
Am Fam Physician. 1999;59(8):2155-2167
See related patient information handout on Parkinson's disease, written by the author of this article.
Parkinson's disease is a progressive degenerative disorder of the central nervous system. The hallmark physical signs are tremor, rigidity and bradykinesia. Idiopathic Parkinson's disease is caused by the progressive loss of dopaminergic neurons in the substantia nigra and nigrostriatal pathway of the midbrain. Secondary parkinsonism may be caused by certain drugs (e.g., metoclopramide and haloperidol) or by cerebrovascular disease (e.g., multiple lacunar strokes). The disease can usually be diagnosed based on the history and physical findings. Dopamine replacement is still considered the most efficacious treatment for Parkinson's disease, but dopamine agonists, formerly prescribed only as adjunctive therapy, are emerging as useful initial therapy. Other pharmacologic treatments include drugs that inhibit dopamine-metabolizing enzymes (monoamine oxidase-B and catechol O-methyltransferase). Injections of botulinum toxin can be helpful in patients with associated dystonia or blepharospasm. Surgery may be indicated for certain patients or when symptoms do not respond to medical therapy. Additional adjunctive therapies include physical therapy, nutritional counseling and techniques to help patients manage emotional and cognitive changes related to the disease.
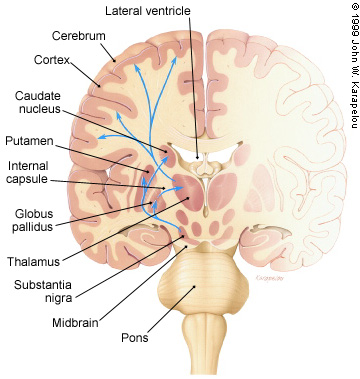
Parkinson's disease, a progressive disorder of the central nervous system (CNS), is caused by the degeneration of dopaminergic neurons in the substantia nigra of the midbrain. These neurons normally project to the striatum, consisting of the caudate and putamen nuclei, whose neurons bear dopamine receptors. This projection of neurons is just one component of the complex network of interconnections among the deep gray-matter structures known as the basal ganglia (Figure 1). Neurochemical or structural pathologic conditions affecting the basal ganglia result in diseases of motor control, classified as movement disorders.
Parkinson's disease has been reported to affect approximately 1 percent of Americans over 50 years of age,1 but unrecognized early symptoms of the disease may be present in as many as 10 percent of those over 60 years of age.2 Early-onset Parkinson's disease, which often affects persons in their 20s, is receiving more attention because of its impact on employability. Epidemiologic studies conducted in the United States have found that Parkinson's disease is more prevalent in men than in women (approximate ratio: 3:2).2
The disease was once thought to affect primarily whites, but recent studies have demonstrated equal prevalence in African Americans and whites living in the same geographic area.3 To date, no studies have determined the prevalence or incidence of Parkinson's disease in Hispanics, and retrospective epidemiologic studies performed in various major cities have yielded contradictory information.4 Variations in the prevalence of the disease in individual racial groups in different geographic areas have suggested an increased risk associated with rural living.5 Pesticides and other toxins have been suspected, but none has been proved to be a definite causative factor.
On the other hand, the search for genetic causes has yielded at least four independent gene loci in various forms of familial Parkinson's disease. The autosomal dominant adult-onset type is linked to a site on chromosome 4q,6 and the gene for autosomal recessive juvenile parkinsonism maps to chromosome 6q.7
Because most patients do not have a clear history of either familial or environmental risk factors, the disorder may be due to a combination of genetic and environmental “influences” or “causes.”
Parkinson's disease severely compromises quality of life. Patients with this illness can find it difficult to read, write and drive. With advanced disease, they often cannot manage basic activities of daily living. Thus, Parkinson's disease can result in loss of employment and, ultimately, loss of personal autonomy.
