
Am Fam Physician. 2019;99(10):635-642
Patient information: See related handout on lice and scabies, written by the authors of this article.
Author disclosure: No relevant financial affiliations.
Pediculosis and scabies are caused by ectoparasites. Pruritus is the most common presenting symptom. Head and pubic lice infestations are diagnosed with visualization of live lice. Nits (lice eggs or egg casings) alone are not sufficient to diagnose a current infestation. A “no-nit” policy for return to school is not recommended because nits can remain even after successful treatment. First-line pharmacologic treatment for pediculosis is permethrin 1% lotion or shampoo. Newer treatments are available but costly, and resistance patterns are generally unknown. Noninsecticidal agents, including dimethicone and isopropyl myristate, show promise in the treatment of pediculosis. Extensive environmental decontamination is not necessary after pediculosis is diagnosed. In adults, the presence of pubic lice should prompt an evaluation for sexually transmitted infections. Body lice infestation should be suspected in patients with pruritus who live in crowded conditions or have poor hygiene. Scabies in adults presents as a pruritic, papular rash in a typical distribution pattern. In infants, the rash can also be vesicular, pustular, or nodular. First-line treatment for scabies is permethrin 5% cream. Clothing and bedding of persons with scabies should be washed in hot water and dried in a hot dryer. Counseling regarding appropriate diagnosis and correct use of effective therapies is key to reducing the burden of lice and scabies.
Pediculosis and scabies are caused by ectoparasites. Pruritus is the most common presenting symptom with both conditions. Determining the specific etiology of pruritus based on history and physical examination findings is important. Lice in particular may be overdiagnosed by anxious patients and treated using over-the-counter medications without an office evaluation.1 Seeking an appropriate clinical diagnosis may help reduce treatment-resistant lice. Although the diagnosis of pediculosis and scabies has not changed substantially, there are new developments in treatment since this topic was previously covered in American Family Physician.2–4
| Clinical recommendation | Evidence rating | References | Comment |
|---|---|---|---|
| A “no-nit” policy is not recommended for schools and day cares because nits alone do not indicate an active infestation. Children should not be kept out of school during treatment, even with active infestation, because the likelihood of transmission is low, and this can result in significant absences. | C | 1, 8 | U.S. and Canadian consensus guidelines based on basic knowledge of the lice life cycle |
| Permethrin 1% lotion or shampoo (Nix) is first-line treatment for pediculosis. Alternative treatments should not be used unless permethrin fails after two treatments. | C | 1, 8 | U.S. consensus guidelines balancing effectiveness and toxicity |
| Nonovicidal therapies for pediculosis should be applied twice, seven to 10 days apart, to fully eradicate lice. Some authors postulate that three treatments with permethrin or pyrethrins might be most effective. | C | 1, 8, 19, 20 | U.S. and Canadian consensus guidelines based on basic knowledge of the lice life cycle Inappropriate retreatment may result in resistance and lack of treatment effectiveness |
| Scabies should be considered in patients with a pruritic, papular rash in the typical distribution and pruritus in close contacts. The classic burrows in webs and creases may not be present. | C | 27, 29–31 | U.S. and European consensus guidelines based on epidemiologic data and case studies |
| Oral ivermectin (Stromectol) should be reserved for patients with scabies who do not improve with permethrin 5% cream (Elimite). | C | 10, 31 | Guidelines using consensus agreement in area of little clinical research |
Pediculosis
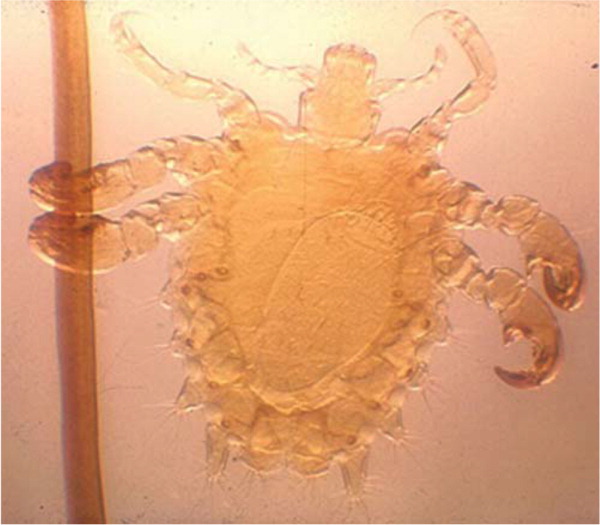
Lice are obligate, blood-sucking parasites that can infest the human head (Pediculus humanus capitis; Figure 13), body (Pediculus humanus corporis), and pubic region (Phthirus pubis; Figure 2). Body and head lice are approximately 1 to 3 mm long, about the size of a sesame seed, and are flattened dorsoventrally. The pubic louse is much shorter. Because lice cannot jump or fly, transmission requires close contact.5 The female louse can survive for up to one month on the scalp and lay up to eight to 10 eggs per day at the skin-hair junction. The eggs hatch and mature into adults in 20 days.1 Viable eggs may be difficult to see but can be found attached to the base of hairs. The yellow to white empty egg casings are easier to visualize.

