A more recent article on seborrheic dermatitis is available.
Am Fam Physician. 2015;91(3):185-190
Author disclosure: No relevant financial affiliations.
Seborrheic dermatitis is a common skin condition in infants, adolescents, and adults. The characteristic symptoms—scaling, erythema, and itching—occur most often on the scalp, face, chest, back, axilla, and groin. Seborrheic dermatitis is a clinical diagnosis based on the location and appearance of the lesions. The skin changes are thought to result from an inflammatory response to a common skin organism, Malassezia yeast. Treatment with antifungal agents such as topical ketoconazole is the mainstay of therapy for seborrheic dermatitis of the face and body. Because of possible adverse effects, anti-inflammatory agents such as topical corticosteroids and calcineurin inhibitors should be used only for short durations. Several over-the-counter shampoos are available for treatment of seborrheic dermatitis of the scalp, and patients should be directed to initiate therapy with one of these agents. Antifungal shampoos (long-term) and topical corticosteroids (short-term) can be used as second-line agents for treatment of scalp seborrheic dermatitis.
Seborrheic dermatitis is a chronic inflammatory dermatologic condition that usually appears on areas of the body with a large density of sebaceous glands, such as the scalp, face, chest, back, axilla, and groin. Although it can be associated with human immunodeficiency virus infection and neurologic disease (e.g., cerebrovascular event, Parkinson disease),1 seborrheic dermatitis typically occurs in healthy persons. Its prevalence is 1% to 3% in the general population and 34% to 83% in immunocompromised persons.2 It has a bimodal distribution, with peaks at two to 12 months of age and in adolescence and early adulthood.2 It is more common in men and is typically more severe in cold and dry climates and during periods of increased stress.3
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Topical antifungal agents are the first-line therapy for acute and long-term treatment of seborrheic dermatitis of the face and body. | A | 3, 14–16, 22–26 |
| Topical corticosteroids are effective in treating seborrheic dermatitis and should be used sparingly to avoid adverse effects. | A | 2, 18, 19, 22, 26, 28, 29, 32 |
| Topical calcineurin inhibitors are effective, well-tolerated second-line treatments for seborrheic dermatitis, but they are not approved by the U.S. Food and Drug Administration for this use. | A | 27–35 |
Diagnosis
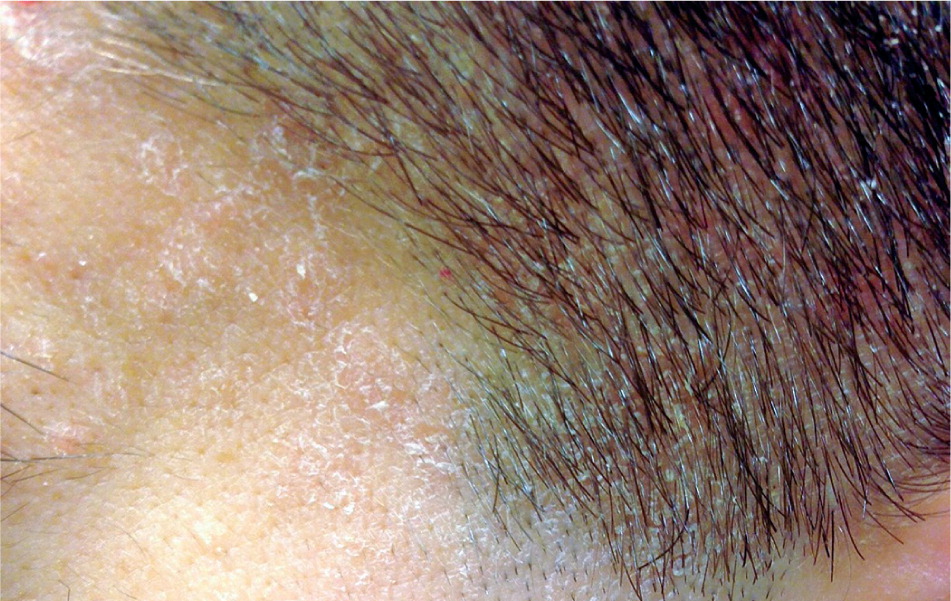
Seborrheic dermatitis is a clinical diagnosis based on the location and appearance of lesions. In infants, it may present as thick white or yellow greasy scales on the scalp; it is usually benign and resolves spontaneously. In adolescents and adults, seborrheic dermatitis typically presents as flaky, greasy, erythematous patches on the scalp (Figure 1), nasolabial folds (Figure 2), ears, eyebrows (Figures 3 and 4), anterior chest, or upper back.3 The differential diagnosis is lengthy (Table 12,4 ), but the correct diagnosis can usually be made clinically by the characteristic distribution of lesions and varying course of the disease.5 If the diagnosis is uncertain, a biopsy demonstrating parakeratosis in the epidermis, plugged follicular ostia, and spongiosis can confirm the presence of seborrheic dermatitis. The diagnosis can be challenging in patients with darker skin, but the same principles apply.