Clinical Presentation
The first step in evaluating a patient with problems suggestive of Parkinson's disease is to determine which components of motor control are affected. The patient's signs and symptoms are then clustered to determine whether the diagnosis is Parkinson's disease or another movement disorder (Table 1).
| History | |
| Rapid progression | |
| Sphincter dysfunction | |
| Mental status | |
| Early dementia | |
| Psychosis | |
| Depression | |
| Aphasia | |
| Cranial nerves | |
| Visual field cut or neglect | |
| Diplopia | |
| Significant dysphagia | |
| Tongue dysmotility | |
| Motor findings | |
| Weakness | |
| Reflex asymmetry | |
| Fasciculations | |
| Apraxia | |
| Dysmetria | |
| Any sensory finding* | |
Like some other CNS degenerative disorders, Parkinson's disease begins insidiously. Persons close to the patient may notice the problem before the patient does. The patient's facial expression may appear “depressed” or “apathetic,” and the voice may become softer in volume and monotonous in tone. The patient may complain of muscular “weakness” or “stiffness.” Involuntary movements, such as tremor or the turning in of a foot (dystonia), may become a problem. The symptoms may be noticed during routine activities, or they may be present only at certain times, such as when the patient is walking or writing.
In the initial stages of Parkinson's disease, many patients do not have movement problems. Instead, they may complain of anxiety and difficulty sleeping. However, signs of motor system dysfunction become apparent on neurologic and physical examination.
The clinical examination of a patient with possible Parkinson's disease should include a detailed evaluation of mental status, cranial nerves, motor tone, muscular strength, reflexes, coordination and sensation. Kinesis, posture, gait and habitual activities must be observed using physical examination maneuvers that best bring out the patient's motor dysfunction.
The hallmark physical signs of Parkinson's disease are tremor, rigidity and bradykinesia. Poor postural reflexes are sometimes included as the fourth hallmark sign. When postural reflexes are inadequate, patients may fall if they are pushed even slightly forward or backward, or if they are standing in a moving vehicle such as a bus or train. Clinical scales rating the presence and severity of these signs are useful.8
In Parkinson's disease, tremor typically occurs at rest but may also be present when the arms are raised (postural tremor). Tremor is not a pathognomonic sign because it can also occur with other movement disorders. Conversely, not all patients with Parkinson's disease manifest tremor, so the absence of tremor does not rule out the diagnosis.
“Cogwheel rigidity” refers to increased tone that is felt by the examiner as a ratchet-like resistance during passive range of motion. This sign may be present with or without tremor.
“Bradykinesia” means slowed movement and includes both nonvolitional and volitional movements. The “masked facies” of Parkinson's disease is an example of slowed nonvolitional movement. Because adjustments of posture to maintain balance require rapid activation of agonist-antagonist muscle groups, bradykinesia may be the underlying reason for poor postural reflexes in Parkinson's disease.
Differential Diagnosis
The “Parkinson's plus” syndromes are a group of movement disorders with features similar to those seen in idiopathic Parkinson's disease, including bradykinesia and rigidity (Table 2). These disorders include multisystem atrophy, Shy-Drager syndrome and olivopontocerebellar atrophy. Early dementia, orthostatic hypotension (or other signs of autonomic nervous system dysfunction), a wide-based gait, axial rigidity or lack of response to levodopa indicates that one of these other conditions may be present.9 Progressive supranuclear palsy, which is characterized by a vertical (downward) gaze palsy, may also be confused with Parkinson's disease. These conditions are also primary degenerative disorders of the CNS, but they generally do not respond to the medical or surgical treatments that are effective in idiopathic Parkinson's disease.
