
Yes, it's complicated, but don't make it harder than it has to be.
Fam Pract Manag. 2010;17(3):24-29
Kent Moore is the AAFP's manager for health care financing and delivery systems and is a contributing editor to FPM. Author disclosure: nothing to disclose.

The 1997 version of Medicare's “Documentation Guidelines for Evaluation and Management Services” defines complete exams for 11 organ systems and significantly expands the definitions for multi-system exams. When the guidelines were released, some physicians appreciated their specificity, while many declared them too burdensome to use. Developed as a replacement for the 1995 documentation guidelines, the 1997 version produced such an uproar among physicians and organized medicine that the Centers for Medicare & Medicaid Services (CMS) first delayed its implementation and then ultimately declared it an alternative to, rather than a replacement for, the 1995 version (see “What about the 1995 guidelines?”).
The purpose of this article is to review the guidelines and help you determine whether your documentation would stand up to an auditor's evaluation. We'll focus on the 1997 guidelines and the multisystem exam, since they are commonly used in family medicine. An overview of the single-system exam requirements is available as a download (
). If you'd like to brush up on the rest of the guidelines, see the article on history documentation in our March/April 2010 issue, and don't miss the next article in this series, which will focus on documenting medical decision making.
WHAT ABOUT THE 1995 GUIDELINES?
In the 1995 documentation guidelines, the level of exam depends, simply enough, on the number of organ systems that are examined and documented. The 1995 guidelines don't specify what constitutes an exam of any organ system and, thus, they don't indicate how much documentation is necessary to substantiate that the system in question has in fact been examined. Some physicians claim that this makes the 1995 guidelines easier to use, but many physicians have adopted the 1997 guidelines. Either version may be used, but it is not permissible to combine them, for example by using the exam section of the 1995 guidelines with the history and decision making sections of the 1997 guidelines.
Multisystem exam
The levels of evaluation and management (E/M) service reflect four levels of examination:
Problem focused exam – a limited exam of the affected body area or organ system.
Expanded problem focused exam – a limited exam of the affected body area or organ system and any other symptomatic or related body area(s) or organ system(s).
Detailed exam – an extended exam of the affected body area(s) or organ system(s) and any other symptomatic or related body area(s) or organ system(s).
Comprehensive exam – a general multisystem exam, or a complete exam of a single organ system and other symptomatic or related body area(s) or organ system(s).
The guidelines include a detailed chart that specifies the exam elements that must be performed and documented to justify each level of exam. In the chart, the shaded headings list the organ systems and body areas as CPT categorizes them.
These body areas and systems are worth some attention. Look closely at the terms and the way they are grouped; they may not correspond exactly to those you are used to running through in your mind. For instance, if you are used to documenting as one unit your findings for “HEENT” or even “HEENTN,” including the neck as well as head, eyes, ears, nose and throat, note that you are in fact documenting findings for one body area (neck) and two organ systems (eyes and ears, nose, mouth and throat).
One other point to keep in mind about the list of systems: It doesn't mention the endocrine system or the allergic/immunologic system, although both are included in the list for documenting the review of systems (ROS). This presumably represents recognition that these systems are easier to ask about than to examine.
Now, back to the multisystem exam chart. The elements of the exam related to each body area and organ system are identified by bullets (•). Parenthetical examples provide clarification and guidance within the chart. Any numeric requirements included in the description of the element (such as “Measurement of any three of the following seven …”) must be satisfied. Elements that have multiple components but that include no specific numeric requirement (such as “Examination of liver and spleen”) require documentation of only one of the components. Finally, CMS urges you to keep in mind that the use of the documentation guidelines is not a substitute for medical necessity. A well documented service won't automatically be assumed to have been medically necessary.
