Engaging office staff will make your practice's antibiotic stewardship efforts more effective.
Fam Pract Manag. 2021;28(6):10-14
Author disclosures: The practice improvement work that is the basis for this article was funded by a State University Partnership contract between the Kentucky Department for Medicaid Services and the University of Louisville. This article represents the view of the authors only. No other relevant financial affiliations.

Antibiotic stewardship is an important strategy for reducing the development of antimicrobial resistance and harmful side effects. Approximately 85%–95% of antibiotic use occurs in the outpatient setting, and at least 30% of prescriptions are considered unnecessary.1,2 In 2016, the Centers for Disease Control and Prevention (CDC) published the “Core Elements of Outpatient Antibiotic Stewardship” with recommendations on how to combat inappropriate prescribing.3 While physicians and other prescribers have an important role in these efforts and should serve as practice leaders (see the related article), there are opportunities for all medical office staff to be involved. By incorporating antibiotic stewardship education and appropriate communication practices throughout the primary care visit, practices have the potential to change the culture and expectations of antibiotic prescribing for sick visits.
KEY POINTS
While physicians and other prescribers have a key role to play in antibiotic stewardship, it's important to get all medical office staff involved as well.
Staff training should include recommended ways to communicate with patients about antibiotic use.
From appointment scheduling to the exam room, patients should receive consistent messages and educational resources about the appropriate use of antibiotics.
GETTING STARTED
To lay the groundwork for antibiotic stewardship among staff, practices should take the following steps:
1. Identify champions to lead antibiotic stewardship efforts. Consider appointing at least two champions: a prescriber and a support staff person, such as a nurse or medical assistant. Champions will be responsible for leading and maintaining stewardship initiatives. If possible, add these roles to formal job descriptions.
2. Require all office staff to complete antibiotic stewardship training. Practices can use existing resources for training. We recommend the CDC's free, online Antibiotic Stewardship Training Series4 or an in-person summary of the CDC training concepts led by office champions. The first six CDC modules offer introductory information about antibiotic use, resistance, stewardship, and communication, which can be helpful to office staff. Prescribers can benefit from additional modules that discuss specific clinical conditions.
3. Organize an antibiotic communication discussion at a staff meeting. An important piece of the CDC training is the communication module. Based on robust research from Seattle Children's Research Institute,5 it summarizes messages that physicians and office staff can use to help manage patient expectations about antibiotic use. (See “Messages to improve antibiotic stewardship” and “Examples of appropriate staff responses to patient comments.”) Staff should discuss and practice these responses. Stewardship champions can identify real-life situations to use in interactive sessions with staff.
| Stage of visit | Concerning message | Improved message |
|---|---|---|
| Candidate diagnosis, which may be either explicit (the parent/patient names a diagnosis) or implicit (the parent/patient describes symptoms or names a condition someone close to patient has been diagnosed with) | “There has been a lot of strep going around.” | “Being around others who are sick is concerning. I hope that's not the case for you.” |
| Physical exam | “Wow, that is a really high fever!” | “Your temperature is elevated.” |
| Diagnosis | “The test says you probably don't have strep.” | “Your rapid strep test is negative.” |
| Treatment recommendations, both negative (rule out the need for antibiotics) and positive (offer symptom relief) | “I don't think you need antibiotics yet.” | “Antibiotics will not treat your viral infection. A saline nasal spray will help with your congestion.” |
| Follow-up, which should provide a contingency plan | “You should feel better soon.” | “We are happy to see you again if your symptoms don't improve or get worse. Please let us know if you have questions in the meantime.” |
| Patient comment | Appropriate response |
|---|---|
| “I just want to feel better soon so I can get back to work.” | “Unfortunately, many illnesses don't have a quick fix. I'm sure Dr. X will come up with a plan to help you feel better in the meantime.” |
| “The last time I had this illness, antibiotics cleared it up right away.” | “Luckily, most colds are caused by viruses and do not require antibiotics.” |
| “I can't believe they wouldn't prescribe me an antibiotic.” | “At least you don't have to worry about the nasty side effects they can cause.” |
| “This appointment was a waste of time.” | “It's still good that you came in. It is always reassuring to know you don't have something more serious going on.” |
| “I guess I'll have to go somewhere else to get what I need.” | “I'm sorry you are dissatisfied with your care here. I can assure you that Dr. X is committed to providing the best care to patients, and sometimes antibiotics can cause more harm than good.” |
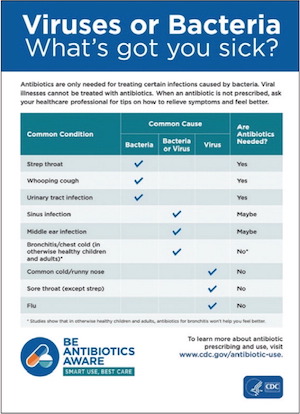
4. Provide patient education throughout the office, not just in the exam room. One of the most challenging times to discuss concerns of inappropriate antibiotic use is while a patient is experiencing an illness. Consider providing patient education on antibiotic awareness outside of sick visits. The CDC offers free patient education materials (handouts, posters, and videos), social media messaging, and more through its “Be Antibiotics Aware” campaign (https://www.cdc.gov/antibiotic-use/materials-references/).6 Additionally, many states have targeted antibiotic awareness campaigns. (See “Sample patient education materials.”) An online search or inquiry to your state department of public health or local academic medical center could reveal more individualized results. Like other public health campaigns, antibiotic awareness requires repeated messaging to shift the public's perspective about appropriate antibiotic use.