| Disease | History | Physical examination | Work-up | Treatment options |
|---|---|---|---|---|
| Idiopathic Parkinson's disease | Gradual onset; tremor, gait disturbance, slowed movements | Resting tremor (affects limbs more than head) | Physical examination is best | Levodopa, dopamine agonist, COMT inhibitor, selegiline (Eldepryl), surgery |
| Cogwheel rigidity (affects limbs more than neck or spine) | ||||
| Drug-induced parkinsonism | Previous exposure to a drug such as metoclopramide (Reglan) or haloperidol (Haldol) | Similar to idiopathic Parkinson's disease | History and physical examination are best | Discontinue offending drug or change to another drug if possible |
| Essential tremor | Present for many years, positive family history | Tremor with arms raised (postural), head involved | Physical examination is best | Beta blocker (e.g., propranolol [Inderal]), primidone (Mysoline), anticholinergic drug, surgery |
| Multisystem atrophy | Parkinsonism with autonomic system dysfunction, dysarthria | Orthostatic hypotension, skin changes (e.g., seborrhea) | Physical examination is best | Levodopa trial, measures to control/reduce blood pressure (e.g., salt-intake reduction, support stockings, midodrine [ProAmatine]) |
| Progressive supranuclear palsy | Difficulty reading or driving, stiffness, bradykinesia, cognitive or behavioral changes | Gaze palsy (down more than up), axial rigidity (affects neck and spine more than legs) | Physical examination is best | Levodopa trial, vision aids, physical therapy |
| Huntington's disease | Involuntary movements, cognitive or behavioral problems | Chorea, loose tone, early dementia | CT or MRI studies of head to measure caudate nuclei | Neuroleptic drugs (e.g., haloperidol) |
| Normal-pressure hydrocephalus | Urinary incontinence, memory or cognitive problems | Dementia with frontal lobe features, festinating gait | CT or MRI studies, lumbar puncture | Evaluate for ventriculoperitoneal shunt |
| Multiple lacunar strokes | Stepwise neurologic complaints and functional loss | Focal findings, asymmetric sensory or motor loss | CT or MRI studies of head | Acetylsalicylic acid (aspirin), risk factor control (e.g., diabetes, hypertension, high lipid levels) |
| Pugilistic (post-traumatic) parkinsonism | Repeated head trauma (e.g., in boxers) | Bradykinesia, evidence of previous trauma | CT or MRI studies of head | Levodopa trial, selegiline trial |
| Depression | Dysphoria, poor appetite, disturbed sleep | Depressed mood and affect | Appropriate tests to rule out coexisting organic disease | Antidepressant drugs (selective serotonin reuptake inhibitors, tricyclic antidepressants, etc.) |
Certain prescription medications, particularly neuroleptic drugs (e.g., haloperidol [Haldol]), some antiemetic agents (e.g., prochlorperazine [Compazine]), gastrointestinal antimotility drugs (e.g., metoclopramide [Reglan]) and antihypertensive drugs (e.g., reserpine [Serpasil]), can produce a constellation of symptoms resembling Parkinson's disease. Older women appear to be more likely to develop these extrapyramidal side effects. Some neuroleptic drugs are still used to treat nausea, hiccups and even peripheral neuropathy (e.g., fluphenazine [Prolixin]). Thus, the physician should ask all patients about the use of these medications, not just patients with a psychiatric history. Tremor and other parkinsonian symptoms may improve several weeks after the offending drug has been discontinued. However, the delayed extrapyramidal syndromes, such as tardive dyskinesia and tardive dystonia, are irreversible and may even worsen when the drug is discontinued.10
Focal lesions of the basal ganglia, most commonly deep lacunar infarctions, can also produce parkinsonian symptoms, particularly multiple lesions. Normal-pressure hydrocephalus classically presents with dementia, urinary incontinence and a gait disturbance similar to that seen in Parkinson's disease. Because dementia and urinary incontinence are not typical findings in early Parkinson's disease, normal-pressure hydrocephalus should be suspected in patients with these symptoms.
Depression can be associated with a sad facial expression and psychomotor retardation resembling the masked facies and bradykinesia that occur in Parkinson's disease. Although depression and Parkinson's disease are two distinct conditions, the occurrence of one does not rule out the other. When they coexist, the physician must treat both conditions, with careful attention given to potential drug interactions.11
When the history and physical examination reveal the classic findings of Parkinson's disease, a costly diagnostic work-up is rarely necessary. However, if a diagnosis other than idiopathic Parkinson's disease is suspected, selected laboratory tests (e.g., complete blood count, liver function studies, thyroid-stimulating hormone level, antinuclear antibody determination and erythrocyte sedimentation rate) should be performed.
Computed tomography or magnetic resonance imaging of the head is usually part of the initial work-up. Imaging studies of the brain may reveal focal lesions or other abnormalities, such as normal-pressure hydrocephalus, basal ganglia calcifications or iron deposits.
Neurophysiologic electrodiagnostic studies are useful in diagnosing associated problems such as dystonia or in evaluating sleep problems that do not respond to conventional medications.12 Consultation with a neurologist can assist with the diagnosis and initiation of drug therapy. Follow-up referral to a neurologist or movement disorders specialist can be helpful when treatment response is suboptimal or complications develop.
