
Am Fam Physician. 2019;99(12):744-750
Patient information: See related handout on plantar fasciitis, written by the authors of this article.
Author disclosure: No relevant financial affiliations.
Plantar fasciitis is a common problem that one in 10 people will experience in their lifetime. Plantar fasciopathy is an appropriate descriptor because the condition is not inflammatory. Risk factors include limited ankle dorsiflexion, increased body mass index, and standing for prolonged periods of time. Plantar fasciitis is common in runners but can also affect sedentary people. With proper treatment, 80% of patients with plantar fasciitis improve within 12 months. Plantar fasciitis is predominantly a clinical diagnosis. Symptoms are stabbing, nonradiating pain first thing in the morning in the proximal medioplantar surface of the foot; the pain becomes worse at the end of the day. Physical examination findings are often limited to tenderness to palpation of the proximal plantar fascial insertion at the anteromedial calcaneus. Ultrasonography is a reasonable and inexpensive diagnostic tool for patients with pain that persists beyond three months despite treatment. Treatment should start with stretching of the plantar fascia, ice massage, and nonsteroidal anti-inflammatory drugs. Many standard treatments such as night splints and orthoses have not shown benefit over placebo. Recalcitrant plantar fasciitis can be treated with injections, extracorporeal shock wave therapy, or surgical procedures, although evidence is lacking. Endoscopic fasciotomy may be required in patients who continue to have pain that limits activity and function despite exhausting nonoperative treatment options.
Plantar fasciitis (also called plantar fasciopathy, reflecting the absence of inflammation) is a common problem accounting for approximately 1 million patient visits per year, with about 60% of these to primary care physicians.1 It is the most common cause of heel pain in adults, with a lifetime incidence of about 10%2 and an increased incidence in women 40 to 60 years of age.1 Plantar fasciitis is associated with a variety of sports but is mostly reported in recreational and elite runners (incidence of 5% to 10%).3
| Clinical recommendation | Evidence rating | References | Comment |
|---|---|---|---|
| Ultrasonography and magnetic resonance imaging are diagnostic options in patients with chronic heel pain despite conservative measures. | C | 3, 13, 14 | Based on systematic reviews of disease-oriented evidence |
| Plantar fascia stretches are effective for reducing heel pain. | B | 17, 18 | Based on small, limited-quality randomized controlled trials |
| Foot orthoses (prefabricated or custom) may reduce heel pain for up to 12 weeks, but the benefit is generally not clinically meaningful in the long term. | B | 21 | Based on moderate-quality evidence from a systematic review and meta-analysis |
| The role of night splints in reducing plantar fasciitis pain is inconclusive. | B | 25, 26 | Based on inconsistent, limited-quality studies |
| Extracorporeal shock wave therapy may have a role in chronic plantar fasciitis that does not respond to conservative therapies. | B | 27, 28 | Based on inconsistent evidence and a meta-analysis |
| Corticosteroid injections may provide, at best, short-term relief for acute and chronic plantar fasciitis. | B | 29 | Based on a Cochrane review of low-quality studies |
Risk Factors
Risk factors for developing plantar fasciitis in nonathletes include limited ankle dorsiflexion, body mass index greater than 27 kg per m2 (odds ratio = 3.7), and spending most of the workday on one's feet 4,5 (Table 16). One study found that reduced ankle dorsiflexion is the greatest risk factor in nonathletes.4 Limited ankle dorsiflexion causes the foot to overpronate, causing more load to be placed on the plantar fascia. The condition also occurs in more active people such as runners and military personnel, but increased body mass index is more weakly associated with plantar fasciitis in these populations.5 Runners and those who spend prolonged time on their feet are more likely to develop the condition because the plantar fascia stretches and contracts (in what is called a typical elastic stretch–shortening cycle), and the repetitive strain can cause an overuse injury.5
| Body mass index > 27 kg per m2 |
| Excessive running |
| Intrinsic foot and calf muscle tightness |
| Leg length discrepancy |
| Occupations requiring prolonged standing or walking |
| Pes cavus (high arch) |
| Pes planus (excessive foot pronation) |
| Reduced ankle dorsiflexion |
| Sedentary lifestyle |
Etiology
The plantar fascia originates from the posteromedial calcaneal tuberosity and inserts into each metatarsal head to form the longitudinal arch of the foot. Plantar fasciitis is a biomechanical overuse condition resulting in degenerative changes at its attachment to the calcaneus. Histologic examination of samples taken from patients undergoing plantar fascia release surgery shows myxoid degeneration with fragmentation and degeneration of the plantar fascia and bone marrow vascular ectasia. These findings support that the condition is a degenerative fasciosis without inflammation, not a fasciitis.7 Therefore, plantar fasciopathy is a more accurate descriptor.