CLINICAL PRESENTATION
The pruritus associated with pediculosis is a delayed hypersensitivity reaction, which may take four to six weeks to develop after the first exposure, with future exposures resulting in pruritus within one to two days.1 Intense pruritus leads to scratching, with subsequent excoriations and possible secondary cellulitis.
DIAGNOSIS
Head lice infestation is diagnosed by finding at least one live louse on visual inspection.1 Visualization can be improved by using a bright light and magnifying lens, and by combing the hair with a lice comb (fine-toothed comb available at most drug stores that is also known as a nit comb) and examining the comb teeth.6 Lice are commonly found behind the ears and on the back of the neck. When lice are found in one family member, the entire family should be examined.
Physicians should not initiate therapy unless live lice are observed. Finding only nits (lice eggs) on examination does not indicate current infestation. One prospective study found that of 91 school-aged children with live lice and/or nits, only 18% of those with nits alone and no live lice developed an active lice infestation during 14 days of observation.7 Nits may remain on the hair for months after successful treatment and can be confused with dandruff, hair spray debris, or dirt particles. The American Academy of Pediatrics does not recommend “no-nit” policies at schools and day cares because nits alone do not indicate an active infestation. Children should not be kept out of school during treatment, even with active infestation, because the likelihood of transmission is low, and this can result in significant absences.1,8
Body lice should be suspected in patients with pruritus who live in crowded conditions or have poor hygiene. Because body lice lay their eggs in cloth fibers, diagnosis is confirmed with identification of body lice or nits in the seams of clothing.5 If pubic lice or nits are identified, the patient should be evaluated for sexually transmitted infections.9,10
PHARMACOLOGIC TREATMENT OF HEAD LICE
Pharmacologic treatment of head lice infestation is focused on three general mechanisms: neurotoxicity resulting in paralysis of the lice (insecticidal treatments), suffocation via “coating” the lice, or dissolution of the wax covering on the exoskeleton4 (Table 11,2,4,8,11–17). Insecticidal agents that are neurotoxic to lice include permethrin 1% lotion or shampoo (Nix), pyrethrins 0.3%/piperonyl butoxide 4% shampoo (Rid), malathion 0.5% lotion (Ovide), spinosad 0.9% suspension (Natroba), ivermectin 0.5% lotion (Sklice), and oral ivermectin (Stromectol; off-label use). Permethrin 1% is recommended as first-line treatment for head lice.1,8,18
| Treatment | Ovicidal? | Mechanism of action | Directions (per package inserts) | Effectiveness | Cost* | Comments |
|---|---|---|---|---|---|---|
| Benzyl alcohol 5% lotion (Ulesfia); prescription | No | Suffocation | Apply to dry hair, leave on for 10 minutes then rinse; repeat in seven days | 75% to 76% of patients are lice free at 14 days11 | — ($450) for two bottles | Can be costly for long hair (dosing is based on hair length) Must be used in conjunction with a lice comb (also called nit comb) Approved for persons six months and older, may be used in pregnant and lactating women |
| Dimethicone solution (Nix Ultra, Lice MD); OTC | No | Suffocation | Spray all over dry hair, and massage until wet; let it sit for 30 minutes, then comb into hair; leave on overnight; wash out, and use a lice comb; repeat in eight to 10 days | 70% to 96% of patients are lice free at 14 days (study of dimethicone 100%)12,13 | — ($10 to $20) for one bottle | May cause eye irritation Should not be used in children younger than two years |
| Isopropyl myristate (Resultz); OTC† | No | Exoskeleton dissolution | Apply to dry hair and scalp, leave on for 10 minutes then rinse with warm water; repeat in eight to 10 days | 54% to 82% of patients are lice free at 14 to 21 days12 | — | May cause local and eye irritation Not recommended for children younger than four years |