Pharmacologic Treatment of Parkinson's Disease
The goals of treatment are to alleviate symptoms that interfere with the patient's activities of daily living and to prevent or limit complications as Parkinson's disease progresses. An additional but still only theoretic goal is to prevent or slow the progression of the disease. If secondary parkinsonism is suspected, treatment should be directed at the identified underlying cause. Treatment for idiopathic Parkinson's disease should be initiated as soon as the patient's symptoms begin to interfere with routine activities (Table 3).
| Drug | Mechanism | Indications | Common side effects | Usual starting dosage | Cost (generic)* |
|---|---|---|---|---|---|
| Increase dopamine levels | |||||
| Levodopa-carbidopa (Sinemet) | Precursor with enzyme inhibitor | Parkinson's disease | Dizziness, nausea, hallucinations and others | 25/100 mg three times daily | $ 70 |
| Amantadine (Symmetrel) | Dopamine reuptake inhibitor | Parkinsonism | Confusion, nausea, hallucination | 100 mg twice daily | 54.50 (20 to 26) |
| May lead to neuroleptic malignant syndrome | |||||
| Stimulate dopamine receptors | |||||
| Bromocriptine (Parlodel) | Dopamine agonist (receptor stimulation) | Parkinson's disease, others (?) | † | 1.25 mg twice daily | 29 |
| Pergolide (Permax) | Same as bromocriptine | Same as bromocriptine | † | 0.05 mg at bedtime | 23.50 |
| Pramipexole (Mirapex) | Same as bromocriptine | Same as bromocriptine | † | 0.125 mg three times daily | 65.50 |
| Ropinirole (Requip) | Same as bromocriptine | Same as bromocriptine | † | 0.25 mg three times daily | 84 |
| Inhibit dopamine metabolism | |||||
| Selegiline (Eldepryl) | MAO-B inhibitor | Parkinson's disease, others (?) | Insomnia, headaches, sweating | 5 mg twice daily | 153.50 (122 to 138) |
| Contraindicated with concurrent use of MAO-A drugs | |||||
| Tolcapone (Tasmar) | COMT inhibitor | Parkinson's disease | Dizziness, orthostasis, diarrhea | 100 mg three times daily | 167 |
| Liver function must be monitored | |||||
| Other | |||||
| Diphenhydramine (Benadryl) | Antihistamine | Acute dystonia, parkinsonism | Drowsiness, dry mouth, blurred vision | 25 mg at bedtime | 3 (1 to 2) |
| Trihexyphenidyl (Artane) | Anticholinergic activity | Tremor | Confusion, dry mouth, nausea | 0.5 to 1 mg twice daily | 6‡ |
| Benztropine (Cogentin) | Same as trihexyphenidyl | Same as trihexyphenidyl | Same as trihexyphenidyl | 1 to 2 mg twice daily | 13 (6.50 to 7) |
DRUGS THAT INCREASE DOPAMINE LEVELS
Because dopamine itself does not cross the blood-brain barrier, it is administered as the precursor levodopa in combination with carbidopa (Sinemet). Carbidopa blocks peripheral dopa decarboxylase, the enzyme that converts levodopa to dopamine within the blood-brain barrier. With the levodopa-carbidopa combination, more levodopa reaches the brain and is converted to dopamine.13 This drug combination was named Sinemet (meaning “without emesis”) because it decreases the side effects caused by peripheral dopamine, especially nausea and vomiting.
Although some newer agents are now prescribed as first-line therapy, levodopa is still considered the most efficacious treatment for Parkinson's disease. In addition, a response to this agent confirms the diagnosis. Unfortunately, levodopa's short duration of action necessitates increasingly frequent dosing as the disease progresses. Thus, doses eventually have to be taken as often as every 90 minutes.
The controlled-release formulation of levodopa-carbidopa (Sinemet CR) has to be broken down in the gastrointestinal tract. It can be taken every four to six hours but, because absorption is reduced, higher total daily dosages are usually required.
The side effects of levodopa in either formulation include orthostatic hypotension, nausea, hallucinations and peak-dose dyskinesias. Levodopa therapy should not be used in patients with narrow-angle glaucoma, and caution is advised in giving this drug to patients with malignant melanoma.