| Condition | Distinguishing features |
|---|---|
| Atopic dermatitis | Flexural lichenification in adults; facial and extensor involvement in infants and children |
| Candidiasis | Typically confined to mucous membranes and intertriginous regions |
| Contact dermatitis | Characteristic distribution patterns from irritant or allergen |
| Erythrasma | Brown-red, scaly eruption of toe webs, groin, and axillae |
| Impetigo | Superficial skin infection caused by streptococci and/or staphylococci; begins as vesicles with thin, fragile roof |
| Lichen simplex chronicus | Eczematous eruption caused by habitual scratching of single localized area; more common in adults, but possible in children |
| Nummular dermatitis | One or several coin-shaped plaques on extremities, typically on backs of hands |
| Pityriasis rosea | Begins with herald patch; “Christmas-tree distribution” of salmon pink papules over trunk and proximal extremities |
| Psoriasis | Distinctive red, scaling papules that coalesce to form round-to-oval plaques |
| Rosacea | Erythematous, edematous eruptions of papules and pustules on forehead, cheeks, nose, and eyes |
| Secondary syphilis | Copper-colored scaly plaques on palms and soles accompanied by an influenza-like syndrome and generalized adenopathy |
| Systemic lupus erythematosus | Discoid: disk-like lesions on face and scalp; subacute: photo-distribution papulosquamous, annular lesions over trunk; acute: photo-distribution red plaques forming facial butterfly rash; infants: appears in first month of life; papulosquamous, annular lesions |
| Tinea capitis, corporis | Dermatophyte infection of the scalp or body; leading edge (active border) scaly, red, and slightly elevated with central clearing; vesicles appear at active border when inflammation is intense; classic “ringworm pattern” |
Pathophysiology
Although the pathophysiology of seborrheic dermatitis is not completely understood, the mechanisms of effective therapies coupled with results of recent biomolecular studies provide clues about the causes. The redness, itching, and scaling associated with seborrheic dermatitis are caused by changes in skin cell functioning.6,7 Malassezia yeast seems to cause a nonspecific immune response that begins the cascade of skin changes that occur in seborrheic dermatitis.6 Malassezia is a normal component of skin flora, but in persons with seborrheic dermatitis, the yeast invade the stratum corneum, releasing lipases that result in free fatty acid formation and cause the inflammatory process to begin.8 Malassezia thrive in high-lipid environments, so the presence of free fatty acids enhances the growth of the yeast. The inflammation causes stratum corneum hyperproliferation (scaling) and incomplete corneocyte differentiation, which alters the stratum corneum barrier and impairs its function, thus increasing access for Malassezia and allowing water to more readily leave the cells.8
Based on the current understanding of the pathophysiology of the condition, the treatments for seborrheic dermatitis make biologic sense. Keratolytics (sulfur and salicylic acid) help remove the outer layers of the hyper-proliferating stratum corneum.9 Coal tar is thought to decrease the rate of stratum corneum production.9 Antifungals decrease the Malassezia population, whereas anti-inflammatories such as corticosteroids and calcineurin inhibitors decrease the inflammatory response. Many of the current treatments for seborrheic dermatitis have multiple effects (antifungal, anti-inflammatory, regulation of stratum corneum production), thereby combatting the skin changes on multiple levels. The severity of symptoms can be affected by stress and sun exposure, and often has a variable course despite treatment.
Treatment
The treatment of infantile seborrheic dermatitis consists primarily of emollients that help loosen scales (e.g., mineral or olive oil, petroleum jelly). Scales can then be removed by rubbing with a cloth or infant hair brush.10,11 One study showed that ketoconazole 1% to 2% cream is effective and seems to be safe when used twice daily for two weeks.12 There are no shampoos that have been approved by the U.S. Food and Drug Administration for treatment of seborrheic dermatitis in children younger than two years.