| Ivermectin 0.5% lotion (Sklice); prescription | Not directly, but lice hatched from treated eggs die within 48 hours | Neurotoxic to lice4 | Apply to dry hair and scalp, leave on for 10 minutes then rinse; one application is sufficient | 74% of patients are lice free at 15 days14 | — ($360) for one tube | Rare adverse effects include skin and eye irritation, erythema, burning, dryness |
| Ivermectin, oral (Stromectol); prescription‡ | Partial | Neurotoxic to lice | 200 mcg per kg, two doses seven to 10 days apart8 | 92% to 97% of patients are lice free at 14 to 15 days after two doses15 | $5 ($8) for one 3-mg tablet (dosing varies based on weight) | Do not use in children weighing less than 33 lb (15 kg) or in pregnant women |
| Malathion 0.5% lotion (Ovide); prescription | Partial | Neurotoxic to lice | Apply to dry hair until hair and scalp are wet, allow to dry naturally, shampoo eight to 12 hours later, rinse and use a lice comb; repeat after seven to nine days only if live lice are still present | 80% of patients are lice free at 14 days16 | $150 ($270) for one bottle | Flammable; do not use with a hair dryer or near cigarettes or an open flame |
| Permethrin 1% shampoo (Nix); OTC | No | Neurotoxic to lice | Apply to damp hair, leave on for 10 minutes then rinse; repeat in seven days | 50% to 97% of patients are lice free at 14 days1,8,17 | $20 for two treatments | First-line treatment1 |
| Pyrethrins 0.3%/piperonyl butoxide 4% shampoo or mousse (Rid); OTC | No | Neurotoxic to lice | Apply to dry hair, leave on for 10 minutes then rinse; repeat in seven days | 62% to 94% of patients are lice free (unclear time frame)1 | — ($15 to $20) for two treatments | Piperonyl butoxide is thought to prolong the activity of pyrethrins Avoid in patients with chrysanthemum allergy |
| Spinosad 0.9% suspension (Natroba); prescription | Yes | Neurotoxic to lice | Apply to dry hair, leave on for 10 minutes then rinse; repeat in seven days only if live lice are present | 68% to 87% of patients are lice free at 14 days16 | $200 ($280) for one bottle | May be used without a lice comb, although use of a lice comb improves results Safe for use in children four years and older Do not use in infants younger than six months because it contains benzyl alcohol |
Noninsecticidal agents that rely on suffocation or exoskeleton dissolution include benzyl alcohol 5% lotion (Ulesfia), dimethicone solution (Nix Ultra, Lice MD), and isopropyl myristate solution (Resultz; approved by the U.S. Food and Drug Administration in May 2017 but not yet marketed in the United States). The Canadian Paediatric Society recommends dimethicone solution and isopropyl myristate solution as second-line agents if permethrin fails after two treatments.8
A key to formulating an effective treatment regimen is recognizing the effectiveness of available treatments in destroying viable eggs because this dictates if retreatment is necessary. Malathion, spinosad, and topical ivermectin are considered ovicidal, and they will kill both live lice and eggs in one treatment. Nonovicidal agents (permethrin, pyrethrins, benzyl alcohol, dimethicone, oral ivermectin, and isopropyl myristate) typically require a repeat application for complete eradication. Timing for nonovicidal treatments is based on the life cycle of the louse.19 An initial application followed by a second application seven to 10 days later (nine days is optimal) should be sufficient to eradicate most lice. Some authors have postulated that the most effective retreatment schedule for permethrin or pyrethrins might be three doses, on days 0, 7, and 13 to 15.1,20