GENERAL MULTISYSTEM EXAMINATION
Constitutional
Measurement of any three of the following seven vital signs: 1) sitting or standing blood pressure, 2) supine blood pressure, 3) pulse rate and regularity, 4) respiration, 5) temperature, 6) height or 7) weight (may be measured and recorded by ancillary staff)
General appearance of patient (e.g., development, nutrition, body habitus, deformities, attention to grooming)
Eyes
Inspection of conjunctivae and lids
Examination of pupils and irises (e.g., reaction to light and accommodation, size, symmetry)
Ophthalmoscopic examination of optic discs (e.g., size, C/D ratio, appearance) and posterior segments (e.g., vessel changes, exudates, hemorrhages)
Ears, Nose, Mouth and Throat
External inspection of ears and nose (e.g., overall appearance, scars, lesions, masses)
Otoscopic examination of external auditory canals and tympanic membranes
Assessment of hearing (e.g., whispered voice, finger rub, tuning fork)
Inspection of nasal mucosa, septum and turbinates
Inspection of lips, teeth and gums
Examination of oropharynx: oral mucosa, salivary glands, hard and soft palates, tongue, tonsils and posterior pharynx
Neck
Examination of neck (e.g., masses, overall appearance, symmetry, tracheal position, crepitus)
Examination of thyroid (e.g., enlargement, tenderness, mass)
Respiratory
Assessment of respiratory effort (e.g., intercostal retractions, use of accessory muscles, diaphragmatic movement)
Percussion of chest (e.g., dullness, flatness, hyperresonance)
Palpation of chest (e.g., tactile fremitus)
Auscultation of lungs (e.g., breath sounds, adventitious sounds, rubs)
Cardiovascular
Palpation of heart (e.g., location, size, thrills)
Auscultation of heart with notation of abnormal sounds and murmurs
Examination of:
carotid arteries (e.g., pulse amplitude, bruits)
abdominal aorta (e.g., size, bruits)
femoral arteries (e.g., pulse amplitude, bruits)
pedal pulses (e.g., pulse amplitude)
extremities for edema and/or varicosities
Chest (Breasts)
Inspection of breasts (e.g., symmetry, nipple discharge)
Palpation of breasts and axillae (e.g., masses or lumps, tenderness)
Gastrointestinal (Abdomen)
Examination of abdomen with notation of presence of masses or tenderness
Examination of liver and spleen
Examination for presence or absence of hernia
Examination of anus, perineum and rectum, including sphincter tone, presence of hemorrhoids and rectal masses
Obtain stool sample for occult blood test when indicated
Genitourinary
Male:
Examination of scrotal contents (e.g., hydrocele, spermatocele, tenderness of cord, testicular mass)
Examination of penis
Digital rectal examination of prostate gland (e.g., size, symmetry, nodularity, tenderness)
Female:
Pelvic examination (with or without specimen collection for smears and cultures), including:
Examination of external genitalia (e.g., general appearance, hair distribution, lesions) and vagina (e.g., general appearance, estrogen effect, discharge, lesions, pelvic support, cystocele, rectocele)
Examination of urethra (e.g., masses, tenderness, scarring)
Examination of bladder (e.g., fullness, masses, tenderness)
Cervix (e.g., general appearance, lesions, discharge)
Uterus (e.g., size, contour, position, mobility, tenderness, consistency, descent or support)
Adnexa/parametria (e.g., masses, tenderness, organomegaly, nodularity)
Lymphatic
Palpation of lymph nodes in two or more areas:
Neck
Axillae
Groin
Other
Musculoskeletal
Examination of gait and station
Inspection and/or palpation of digits and nails (e.g., clubbing, cyanosis, inflammatory conditions, petechiae, ischemia, infections, nodes)
Examination of joint(s), bone(s) and muscle(s) of one or more of the following six areas: 1) head and neck; 2) spine, ribs and pelvis; 3) right upper extremity; 4) left upper extremity; 5) right lower extremity; and 6) left lower extremity. The examination of a given area includes:
Inspection and/or palpation with notation of presence of any misalignment, asymmetry, crepitation, defects, tenderness, masses or effusions
Assessment of range of motion with notation of any pain, crepitation or contracture
Assessment of stability with notation of any dislocation (luxation), subluxation or laxity
Assessment of muscle strength and tone (e.g., flaccid, cog wheel, spastic) with notation of any atrophy or abnormal movements
Skin
Inspection of skin and subcutaneous tissue (e.g., rashes, lesions, ulcers)
Palpation of skin and subcutaneous tissue (e.g., induration, subcutaneous nodules, tightening)
Neurologic
Test cranial nerves with notation of any deficits
Examination of deep tendon reflexes with notation of pathological reflexes (e.g., Babinski)
Examination of sensation (e.g., by touch, pin, vibration, proprioception)
Psychiatric
Description of patient's judgment and insight
Brief assessment of mental status, including:
orientation to time, place and person
recent and remote memory
mood and affect (e.g., depression, anxiety, agitation)
Multisystem exam requirements
To qualify for a given level, your exam must meet the following content and documentation requirements (these are summarized in the table "Exam content and documentation requirements"):
Problem focused – should include performance and documentation of one to five bulleted elements in at least one organ system or body area;
Expanded problem focused – should include performance and documentation of at least six bulleted elements in at least one organ system or body area;
Detailed – should include performance and documentation of at least two bulleted elements from each of six organ systems or body areas OR performance and documentation of at least 12 bulleted elements; the 12 elements must be drawn from two or more organ systems or body areas;
Comprehensive – should include at least nine organ systems or body areas. For each system/area selected, all bulleted elements should be performed, unless specific directions limit the content of the examination, and at least two bulleted elements should be documented.