Diagnosis
Plantar fasciitis can be diagnosed clinically by findings from the patient history and physical examination. The patient will have sharp pain in the anteromedial aspect of the heel8 (Figure 16). Pain will begin with ambulation after a period of inactivity, then will improve or resolve as the activity progresses. However, the pain will return at the end of the day. The classic presentation is pain with the first step of the morning. Paresthesia is uncommon. The patient may have had a recent increase in weight-bearing activity.9
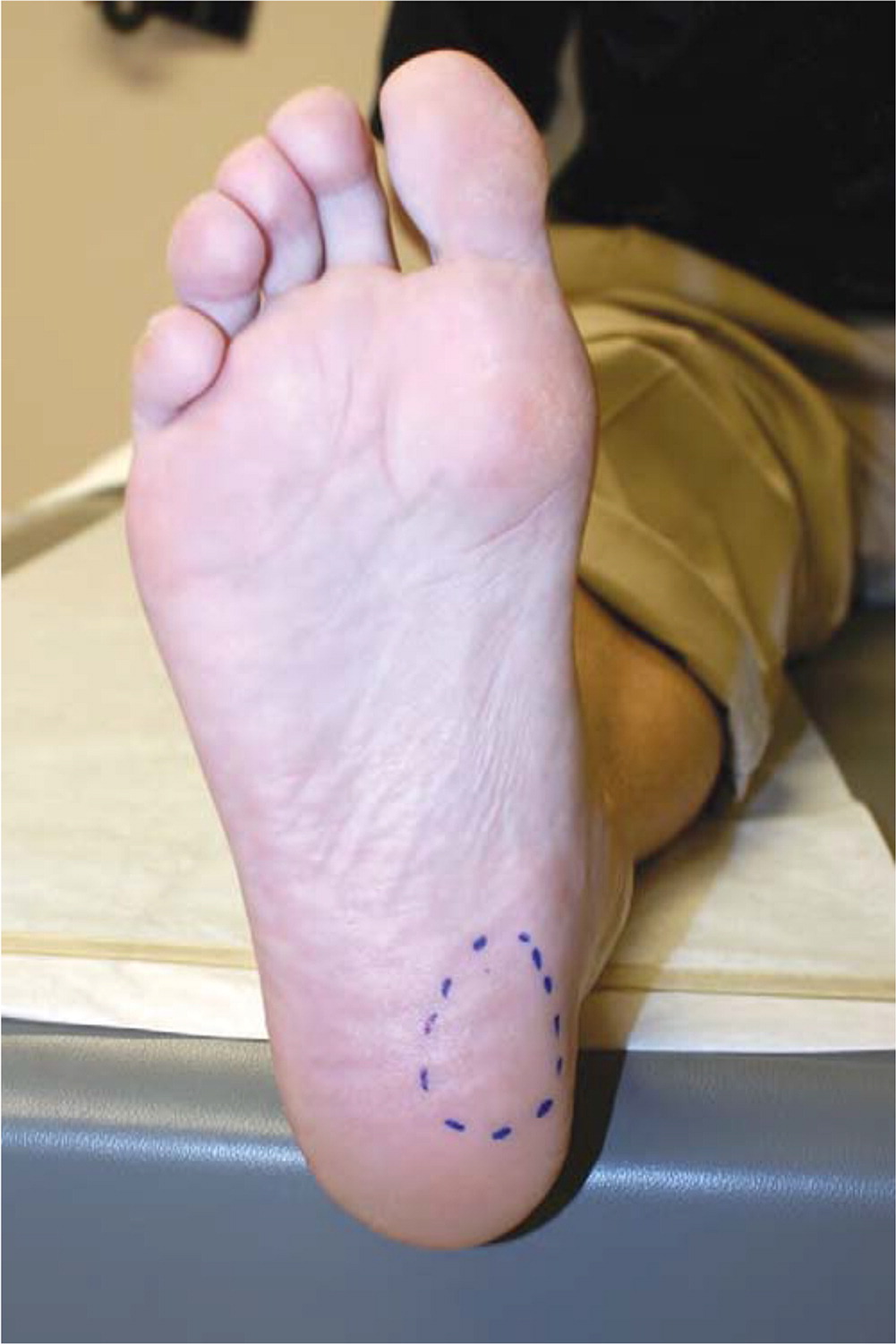
On physical examination, the patient will be tender to palpation on the proximal plantar fascial insertion at the anteromedial calcaneus. The windlass test may also be helpful (https://www.youtube.com/watch?v=fg0PtnoAzSs). A positive result is heel pain reproduced by forced dorsiflexion of the toes at the metatarsophalangeal joints with the ankle stabilized.10 According to one study, the windlass test has 100% specificity and 32% sensitivity (positive likelihood ratio = 1.47).10
Imaging
In most cases, clinical findings are sufficient to diagnose plantar fasciitis. However, imaging may help determine whether an alternate diagnosis (Table 26) is present in patients with pain that lasts longer than three months and does not respond to therapy.11 Guidelines from the American College of Radiology state that although radiography is typically not sensitive for plantar fasciitis, it should be the initial study.12 Magnetic resonance imaging has been proven helpful in the diagnosis of plantar fasciitis. Ultrasonography is effective for differentiating the normal plantar fascia from tissue involved with plantar fasciitis, and it is less expensive.12
| Etiology | Symptoms |
|---|---|
| Neurologic causes | |
| Baxter neuritis | Burning over the medial heel |
| Medial calcaneal nerve entrapment | Burning over the inferomedial aspect of the calcaneus |