Clinical experience has shown that after several years of levodopa therapy, patients tend to develop motor fluctuations such as the “on-off ” phenomenon, “freezing,” “wearing off ” (end-of-dose failure) and dyskinesias (involuntary movements associated with loose muscle tone). Patients with the on-off phenomenon experience abrupt changes in muscle tone, switching from rigidity (“off ”) to a normal or dyskinetic state (“on”) and then back to rigidity (“off ”) within minutes.
Recent studies support the earlier observations14 that motor fluctuations are part of the natural course of Parkinson's disease and are probably related to postsynaptic alterations in the striatum.15 However, dyskinesias have not been observed in patients who have never been exposed to levodopa. The association of dyskinesias with levodopa led to a search for adjunctive treatments. Controversy also arose about how early in the course of Parkinson's disease patients should be treated with levodopa. Delaying levodopa therapy until pronounced disability is present appears to increase the risk of earlier motor complications with treatment and contribute to reduced survival.16
Amantadine (Symmetrel), which has a longer half-life than levodopa, appears to act synergistically with levodopa and thus has been considered useful in the treatment of early Parkinson's disease. Recent reports suggest that amantadine reduces the dyskinesias that occur later in the disease,17 perhaps through antagonist activity at certain glutamate receptors.18 Side effects include orthostatic hypotension, nausea and hallucinations. These effects may limit the use of amantadine in patients with advanced disease.
DRUGS THAT STIMULATE DOPAMINE RECEPTORS
Dopamine receptor agonists were introduced as adjuncts to levodopa therapy to help control the motor fluctuations that occur in patients with Parkinson's disease. The dopamine agonists available for the treatment of Parkinson's disease in the United States are bromocriptine (Parlodel),19 pergolide (Permax),20 pramipexole (Mirapex)21 and ropini-role (Requip).22 Side effects, including nausea, dizziness, hallucinations and cognitive effects, tend to occur most commonly during the first few weeks after initiation of a dopamine agonist. Consequently, dopamine agonists must be started at a low dosage level and gradually titrated to therapeutic levels.
In most cases, dopamine receptor agonists should be initiated when patients are still taking a low to medium dosage of levodopa (i.e., less than 600 mg per day). Patients taking more than 600 mg of levodopa per day have a higher incidence of adverse events from dopamine receptor agonists.
Although dopamine agonists are generally considered useful as adjuncts to levodopa, their introduction in early Parkinson's disease, even as monotherapy, may reduce motor fluctuations later in the disease. As monotherapy, however, dopamine agonists may not provide adequate improvement. Patients who do not respond to levodopa are unlikely to respond to dopamine agonist monotherapy.
Is there a “best” dopamine agonist? The four available agents have affinities for different dopamine receptor subtypes. Debate continues about which of these subtypes are important in the initial pathophysiology of Parkinson's disease, the eventual development of motor fluctuations and the occurrence of pharmacologic side effects.
The characteristics and side effect profiles of the four dopamine agonists used to treat Parkinson's disease are summarized in Table 4. It is important to note that the incidence of adverse effects is higher when a dopamine agonist is taken with levodopa than when it is taken as monotherapy. For example, the initial multicenter trial of combined ropinirole and levodopa therapy22 reported higher rates of nausea (52 percent), dizziness (36 percent) and somnolence (36 percent) than were encountered in a subsequent trial in which ropinirole was used as monotherapy in early Parkinson's disease.23
| Properties and side effects | Bromocriptine (Parlodel) | Pergolide (Permax) | Pramipexole (Mirapex) | Ropinirole (Requip) | |
|---|---|---|---|---|---|
| Properties | |||||
| Initial dosage | 1.25 mg twice daily | 0.05 mg at bedtime | 0.125 mg three times daily | 0.25 mg three times daily | |
| Half-life | 10 to 12 hours | 16 to 24 hours | 8 hours | 6 hours | |
| Side effects | |||||
| Somnolence | + | ++ | +++ | ++ | |
| Insomnia | + | ++ | ++++ | + | |
| Dizziness or lightheadedness | +++ | +++ | +++ | ++ | |
| Hallucinations or confusion | +++ | ++ | ++ | ++ | |
| Headache | +++ | +++ | ++ | ||
| Orthostasis | +++ | +++ | ++ | +++ | |
| Nausea | ++++ | ++++ | ++++ | ++ | |
| Constipation | ++ | ++ | |||
| Others | |||||
| Arthralgia | ++ | ||||
| Blurred vision | ++ | + | |||
| Dry mouth | +++ | ++ | |||
| Pleurisy | ++ | ||||
| Upper respiratory Infection | ++ | ||||
Caution is advised in prescribing dopamine agonists to elderly patients or patients who have already experienced hallucinations, confusion or cognitive impairment. In addition, the ergoline-derived dopamine agonists bromocriptine and pergolide (plus cabergo-line, an agent not available in the United States) have associated risks of retroperitoneal and pulmonary fibrosis and erythromelalgia (redness and burning pain in the distal extremities, usually the feet).