One way to remember the distinctions is to “think in sixes”: The lowest level of exam has fewer than six bulleted elements, the next level has six or more, the next has 12 or more, and the highest has 18 or more. Also note that the definition of the detailed exam is not as complicated as it may sound. The first alternative (at least two elements from each of six systems or body areas) is just a special case of the second. If you document 12 bulleted elements, you've documented a detailed exam, whether those 12 elements are spread evenly over 6 systems and body areas or not. The points to remember for the detailed exam are 12 bulleted elements and at least two systems or body areas. If you prefer to think in terms of six systems and two bulleted points per system, fine. Just remember that this is only one possibility.
Note the peculiar wording of the requirement for the comprehensive general multisystem exam: While the guidelines say explicitly that you must perform all the elements of the exam identified by bullets in the nine or more systems or body areas you examine, they require that you document only two per system or area. This distinction is evidently deliberate. The rationale, as best we can understand, is that requiring all bulleted items to be covered in the exam ensures that the physician work going into the exam is adequate to justify the level of reimbursement, while requiring documentation of only two elements somewhat relieves the physician's documentation task.
| Exam type | Requirements | Systems/Areas | Bulleted elements |
|---|---|---|---|
| Problem focused | Perform and document one to five elements identified by a bullet. | 1+ | <6 |
| Expanded problem focused | Perform and document at least six elements identified by a bullet. | 1+ | 6+ |
| Detailed | Perform and document at least 12 elements identified by a bullet in two or more systems/areas. | 2+ | 12+ |
| Comprehensive (general multisystem) | Perform all elements identified by a bullet and document at least two elements identified by a bullet from each of at least nine systems/areas.* | 9+ | 18+ |
Practice
The requirements for the problem focused exam are minimal. If you or your ancillary staff measure and document even three of the seven vital signs listed in the chart, you have documented a problem focused exam. For instance, a notation of “BP 126/86, P 82, WT 190” meets the requirements of the first bullet under the Constitutional system, and since you performed and documented “one to five elements identified by a bullet in one or more organ system(s) or body area(s),” you've met the requirements for documenting a problem focused exam.
For an expanded problem focused exam, the threshold is six elements identified by a bullet in one or more organ system(s) or body area(s). Consider this example: You see a 55-year-old man who has returned for follow-up of his hypertension. His only complaint is a scratchy throat that he's had for the past several days. Your observations are noted as follows:
The following elements identified by bullets in the CMS table are documented in the note:
Constitutional: Measurement of three vital signs (“BP 126/86, P 82, WT 190”);
Ears, Nose, Mouth and Throat: Examination of oro-pharynx (“oropharynx benign”);
Ears, Nose, Mouth and Throat: Otoscopic examination of external auditory canals and tympanic membranes (“TMs nl”);
Eyes: Examination of pupils and irises (“PERRLA”);
Neck: Examination of neck (“Supple”);
Cardiovascular: Examination of carotid arteries (“NECK: … w/o … bruits”)
Neck: Examination of thyroid (“w/o … thyromegaly”);
Respiratory: Percussion of chest (“BS clr to percussion”);
Respiratory: Auscultation of lungs (“BS clr to … auscultation”);
Cardiovascular: Auscultation of heart with notation of abnormal sounds and murmurs (“WNL w/o gallop, murmur, rub, click or irregularity”);
Cardiovascular: Examination of extremities for edema and/or varicosities (“w/o edema, pulses intact”).
