
Am Fam Physician. 2020;102(11):679-691
Related letter: Using DaTscan to Diagnose Parkinson Disease
Related letter: Ultrasound Subthalamotomy for the Management of Parkinson Disease
Parkinson disease is a progressive neurodegenerative disorder with significant morbidity and mortality. Most patients consult with their primary care physician about Parkinson disease symptoms before seeking care from a specialist. The diagnosis of Parkinson disease is clinical, and key disease features are bradykinesia, rigidity, and tremor. The main diagnostic signs of Parkinson disease are motor symptoms; however, Parkinson disease is also associated with nonmotor symptoms, including autonomic dysfunction, depression, and hallucinations, which can make the initial diagnosis of Parkinson disease difficult. Disease progression is variable and clinical signs cannot be used to predict progression accurately. Therapies, including levodopa, have not demonstrated the ability to slow disease progression. Motor symptoms are managed with carbidopa/levodopa, monoamine oxidase-B inhibitors, and nonergot dopamine agonists. Prolonged use and higher doses of levodopa result in dyskinesias and motor symptom fluctuations over time. Deep brain stimulation surgery is performed for patients who do not achieve adequate control with levodopa therapy. Deep brain stimulation is most effective for significant motor fluctuations, dyskinesias, and tremors. Nonmotor symptom therapies target patient-specific conditions during the disease course. Interdisciplinary team care can alleviate multiple symptoms of Parkinson disease.
Parkinson disease is a progressive neurodegenerative disorder with significant morbidity and mortality. Approximately 60,000 people are diagnosed with Parkinson disease each year in the United States; it is the 14th leading cause of death, with most patients dying from complications of the disease.1 Most patients consult with their primary care physician about Parkinson disease symptoms before seeking care from a specialist. Primary care physicians are often the most accessible to patients and caregivers coping with this disease.
Pathophysiology
Parkinson disease is characterized by a progressive loss of dopamine-producing neurons in the basal ganglia, particularly in the substantia nigra,2 and development of Lewy bodies in the dopaminergic neurons. Lewy bodies are the pathologic feature of Parkinson disease.3 However, Lewy bodies are nonspecific for Parkinson disease and are found in multiple neurodegenerative diseases; therefore, Parkinson disease represents a disease syndrome with different clinical subtypes.4
Diagnosis
The diagnosis of Parkinson disease is clinical, and key features include bradykinesia, rigidity, and tremor. The most common presenting symptom in Parkinson disease is a unilateral resting tremor, often localized to the distal muscles of the hand, causing a pill-rolling motion. Some patients note an internal tremulousness sensation before the manifestation of the pill-rolling tremor.5 Rigidity usually starts on the side of the body affected by the tremor and can affect gait, contribute to muscle pain, and impair posture. Cogwheel rigidity, in which affected muscles ratchet or alternate rapidly between rigidity and relaxation when moved passively, is the most common type in Parkinson disease. A small number of patients with Parkinson disease present with lead pipe rigidity, in which affected muscles stay rigid throughout the passive motion.
The main diagnostic signs of Parkinson disease are motor symptoms; however, nonmotor symptoms are also common and debilitating. Nonmotor symptoms that often present before motor symptoms include rapid eye movement sleep disorder, depression, constipation, fatigue, and olfactory dysfunction. A large survey of patients with Parkinson disease found that almost all patients reported nonmotor symptoms, with psychiatric symptoms occurring most often.6 Associated nonmotor symptoms that can occur later in the disease can include autonomic dysfunction such as orthostatic hypotension and urinary dysfunction, which can impact quality-of-life and level-of-care issues for patients. Some nonmotor symptoms such as dementia and psychosis occur with advanced Parkinson disease but are notably debilitating.
A physical examination should include assessment for decreased spontaneous or uncontrollable movements, tremors, or flat or masked facial expressions. A gait examination should assess for shuffling gait, stooped posture, en bloc turns, freezing (i.e., sudden transient arrests of movement), or postural instability. Bradykinesia, or the overall slowing of movement, includes decreased manual dexterity, shuffling steps, freezing gait, and festinating gait (i.e., involuntary gait acceleration). For a video illustrating common Parkinson disease movements, see https://www.youtube.com/watch?v=pFLC9C-xH8E. The neurologic examination should focus on muscle tone (e.g., cogwheel, lead pipe) and bradykinesia through rapid alternating movements testing.