DRUGS THAT INHIBIT DOPAMINE METABOLISM
Dopamine enhancement through the inhibition of dopamine breakdown in the CNS was the philosophy behind the development of selegiline (Eldepryl), a monoamine oxidase B inhibitor. This agent is meant to be used as an adjunct to levodopa therapy. Theoretically, it allows levodopa to be administered less often, but this has not been observed in practice. Although selegiline has antioxidant properties, no evidence supports the earlier notion that the drug is neuroprotective and delays the natural progression of Parkinson's disease.24
Patients treated with selegiline report psychomotor enhancement, perhaps related to the methamphetamine metabolite of the drug.25 Side effects include headache, sweating and insomnia, as well as dopaminergic reactions such as hallucinations, nausea, vomiting and postural hypotension. A report published several years ago indicated that selegiline increased mortality in patients with Parkinson's disease,26 but a recent meta-analysis failed to support this finding.27 Selegiline should not be given to patients who are taking other monoamine oxidase inhibitors. Caution is advised if this drug is prescribed to patients being treated with serotonergic agents (e.g., sumatriptan [Imitrex]) or nonadrenergic agents (e.g., amitriptyline [Elavil]).28 Other relative contraindications to selegiline use are peptic ulcer disease and cardiovascular disease.
Dopamine and its precursor, levodopa, are both metabolized by the enzyme catechol O-methyltransferase (COMT) in the liver, gastrointestinal tract and other organs. By preventing this breakdown, COMT inhibitors enhance the amount of levodopa that reaches the CNS, thereby allowing more of the drug to be converted to dopamine. Although this mechanism parallels that of carbidopa, COMT inhibitors can be taken concurrently with the levodopa-carbidopa combination because a different enzyme is involved.
The agent tolcapone (Tasmar) is a very potent COMT inhibitor with high lipid solubility. Thus it crosses the blood-brain barrier well. In phase III trials of tolcapone as adjunctive therapy to levodopa-carbidopa, clinical efficacy was achieved at dosages of 100 to 200 mg three times daily. The addition of tolcapone allowed a 25 percent reduction in the levodopa dosage.29
The U.S. Food and Drug Administration (FDA) recently issued a warning concerning reports of hepatocellular injury and acute fulminant liver failure associated with the use of tolcapone. The boxed warning added to the product label emphasizes that tolcapone should be used as an adjunct only in patients being treated with levodopa-carbidopa who are experiencing symptom fluctuations and are not responding satisfactorily to other adjunctive therapies or who are not appropriate candidates for such therapies. When tolcapone is prescribed, informed consent is required, including patient education about the restricted indications and the symptoms of hepatic dysfunction. Biweekly blood tests of hepatic function must be performed, and any evidence of liver injury should be reported to the FDA through MedWatch (800-FDA-1088).
Entacapone, a less potent COMT inhibitor than tolcapone, is currently undergoing trials as adjunctive therapy with levodopa. The drug may soon be released in the United States. Entacapone does not cross the blood-brain barrier well, and it has a very short half-life. Monitoring of liver function is recommended with this agent but thus far is not required.
In clinical trials, both tolcapone and entacapone have been found to be effective against the “wearing off ” that occurs with levodopa. As a result, patients can be managed with less frequent dosing. Patients receiving a COMT inhibitor report increased energy levels, better sleep and improved functioning in terms of the activities of daily living.
In addition to adverse effects related to the enhancement of levodopa, patients treated with COMT inhibitors may experience diarrhea, and their urine may become bright yellow.