To be precise, you have documented that you examined at least 11 elements identified by a bullet. That's more than enough to substantiate that you did an expanded problem focused exam and almost enough for a detailed exam. In fact, if you had happened to add a comment about the patient's general appearance (a bulleted item under the Constitutional system), you'd have documented 12 items in two or more systems, which is the minimum required for a detailed exam.
Finally, there is the comprehensive multisystem exam. Previously, the guidelines required that such an exam include findings from eight or more of the 12 organ systems. The revised guidelines require documentation of at least two elements from each of nine body areas and/or systems out of the 14 body areas or systems recognized. This is more stringent in that it raises the bar from eight to nine and requires documenting two exam elements for each system or area examined, but it is less stringent at least in that you can now count organ systems and body areas.
In the example discussed above, the physician performed and documented at least two elements from each of the following five body areas or organ systems: Constitutional (assuming the addition of a note about general appearance); Ears, Nose, Mouth and Throat; Neck; Respiratory; and Cardiovascular. A comprehensive multisystem exam would pretty clearly be inappropriate given the clinical situation and chief complaint, but just by way of illustration, it would also require the physician to document at least two elements from four of the following additional body areas or organ systems to bring the total number of body areas or organ systems to nine: Eyes; Chest (Breasts); Gastrointestinal (Abdomen); Genitourinary; Lymphatic; Musculoskeletal; Skin; Neurologic; and Psychiatric. As noted above, the guidelines require that all the elements listed be performed for each body area or organ system examined, even though only two in each area or system must be documented.
Writing it down
The guidelines make several points about what you actually write in the record to document your findings. They can be paraphrased as follows:
Note all abnormal or unexpected findings, no matter whether they're related to the presenting problem. If you note an abnormal finding, be specific. It may seem unnecessary to say so, but “Neck: abnormal” is not enough.
Include equally specific notes of normal (negative) findings if they are relevant to the patient's problem (for instance, “Neck: supple” in a child with fever).
If you examine an unaffected area or asymptomatic organ system and find no abnormalities, a brief note is enough (“Skin: nl”; “GI: nl”).
While the guidelines say what CMS would like to see included in your documentation, they don't dictate the format. CMS has said that it's the reviewer's responsibility to pull the information out of the chart, not the doctor's responsibility to make the record easier for the reviewer to read. That said, some physicians do attempt to organize their notes to facilitate the reviewer's counting of HPI elements covered, systems examined, and so on. The FPM Toolbox includes a template for documenting E/M visits that facilitates this sort of counting. For additional suggestions, see “The organized note.” Good luck!
THE ORGANIZED NOTE
Making sure your notes are organized as a reviewer would like them can't hurt, although if it requires changing your documentation habits, it can slow you down a little until you're used to it. Whether you need to train yourself or your transcriptionist, consider following these guidelines:
Use an outline format. Use S, O, A and P or History, Examination and Medical Decision Making as the main headings.
Subdivide each of the major sections appropriately. The more recognized subdivisions you use, the better, particularly with a long note. Although the guidelines don't require it, label CC, HPI, ROS and PFSH separately if you think the demarcations between them might be unclear, and label each body part or system examined.
Be succinct but thorough. Using unnecessary words, complete sentences and multiline paragraphs obscures both the critical information and the demarcations between subsections. If you don't start each subsection on a new line, at least make sure each one can easily be identified in the text, for instance by starting each with a heading all in capital letters (NECK: Supple w/o JVD, bruits or thyromegaly. CHEST: Breath sounds clr to percussion & auscultation).
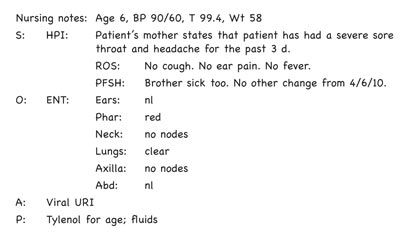
Here is what a well-organized note might look like:
Editor's note: FPM was published for several years before going online. In an effort to capture the best of the “pre-web” FPM for the online archive, we are publishing updated versions of some particularly useful early articles. This article is adapted from one that appeared in 1997.