Resistance to permethrin and pyrethrins/piperonyl butoxide can be significant, although the geographic distribution of resistant lice is not well-known.17 Pseudoresistance may be due to poor adherence, incorrect product use (underdosing or not following directions), and reinfestation. After trials of two appropriately administered courses of permethrin, an alternative agent should be used.8
NONPHARMACOLOGIC TREATMENT OF HEAD LICE
Wet combing for the treatment of head lice involves washing with ordinary shampoo, moistening the hair with commercially available leave-in conditioner, combing with a wide-tooth comb until detangled, and then systematically combing the hair from root to tip with a lice comb. The conditioner should then be rinsed out and the hair combed with a lice comb again.21 Wet combing alone does not have adverse effects and is often preferred by parents wanting to avoid a chemical treatment; however, it can be time-consuming. Wet combing should be done every three days until no lice are detected on four to five consecutive occasions. Cure rates vary considerably (47% to 75%), although studies are not high quality.22,23
Several substances, including vinegar, formic acid solution, nit-removal conditioners, water, regular conditioner, and almond oil, have been evaluated as methods to remove nits by loosening the nit from the hair shaft.23 Water and regular conditioner were the most effective in the removal of nits in an in vitro study.23 Use of herbal and alternative products (e.g., tea tree oil, eucalyptus oil) is not recommended in children because their safety and efficacy have not been evaluated by the U.S. Food and Drug Administration, and evidence of benefit is limited.1,12
Head-to-head contact is the most prevalent form of lice transmission. Fomite transmission is a common misconception. Although fomite transmission is rare, items that have come into direct contact with the head (e.g., pillowcases, hats, clothing) within the two days before treatment should be washed. Bringing the items to a temperature of at least 130°F (54°C) in the washing machine or dryer can effectively eradicate the lice.1 Placing items in a sealed plastic bag for two weeks is also effective. Sprays, carpet treatments, and other chemical environmental decontamination measures should not be used.1
TREATMENT OF PUBIC AND BODY LICE
Treatment of pubic lice is similar to that of head lice. The Centers for Disease Control and Prevention recommends permethrin 1% lotion or pyrethrins 0.3%/piperonyl butoxide 4% shampoo as the first-line agent, and malathion 0.5% lotion or oral ivermectin as an alternative.10 The Centers for Disease Control and Prevention recommends treating sex partners from the previous month, although European guidelines recommend treating partners from the previous three months.9,10 The mainstay of treatment for body lice involves laundering clothing and bedding in hot water and bathing regularly.
Scabies
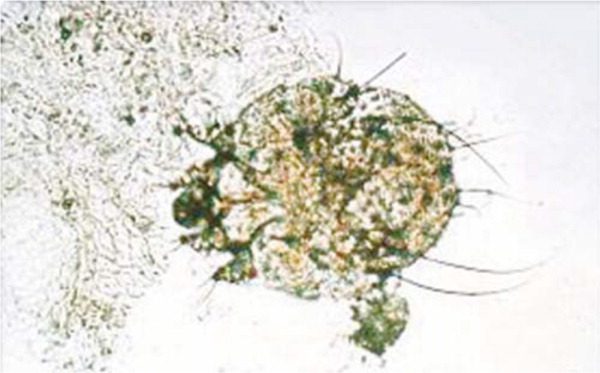
Scabies is a common public health problem affecting approximately 100 million persons annually.24 It is caused by the Sarcoptes scabiei mite (Figure 3). The female mite is approximately 0.4 mm in size. After mating on the skin surface, the male mite dies, and the female burrows under the skin where she lays eggs for four to six weeks.25,26 Egg production occurs at a rate of one to three eggs daily, and larvae emerge two to three days after the eggs are laid. The larvae reach maturity in about two weeks, and the new mites cut through the burrow to the skin surface to mate and multiply.25,26 With the first infestation, symptoms may not develop for up to six weeks because there is a delay in the hypersensitivity reaction to mite feces, during which time household contacts may become infected. Symptoms occur more quickly with reinfestations.25