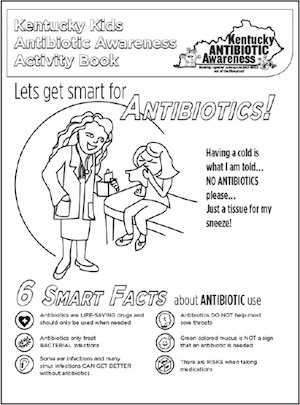
SAMPLE PATIENT EDUCATION MATERIALS
World Antimicrobial Awareness Week materials. World Health Organization.
Kentucky Kids Antibiotic Awareness Activity Book. Kentucky Antibiotic Awareness, University of Louisville Department of Pediatrics, Child and Adolescent Health Research Design and Support Unit.
OPPORTUNITIES THROUGHOUT THE VISIT
After office staff have been trained on antibiotic awareness and communication strategies, they can begin using these concepts throughout the patient visit.
Appointment scheduling. When patients call to schedule an appointment, a customized hold message can educate them about when antibiotics are and are not needed. Triaging can also prevent unnecessary visits (e.g., visits for the common cold). Training office staff to provide self-care advice has shown to be effective for managing upper respiratory infection symptoms.7 For offices that use online scheduling, computerized prompts could assist patients in determining whether an office visit is required. The following message could be used for triage:
Cold symptoms are caused by viruses. Unfortunately, we do not have medicines to cure a cold. If you feel comfortable managing your symptoms at home, you could save yourself a trip to the office. Your symptoms will likely last around 7–10 days. If your symptoms continue or become severe, or if you prefer a visit now, we would be happy to see you right away.
Check-in and waiting room. The patient check-in process is another important opportunity for appropriate communication strategies. While the patient is in the waiting room, education can be provided via TV monitor messages, posters, brochures, and children's activity books.
Exam room. Staff should continue to manage expectations through appropriate communication as they take the patient's vitals and medical history. Additionally, studies have shown that displaying a poster with the practice's commitment to appropriate antibiotic prescribing leads to a reduction in inappropriate prescriptions.8,9 Templates are provided on the CDC website or practices can customize their own.
CASE STUDY
To see how antibiotic stewardship might look in the primary care office setting, let's consider the case of Susie, a 5-year-old patient with mild, intermittent asthma, who has been feeling ill for three days with rhinorrhea, congestion, and cough. She has not been sleeping well and has missed school. Her mother recalls a similar illness last year for which Dr. Smith wrote a prescription for an antibiotic. Susie felt better a few days later. Susie's mother calls their family physician's office to make an appointment.
While waiting on hold, Susie's mother hears the following message: “Did you know most common colds are caused by viruses, which do not respond to antibiotics? Antibiotics can cause unwanted side effects and antibiotic resistance, so they should only be used when necessary.” When the receptionist answers, Susie's mother describes the course of illness. The receptionist asks if they would feel comfortable managing these symptoms at home first, or if they would like to go ahead and make an appointment for later today. Susie's mother worries about her daughter's asthma and decides to proceed with the appointment.
Later that day in the waiting room, Susie enjoys a coloring page and shows her mom. The page includes “Six Smart Facts about Antibiotic Use.” While waiting in the exam room, Susie's mother notices a poster signed by Dr. Smith about his commitment to prescribe antibiotics only when needed.
During the physical exam, Dr. Smith states that Susie's chest sounds clear, and she has an upper respiratory infection, also known as the common cold. He explains that this is caused by a virus and will not respond to antibiotics, but there are some steps they can take to help Susie feel better. Dr. Smith recognizes Susie's mother's concerns and ensures her that they can return to the office if her symptoms do not improve or get worse in the next week. Susie's mother is now more familiar with the side effects of antibiotics, such as diarrhea, and is relieved to not have to worry about those or forcing her daughter to take medicine.
A TEAM EFFORT
The literature supports the inclusion of staff nurses in hospital-based antibiotic stewardship programs.10,11 Engaging outpatient nurses, medical assistants, and other office staff in antibiotic stewardship efforts has the potential to change the culture and patient expectations regarding antibiotic prescribing in office-based primary care.