Treatment of seborrheic dermatitis in adolescents is identical to that in adults11; the primary goals are to lessen the visible signs of the condition and to reduce pruritus and erythema. Treatment includes over-the-counter shampoos and topical antifungals, calcineurin inhibitors, and corticosteroids (Tables 2 and 3).2,3,5,8,9,13–32 Because seborrheic dermatitis is a chronic condition, ongoing maintenance therapy is often necessary.2,9
| Product | Dosing frequency | Common adverse effects | Cost for generic (brand)* |
|---|---|---|---|
| Over-the-counter preparations | |||
| Coal tar shampoo | Twice per week | Contact dermatitis, folliculitis, photosensitivity | $5 for 130 mL |
| Selenium sulfide shampoo | Twice per week | Alopecia, hair discoloration, irritation | $7 for 325 mL |
| Tea tree oil shampoo | Daily | Allergic contact dermatitis, irritation | $14 for 473 mL |
| Zinc pyrithione shampoo | Twice per week | Irritation | $5 for 420 mL |
| Topical antifungals | |||
| Ciclopirox 1% shampoo (Loprox) | Daily initially, then twice per week | Burning, contact dermatitis, pruritus | $59 ($527) for 120 mL |
| Ketoconazole 2% shampoo (Nizoral) | Daily initially, then twice per week | Irritation, pruritus, xeroderma | $16 ($63) for 120 mL |
| Topical corticosteroids | |||
| Betamethasone valerate 0.12% foam (Luxiq) | Twice daily | Hypopigmentation, pruritus, skin atrophy, stinging | $88 ($274) for 50 g |
| Clobetasol 0.05% shampoo (Clobex), alternating with ketoconazole 2% shampoo | Each twice weekly, alternating medications, for up to two weeks | Burning, erythema, folliculitis, hypopigmentation, pruritus, skin atrophy | $144 ($644) for 118 mL |
| Fluocinolone 0.01% shampoo (Capex) | Daily | Burning, dryness, hypopigmentation, skin atrophy | NA ($364 for 120 mL) |
| Fluocinolone 0.01% solution (Synalar) | Once or twice daily | Burning, cough, fever, hypopigmentation, pruritus, rhinorrhea, skin atrophy | $32 ($289) for 60 mL |
| Product | Dosing frequency | Common adverse effects | Cost for generic (brand)* |
|---|---|---|---|
| Topical antifungals | |||
| Ciclopirox 0.77% gel or cream (Ciclodan) | Twice daily for up to four weeks | Burning, contact dermatitis, pruritus | $58 ($58) for 90-g tube of cream, $36 for 30-g tube of gel |
| Ketoconazole 2% cream, foam (Extina), or gel (Xolegel) | Twice daily for eight weeks, then as needed | Burning, irritation, photosensitivity | $15 for 30-g tube of cream ($355 for 50-g can of Extina, $495 for 45-g tube of Xolegel) |
| Sertaconazole 2% cream (Ertaczo) | Twice daily for up to four weeks | Contact dermatitis, tenderness, xeroderma | NA ($423 for 60 g) |
| Topical calcineurin inhibitors† | |||
| Pimecrolimus 1% cream (Elidel) | Twice daily | Burning, headache, upper respiratory infection | NA ($204 for 30 g) |
| Tacrolimus 0.1% ointment (Protopic) | Twice daily | Burning, influenza-like symptoms, pruritus | NA ($234 for 30 g) |
| Topical corticosteroids | |||
| Betamethasone valerate 0.1% cream (Beta-Val) or lotion | Once or twice daily | Hypopigmentation, skin atrophy, stinging, telangiectasia | $13 ($7) for 15-g tube of cream; $25 ($13) for 60-mL bottle of lotion |
| Desonide 0.05% cream, foam (Verdeso), gel (Desonate), lotion (Lokara), or ointment (Desowen) | Once or twice daily | Burning, hypopigmentation, skin atrophy, stinging, upper respiratory symptoms | $15 for 15-g tube of cream; ($295 for 50-g can of Verdeso); ($419 for 60-g tube of Desonate); $73 ($73) for 59-mL bottle of lotion; $13 ($28) for 15-g tube of ointment |
| Fluocinolone 0.01% cream, oil (Derma Smoothe), or solution (Synalar) | Once or twice daily | Burning, cough, dryness, fever, hypopigmentation, irritation, pruritus, rhinorrhea, skin atrophy | $23 for 15-g tube of cream; $84 ($210) for 118-mL bottle of oil; $32 ($289) for 60-mL bottle of solution |
| Hydrocortisone 1% cream or ointment | Once or twice daily | Burning, hypopigmentation, pruritus, skin atrophy | $4 for 28-g tube of cream; $7 for 28-g tube of ointment |
SCALP
For mild seborrheic dermatitis of the scalp, over-the-counter dandruff shampoos containing selenium sulfide, zinc pyrithione, or coal tar can control symptoms at a fraction of the cost of other treatments.8,9,13 Tea tree oil shampoo may also decrease symptoms.9 For long-term control, antifungal shampoos containing ketoconazole 2% (Nizoral)3,14 or ciclopirox 1% (Loprox)15,16 can be used daily or at least two or three times per week for several weeks, until remission is achieved. Once-weekly use of these medicated shampoos can prevent relapse.14–17 These shampoos should remain on the hair for at least five minutes to guarantee adequate exposure to the scalp.9