| Tarsal tunnel syndrome | Paresthesia in the plantar aspect of the foot |
| Skeletal causes | |
| Acute calcaneal fracture | Inability to bear weight secondary to a high-energy event |
| Bone tumor | Deep bone pain, night pain |
| Calcaneal apophysitis (Sever disease) | Heel pain in girls eight to 13 years of age or boys 10 to 15 years of age |
| Calcaneal stress fracture | Slow-onset heel pain secondary to repetitive loading |
| Spondyloarthropathies | Heel pain at Achilles tendon insertion |
| Soft tissue causes | |
| Achilles tendinitis | Posterior ankle pain at medial malleolus level |
| Fat pad contusion | Centralized heel pain |
| Flexor hallucis longus tenosynovitis | Pain with resisted flexion of the great toe |
| Plantar fascia rupture | A pop followed by sudden onset of pain |
| Plantar fibroma | Nodule in the plantar surface of foot midportion |
| Posterior tibial tendinitis | Pain with resistance to foot inversion |
| Retrocalcaneal bursitis | Swelling and pain of the retrocalcaneal region |
Plain radiography can evaluate for bony lesions. A heel spur may be visible on lateral heel radiographs, but this is not pathognomonic of plantar fasciitis because it is a common incidental finding in asymptomatic patients (Figure 2).6 Although people with chronic heel pain are more likely to have a bone spur,13 the spur will remain after symptoms resolve.

Ultrasonography is an inexpensive, accurate, and reliable alternative to magnetic resonance imaging for evaluation of heel pain.14 Ultrasound findings consistent with plantar fasciitis include greater plantar fascia thickness compared with controls,13 plantar fascia thickness greater than 4.0 mm (odds ratio = 105.11; 95% CI, 3.09 to 3,577.28; P = .01),13 and reduced echogenicity of the plantar fascia.3 If ultrasonography is not available in the clinic, the patient can be referred for further imaging.