Female scabies mites can travel up to 2.5 cm per minute, but they do not jump or fly.25 After exposure, mites can penetrate the epidermis within 30 minutes. Transmission typically occurs via direct skin-to-skin contact, but there is evidence that mites can survive for days after leaving human skin and be transmitted via fomites (e.g., clothing, linens, towels).27 About 15 to 20 minutes of close contact is needed to transfer the mite from one person to another.28 Risk factors for scabies infestation include overcrowded living conditions, poor hygiene, poor nutritional status, homelessness, dementia, sexual contact, and living in a tropical region.24,26
CLINICAL PRESENTATION
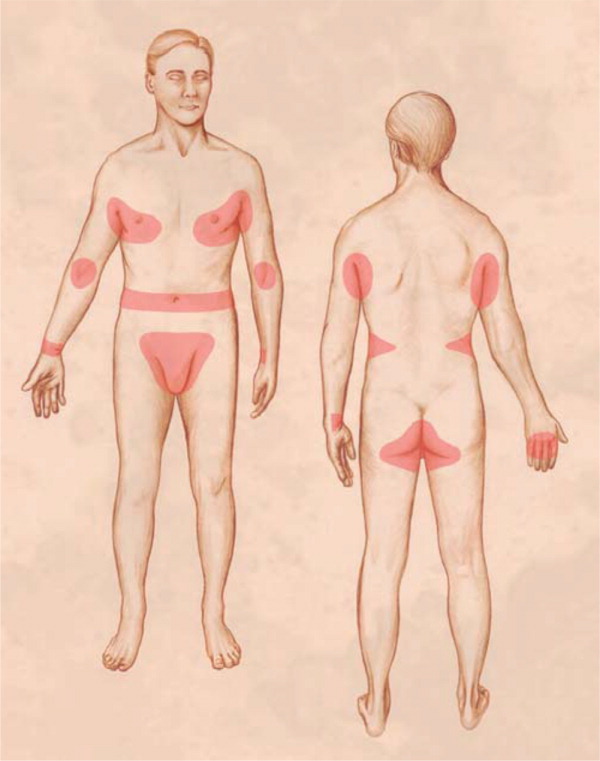
Persons with scabies typically present with intense, generalized pruritus that is worse at night. The face and neck are unaffected. The primary skin lesions are erythematous, pruritic papules, pustules, vesicles, and nodules. The pathognomonic finding is a burrow (Figure 4), which is not always evident. The lesions are most commonly found on the finger webs, wrist flexors, elbows, axillae, buttocks, genitalia, and breasts.25,26 Nonspecific secondary skin findings may include excoriations, eczematization, and pyoderma. The characteristic distribution of lesions in adults with scabies is illustrated in Figure 5.3 Infants may present with pustules on the palms and soles and vesicles or other lesions on the neck and face.25,26

DIAGNOSIS
Scabies should be considered in patients with a history of a pruritic, papular rash in the typical distribution and pruritus in close contacts.27,29–31 Finding mites, eggs, or fecal pellets using microscopy confirms the diagnosis. Evaluation of a skin scraping is the diagnostic standard for detecting mites.32 A skin scraping suspended in oil allows for microscopic identification of mites, eggs, and fecal pellets; however, dermoscopy has fewer false negatives and may be preferable.26,32
A recent study showed that scabies is misdiagnosed in 45% of cases, highlighting the need for improved clinician education and diagnostic methods.32 Misdiagnosis may be due to reliance on history and physical examination findings alone rather than using microscopy, although there is evidence supporting empiric treatment if a patient presents with pruritus and he or she has lesions typical of scabies on at least two body sites or other household members also have pruritus.27,30 The differential diagnosis of scabies is presented in Table 2.5,32
| Contact dermatitis |
| Eczema |
| Folliculitis |
| Impetigo |
| Insect bites (mosquitoes, fleas, bedbugs) |
| Irritant dermatitis |
| Tinea |
TREATMENT OF SCABIES
Permethrin 5% cream (Elimite) is the first-line treatment for scabies.29 Physicians should educate their patients about correct application of permethrin cream, reminding them that it should be applied to all areas of the body from the neck down, remain on the skin for eight to 14 hours or overnight, washed off, and reapplied in one week. Patients should be told that they may continue to itch for up to two weeks, even after appropriate and effective treatment. Persistent posttreatment symptoms should prompt consideration of misdiagnosis, treatment failure, or treatment-related skin irritation.25,32 Sex partners from the past two months should be treated.10,31
Environmental control measures for scabies include washing items such as sheets and clothing at a temperature of at least 122°F (50°C) and drying in a hot dryer. For items that cannot be machine washed, isolation in a sealed plastic bag for at least one week is sufficient.31
This article updates previous articles on this topic by Gunning, et al.2 and by Flinders and De Schweinitz.3
Data Sources: A PubMed search was conducted in Clinical Queries using the key terms lice and scabies, with the limits human and English. The search included Essential Evidence Plus, meta-analyses, randomized controlled trials, clinical trials, guidelines, and reviews. Also searched were the Cochrane database, the National Guideline Clearinghouse, UpToDate, and DynaMed. Search dates: December 2017, March 2018, and May 2018.