Depending on the severity of scalp inflammation, topical corticosteroids can be beneficial, but long-term use is associated with adverse effects and can be expensive.2 Fluocinolone 0.01% solution (Synalar) or shampoo (Capex) and betamethasone valerate 0.12% foam (Luxiq) can reduce itching and inflammation.18 For moderate to severe cases, clobetasol 0.05% shampoo (Clobex) twice weekly alternating with ketoconazole 2% shampoo twice weekly can reduce acute symptoms more quickly and maintain control longer after discontinuing use, compared with ketoconazole alone.19
Although some doctors warn their patients that any treatment for scalp seborrheic dermatitis may lose its effectiveness after three months of use, a study evaluating a zinc scalp treatment at six and 11 months showed no loss of effect.20 A study of the long-term use of ketoconazole shampoo for maintenance therapy also showed no degradation in effectiveness over time.21 What may appear to be a worsening of symptoms despite continued use of a treatment may actually represent the natural, varying course of the disease. Often, reassurance and maintenance of therapy are all that is needed, reserving changes in treatment for persistent worsening of symptoms. Patients with symptoms that do not respond to any of the therapies outlined above may benefit from systemic anti-inflammatories and should be referred to a dermatologist.
FACE AND BODY
The mainstays of treatment for facial seborrheic dermatitis are topical antifungals, corticosteroids, and calcineurin inhibitors. Ketoconazole 2% is as effective as hydrocortisone 1% cream.22 Ketoconazole 2% gel (Xolegel) significantly reduced symptoms of erythema, pruritus, and scaling compared with vehicle alone.23 Ciclopirox appears to be better tolerated and more effective than ketoconazole 2% gel.24,25 Ciclopirox 1% cream (not available in the United States) was shown in a randomized, double-blinded trial to greatly reduce symptoms when used as a maintenance medication.24 Sertaconazole 2% cream (Ertaczo) was more effective than hydrocortisone 1% cream in one study.26 In light of their effectiveness, low adverse effect profile, and reasonable cost, topical antifungals are the preferred agents for acute and long-term treatment of seborrheic dermatitis of the face and body.3,14–16,22–26
Low- or mid-potency topical corticosteroids have been successful in reducing symptoms of seborrheic dermatitis and are as effective as antifungal and other anti-inflammatory agents.22,29 Although they are effective and cost significantly less than topical antifungals and calcineurin inhibitors, topical corticosteroids are best used as second-line agents because long-term use has been associated with thinning of the skin and formation of telangiectasia.2,18,19,22,26,28,29,32
Studies have shown that off-label use of topical calcineurin inhibitors can be as effective as topical antifungal and corticosteroid therapy with a lower adverse effect profile.27–32 Pimecrolimus 1% cream (Elidel) provides longer-lasting symptom relief than betamethasone valerate 0.1% cream (Beta-Val).28 Tacrolimus 0.1% ointment (Protopic) may improve symptoms as well as hydrocortisone cream.27 Although pimecrolimus and tacrolimus received a boxed warning from the U.S. Food and Drug Administration because of concerns about a possible association with lymphoma and skin cancer, there is insufficient evidence to support this claim.33,34 As a result, the American Academy of Dermatology recommends that continuous long-term use of topical calcineurin inhibitors be avoided and application limited to the areas of involvement.35 Like topical corticosteroids, these agents are an effective second-line therapy for flares-ups.
Data Sources: Essential Evidence Plus was searched using the keywords dermatitis and seborrheic. Search date: July 29, 2013. Ovid was searched using the keywords cancer risk and topical calcineurin inhibitors. Search date: February 3, 2014. Ovid was searched using the keywords seborrheic dermatitis and microbiology. Search date: February 8, 2014. Ovid was searched using the keywords seborrheic dermatitis, diagnosis of, and classification of. Search date: February 15, 2014. Ovid was searched using the keywords seborrheic dermatitis, and studies were limited to those published January 1, 2013, through September 2014. Search date: October 14, 2014.
The views expressed are those of the authors and do not reflect the official policy of the Department of the Army, the Department of Defense, or the U.S. government.