OTHER PHARMACOLOGIC APPROACHES
Trihexyphenidyl (Artane) or benztropine (Cogentin) may be prescribed as adjunctive therapy to levodopa. Either of these anti-cholinergic drugs may be helpful in managing significant tremor early in the course of Parkinson's disease. Anticholinergic agents have been used with mixed results in patients with essential tremor, dystonias and certain dyskinesias. Unfortunately, elderly patients are often unable to tolerate the side effects of these drugs, which include cognitive impairment, dry mouth and urinary retention. In recent years, the use of anticholinergic drugs in Parkinson's disease has been limited to patients with severely disabling tremor.30 However, it is extremely difficult to withdraw these drugs in patients who have been taking them regularly.
Other drugs that affect motor tone and control, including benzodiazepines, anticonvulsant drugs and antispasmodic agents (e.g., baclofen [Lioresal]), should be used with caution in patients with Parkinson's disease. For example, baclofen is effective in managing hemifacial spasm and possibly blepharospasm, but it may lower the seizure threshold and produce muscle weakness.
BOTULINUM TOXIN
Botulinum toxin in the forms produced by certain strains of Clostridium botulinum is available as an injectable drug for the treatment of certain conditions characterized by involuntary hyperactivity of muscles. Botulinum toxin type A (Botox) has been in use in the United States for more than 10 years, and botulinum toxin type B is soon to be released.
Very small quantities of the toxin are injected directly into the hyperactive muscles under electromyographic guidance. This treatment has been beneficial in patients with dystonia, hemifacial spasm, blepharospasm, spasmodic torticollis, dysphonia, and spasticity from stroke, multiple sclerosis and other causes. It is also useful for alleviating the blepharospasm and limb dystonias that are frequently associated with Parkinson's disease even when other manifestations are successfully controlled by medications.31
Surgery for Parkinson's Disease
At one time, surgery was reserved for use in patients with early-onset Parkinson's disease who became disabled in their prime working years. However, techniques have advanced so rapidly that surgery is now considered an option even in elderly patients as long as they meet medical screening criteria, including failure to respond to available medications and absence of cardiopulmonary risk factors for surgery. It is essential to select a neurosurgeon who is part of a movement disorders team with considerable experience in performing the surgical procedures used to treat Parkinson's disease.
THALAMOTOMY
Thalamotomy, introduced even before levodopa became available in the 1960s, effectively reduces tremor and sometimes rigidity on the contralateral side.32 Unfortunately, bilateral thalamotomy may result in speech, swallowing and visual deficits.
THALAMIC STIMULATION
Thalamic stimulation can reproduce the benefits of thalamotomy without the risk of irreversible tissue loss, because no physical lesion is created. The stimulation procedure involves the insertion of an electrode wire into the ventral intermediate nucleus (VIM) of the thalamus under electrophysiologic guidance. The other end of the wire is connected to a pulse generator that resembles a cardiac pacemaker in size and shape. This generator is implanted subcutaneously in the pectoral area.
The patient activates the unit by passing a small (2-in) hand-held magnet over the chest. Within seconds to minutes, the tremor resolves on the contralateral side, and the patient is free to move without tremor until the magnet is passed over the unit again to deactivate the pulse generator. Although bradykinesia and rigidity usually remain, thalamic stimulation can produce dramatic results in the patient whose primary disabling feature is tremor, whether caused by Parkinson's disease or essential tremor.33
PALLIDOTOMY
Pallidotomy is a procedure in which a portion of the globus pallidus is lesioned permanently. The procedure has significant associated risks, including visual field deficits and hemiparesis (because of the proximity of the medial pallidum to the optic tracts and internal capsule). Bilateral procedures have a greater than 15 percent complication rate and are associated with postoperative neuropsychiatric deficits in some patients. If pallidotomy is performed under careful electrophysiologic monitoring and restricted to one side (preferably the nondominant side), the results are more favorable. Compared with thalamic procedures, pallidotomy is less beneficial for tremors and more beneficial for dyskinesias.34
OTHER TREATMENTS
Other Therapeutic Strategies
Slowness of gait, poor postural reflexes, involuntary movements and orthostatic hypotension contribute to the falls frequently experienced by patients with Parkinson's disease, especially later in the course of the disorder. Measures to reduce the risk of falls include wearing leather rather than rubber-soled shoes and removing throw rugs in the patient's home. When possible, pharmacotherapy may also need to be adjusted.
