, thousands of mites may be present, and the risk of transfer is greater.
DIAGNOSIS
Scabies may be diagnosed with a history of pruritus, rash in the typical distribution, and history of itching in close contacts. Finding mites, eggs, or fecal pellets provides definitive diagnosis. The most common method of examination for mites is skin scraping. Scrapings should be taken from nonexcoriated burrows, papules, or vesicles by applying a drop of mineral oil to the skin, scraping laterally across the lesion using a scalpel, and transferring the oil and skin scraping to a slide. A positive test result reveals mites, eggs, or fecal pellets (Figure 5).

TREATMENT
In contrast to lice, there are fewer randomized controlled trials of products to treat scabies. Most studies were conducted using lindane as the comparator. There is no clear evidence of resistance to permethrin 5% cream for classic scabies, despite heavy use over the previous two decades, and it remains the first-line treatment.18 Physicians should educate patients on correct application of permethrin cream, reminding them that the cream should be applied to all areas of the body from the neck down, kept on overnight or for eight to 14 hours, washed off, and reapplied in one week. Patients should be educated that they may continue to have itching for up to two weeks, even after appropriate and effective treatment. There is evidence for empiric treatment if a patient presents with pruritus and lesions typical of scabies in at least two body sites, or if there are others in the patient's household with pruritus.29,30
A single dose of oral ivermectin at 200 mcg per kg and repeated at day 14 also is considered an option for first-line treatment of classic scabies by the CDC, although cost and availability often relegate it to second-line therapy if treatment with topical permethrin is unsuccessful.18
Environmental control measures for scabies include washing sheets and clothing at 140°F (60°C) and drying in a hot dryer. For items that cannot be machine washed, isolation in a plastic bag for at least 72 hours is sufficient. Other environmental measures such as pesticide sprays or powders are not recommended. Vacuuming may be helpful, although there is little direct evidence of benefit.
Crusted scabies represents a treatment challenge. It often is longstanding because of misdiagnosis. Clinical trials are limited. The CDC recommends dual therapy with ivermectin at 200 mcg per kg orally on days 1, 2, 8, 9, and 15, plus permethrin 5% cream full-body application daily for seven days, then twice weekly until demonstrated cure.18,30 Environmental control measures in affected institutions include patient isolation until dual therapy is completed, barrier precautions with gloves, and screening and treatment of infected caregivers and close contacts.
Data Sources: A PubMed search was conducted in Clinical Queries using the key terms lice and scabies, and using the limits human and English. The search included meta-analyses, randomized controlled trials, clinical trials, guidelines, and reviews. Also searched were the Cochrane Database of Systematic Reviews, the National Guideline Clearinghouse Database, UpToDate, and DynaMed. Search dates: May 2010, October 2010, and April 20, 2011.