Magnetic resonance imaging can be useful to rule out other conditions, such as plantar fascia tears or calcaneal stress fracture. It can show increased plantar fascia thickness and signal intensity.3
Nonoperative Treatment
Approximately 80% of patients with plantar fasciitis improve within 12 months with nonoperative therapy.15 Nonoperative management initially consists of activity modification, ice massage, nonsteroidal anti-inflammatory drugs, stretching, strengthening exercises, and heel padding. The American College of Foot and Ankle Surgeons recommends tailoring treatment to the patient's symptoms, lifestyle, and activity level rather than following a treatment ladder because most treatment modalities are not supported by sufficient evidence, but most are clinically successful when used.11
STRETCHING/STRENGTHENING
Previously, stretching protocols emphasized stretching the Achilles tendon because lack of ankle dorsiflexion is a risk factor for plantar fasciitis.4 However, studies have indicated that plantar fascia–specific stretching may be more beneficial (Figure 3 and Figure 4).16 One randomized controlled trial (RCT) assigned 82 patients to plantar fascia stretching or Achilles tendon stretching.17 Both groups received nonsteroidal anti-inflammatory drugs and insoles. Heel pain improved by 52% at eight weeks in the plantar fascia group compared with 22% in the Achilles tendon group. Another RCT compared outcomes from a plantar fascia– specific stretching protocol vs. a high-load strengthening program to support the Achilles tendon and the plantar fascia windlass mechanism (which raises the arch and shortens the foot during the propulsive phase of the gait).18 Patients who underwent the strength training program had more improvement at three months than the stretching group; however, both groups improved.


FOOT ORTHOSES
Foot orthoses are thought to reduce symptoms of plantar fasciitis by reducing strain on the fascia.19 Orthoses can provide medial arch support and reduce foot pronation. A 2006 RCT assigned 135 patients to a sham orthosis, prefabricated orthosis, or customized orthosis.20 After three months, the patients who used customized and prefabricated orthoses had improved function and pain, with no difference in pain between the customized and prefabricated orthosis groups. A recent systematic review and meta-analysis of 19 studies on the use of foot orthoses in adults with plantar heel pain found that orthoses decreased pain between seven and 12 weeks compared with sham orthoses, but that pain was not consistently improved in the long term (13 to 52 weeks).21 In addition, all of these studies indicate that using an off-the-shelf orthosis was as effective as using a customized orthosis.
TAPING
Low-Dye taping is a technique to treat plantar fasciitis in people with excessive pronation (https://www.youtube.com/watch?v=ZwMZ90BdYhw). The principle is to fix the subtalar joint axis, which consequently reduces excessive pronation and corrects foot disorders.22 Studies have shown that Low-Dye taping reduces pain at one week, but effectiveness wanes afterward.23
DRY NEEDLING/ACUPUNCTURE
Acupuncture and dry needling have been used to treat plantar fasciitis. A thin needle is inserted into a myofascial trigger point, which decreases pain by altering the biochemical environment and local blood flow.24 A meta-analysis showed that myofascial trigger point needling reduces pain in patients with plantar fasciitis.24 However, it was limited by inclusion of different techniques and lower-quality studies. Because of the lack of high-quality evidence, the American College of Foot and Ankle Surgeons does not recommend for or against these treatments.11
NIGHT SPLINTS
A night splint maintains the ankle in a neutral or dorsiflexed position during sleep to prevent contracture of the gastrocnemius–soleus complex. Evidence on the benefits of night splints for the treatment of plantar fasciitis is conflicting. An RCT (N = 116) showed no improvement of symptoms when a night splint was added to a regimen of nonsteroidal anti-inflammatory drugs and Achilles tendon stretching.25 However, another RCT (N = 28) showed that a combination of foot orthoses and night splints resulted in lower pain scores compared with orthotic insoles alone at two and eight weeks.26 Further studies are needed to determine the role of night splints in the treatment of plantar fasciitis.