Physical therapy can be helpful. Particular emphasis should be given to upright posture, gait training and extension exercises for the neck, trunk and legs. A formal exercise program should be taught to the patient (and to the caregiver, if applicable). The patient should perform daily home exercises and receive “refresher” exercise instruction every six to 12 months.
Nutrition is another common problem in patients with Parkinson's disease. Pharyngeal and gastrointestinal musculature often become impaired in this movement disorder, and dry mouth and gastrointestinal disturbances may occur as side effects of prescribed medications. Consequently, patients should be offered both speech therapy and nutritional supplements.
Sleep disturbances are also common in patients with Parkinson's disease. The proximity of the substantia nigra to the sleep and arousal centers in the brain stem may be significant to the occurrence of these problems. Sleep disturbances are usually managed with the adjustment of scheduled medications, dietary modifications and sleep hygiene practices. If sleep problems persist, referral to a physician with specialized training in sleep physiology is advised to determine if the patient has a treatable sleep disorder such as sleep apnea, myoclonus, periodic leg movements or rapid-eye-movement (REM) sleep disorder.12
Psychologic well-being is an important issue in patients with movement disorders. Patients may easily become depressed because they are unable to perform physically. Sexual function is frequently impaired because of associated autonomic nervous system dysfunction. With depression, libido may also decline.
In the later stages of some degenerative conditions, including idiopathic Parkinson's disease, dementia may develop, and patients may eventually have to be institutionalized.38 An atypical neuroleptic agent such as clozapine (Clozaril) or olanzapine (Zyprexa) can be useful in patients with severe hallucinations or psychosis.39 Some of the other symptoms of dementia can be alleviated with donepezil (Aricept) or tacrine (Cognex), but this condition currently has no cure. Dementia is increasingly recognized as a risk factor for shortened survival in patients with Parkinson's disease.40
Community Resources
A number of organizations provide support and medical information on Parkinson's disease in lay terms, largely through the efforts of patients and their families (Table 5). Internet sites for both patients and health care professionals are offered by various universities and other organizations. On-line question-and-answer “news groups” have proliferated on the Internet (Table 6). These sources can provide answers to questions about potential legal issues, such as the operation of motor vehicles by persons with Parkinson's disease, and can also provide assistance to caregivers.
| American Parkinson's Disease Association |
| 1250 Hylan Blvd., Suite 4B, Staten Island, NY 10305 |
| Telephone: 718-981-8001 or 800-223-2732 |
| National Parkinson Foundation, Inc. |
| 1501 N.W. Ninth Ave., Miami, FL 33136 |
| Telephone: 800-327-4545 |
| The Parkinson's Disease Foundation |
| 710 W. 158th St., New York, NY 10032 |
| Telephone: 212-305-3480 or 800-457-6676 |
| United Parkinson Foundation |
| 833 W. Washington Blvd., Chicago, IL 60607 |
| Telephone: 312-733-1893 |
| International Tremor Foundation |
| 7046 W. 105th St., Overland Park, KS 66212 |
| Telephone: 913-341-3880 |
| American Parkinson Disease Association |
| http://www.apdaparkinson.com |
| Awakenings (Parkinson's disease forum and information) |
| http://www.parkinsonsdisease.com |
| National Institute of Neurologic Disorders and Stroke: Experimental Therapeutics Branch |
| http://etb.ninds.nih.gov |
| National Parkinson Foundation, Inc. |
| http://www.parkinson.org |
| The Parkinson's Disease Foundation |
| http://www.pdf.org |
| The Parkinson's Disease Questionnaire (user manual) |
| http://hsru.dphpc.ox.ac.uk/pdqmanual.htm |
| Parkinson's Disease Interest Group (law forum and other information) |
| http://www.santel.lu/SANTEL/diseases/parkins.html |
| Ability: Parkinson's Disease |
| http://www.ability.org.uk/parkinso.html |
| Meditopia! (articles on Parkinson's disease) |
| http://meditopia.com/dis/park/otpark.html |