EXTRACORPOREAL SHOCK WAVE THERAPY
Extracorporeal shock wave therapy (ESWT) was introduced in the early 1990s as a treatment for insertional tendinopathies. The shock waves stimulate healing by producing vibration that encourages circulation. It is thought to stimulate neovascularization, increase growth factors, and destruct unmyelinated nerve fibers (substance P fibers). Shock waves can be delivered from low- to high-energy waves, and the wave modality can be focused or radial. There is no consensus on the optimal shock wave intensity, modality, or pulse cycle protocol for the treatment of plantar fasciitis. Some studies have shown no benefit of ESWT for plantar fasciitis. One of these, an RCT of 166 people randomized to placebo or ultrasound-guided ESWT, found that both groups had improvement in heel pain, but that there was no benefit after treatment completion.27 This difference in treatment may be due to the large variation of treatment force (0.02 to 0.33 mJ per mm2) used. Findings from a meta-analysis indicate that a force of 0.28 mJ per mm2 produces benefits.28
A recent meta-analysis evaluated nine RCTs that included sham treatment as the comparator and concluded that focused application of ESWT should be recommended as remedial treatment after failure of traditional conservative therapy, thus possibly avoiding surgical intervention. However, this finding was limited by the small study size.28
INJECTIONS
Corticosteroids are commonly used to decrease pain and inflammation. Although plantar fasciitis is a degenerative rather than inflammatory process, there is evidence of a short-term therapeutic effect of corticosteroids.29 An RCT assigned 83 patients with plantar fasciitis to ultrasound-guided injection of normal saline or dexamethasone.30 The dexamethasone group had better pain relief at four weeks (number needed to treat = 3) and decreased plantar fascia swelling at three months compared with the saline injection group. A 2014 meta-analysis showed that ultrasound-guided injections are superior to palpation-guided injections for pain relief and reducing plantar fascia thickness.31 Potential complications of corticosteroid injections include fascia rupture and fat pad atrophy. Rupture occurs in an estimated 2.4% of patients who receive multiple injections, and injections on the calcaneal side of the plantar fascia are thought to be less likely to cause fat pad atrophy.32
Autologous blood-derived products (platelet-rich plasma and whole blood) have the potential to stimulate tissue regeneration. In theory, these injections could be superior to corticosteroid injections in the treatment of plantar fasciitis because it is not an inflammatory process. A meta-analysis compared pain scores three months after treatment with autologous blood-derived products, corticosteroid injections, or ESWT.33 Subgroup analysis found that platelet-rich plasma injections conferred the best immediate results, whereas ESWT had the highest likelihood of success at three months. However, a recent meta-analysis of 39 trials suggested minimal, if any, benefit from platelet-rich plasma injections compared with control interventions, based on very low-quality evidence.34 In addition, autologous blood-derived product injections are not covered by insurance plans and can incur large costs for patients. Whole blood injections may not have additional costs beyond the cost of the injections because unlike platelet-rich plasma, whole blood does not require additional processing, which can be expensive. A study comparing platelet-rich plasma and whole blood injections showed no significant differences in effectiveness between treatments; each was about 80% successful at three months.35
Botulinum toxin has been used to treat many chronic pain conditions. Its mechanisms of action include inhibition of pain peptide release from nerve terminals and sensory ganglia, anti-inflammatory and antiglutaminergic effects, and reduction of sympathetic neural discharge. Several small RCTs and a meta-analysis indicate that botulinum toxin injections improve pain and overall foot function at three and eight weeks in patients with plantar fasciitis.36,37 Data comparing ultrasound-guided botulinum toxin injections with ultrasound-guided corticosteroid injections suggest greater benefit with botulinum toxin.38
Surgery
Plantar fasciitis is typically self-limited, with 80% of patients improving within one year.15 However, surgery can be considered when nonoperative treatments have failed. Open, percutaneous, or endoscopic plantar fasciotomy without inferior calcaneal exostectomy is the preferred surgical method.39 The open approach requires patients to be nonambulatory for three weeks after surgery. A return to full activity may take up to three months. Potential complications include plantar arch collapse and scarring of the incision site. Endoscopic fasciotomy has become the standard surgical treatment. An RCT comparing open vs. endoscopic plantar fasciotomy found that patients who underwent the endoscopic procedure had earlier return to activity and earlier improvements in functional outcomes and pain relief.40 One study followed 652 patients who underwent endoscopic plantar fasciotomy; 97% reported pain relief and 77% had returned to wearing a regular shoe seven days after the procedure.41 Complications include arch destabilization, midfoot pain, heel pain, and loss of arch height.
This article updates previous articles on this topic by Goff and Crawford6 ; Cole, et al.42 ; and Young, et al.43
Data Sources: We searched PubMed, EBSCO, CINAHL, and the Cochrane database using the key words plantar fasciitis and plantar fasciopathy, in addition to the Essential Evidence Plus summary provided by American Family Physician. The search was limited to meta-analyses, systematic reviews, randomized controlled trials, and reviews published in the past 10 years. Search dates: October 2018 and April 2019.