Misdiagnosis often occurs because of the multiple symptoms associated with Parkinson disease and the notable clinical overlap with other diseases. Careful examination of the tremor can differentiate between Parkinson disease and other causes. Whole hand tremor is usually an essential tremor or it can be attributed to cerebellar causes. Features supporting a diagnosis of Parkinson disease are asymmetric clinical motor presentation, gradual onset, and bradykinesia. Motor symptom response to levodopa also supports the diagnosis. Insidious progression of symptoms and postural instability are hallmarks of later stages of Parkinson disease. Factors indicating another diagnosis are rapid disease progression, early or symmetric bilateral body involvement, and inadequate response to levodopa.7 Although upper extremity tremor is the more common presenting symptom in Parkinson disease, the development of lower extremity tremor favors a diagnosis of Parkinson disease over essential tremor.8,9 Essential tremor, progressive supranuclear palsy, drug-induced parkinsonism, and Lewy body dementia are often mistaken for Parkinson disease.
Pharmacologic Treatment
INITIAL DRUG THERAPY SELECTION FOR MOTOR SYMPTOMS
Guidelines recommend treating motor symptoms when they impact the functions of daily life or decrease quality of life.10–12 Treatment options for early Parkinson disease include carbidopa/levodopa (Sinemet, Rytary), monoamine oxidase-B (MAOB) inhibitors, nonergot dopamine agonists, anticholinergic agents, or amantadine.10–12 Table 1 summarizes the pharmacologic management of motor symptoms in Parkinson disease.10–19 First-line therapy for motor symptom management in Parkinson disease is carbidopa/levodopa because of its effectiveness in managing tremors, rigidity, and bradykinesias.10–12 Levodopa is the active component that crosses the blood-brain barrier, and carbidopa inhibits peripheral metabolism of levodopa.13 Levodopa is most effective when taken on an empty stomach; however, this can cause difficulty with medication tolerance.13 Challenges with the prolonged use of levodopa in Parkinson disease are motor fluctuations with dyskinesias (i.e., choreiform movements) during peak medication levels and freezing or “off effects” during lower levels. Continuous use may lead to more off periods, during which Parkinson disease symptoms return because of low dopamine levels, and decreased medication effectiveness per dosing interval.14–16,20,21 Patients with Parkinson disease can experience dystonia or pain from lack of levodopa or dyskinesias caused by levodopa administration.22
| Class or specific agent | Role in therapy | Dosage forms available | Dosing pearls | Adverse effects | Advantages | Disadvantages | Cost* for 30-day supply | |
|---|---|---|---|---|---|---|---|---|
| Amantadine (Gocovri, Osmolex ER) | Treatment of dyskinesias associated with carbidopa/levodopa (Sinemet, Rytary) therapy | Amantadine: 100-mg immediate-release tablets Gocovri: 68.5-mg and 137-mg extended-release capsules Osmolex ER: 129-mg, 193-mg, and 258-mg tablets | Immediate release: 100 mg 1 to 2 times per day (maximum dosage: 400 mg per day) Extended release: start with lowest dose 1 time per day and titrate up weekly based on symptoms Do not discontinue abruptly; taper over several weeks | Orthostasis, peripheral edema, hallucinations, delusions, paranoia, dizziness, livedo reticularis, abnormal dreams, altered cognition, insomnia, confusion, drowsiness, agitation, depression, suicidal ideation, anxiety | Most helpful for dyskinesias; add to levodopa therapy | Not ideal for older adults secondary to cognitive effects and psychosis | Amantadine: $20 Gocovri: NA Osmolex ER: $500 | |
| Anticholinergics | ||||||||
| Benztropine Trihexyphenidyl | Early treatment of motor symptoms, primarily tremor | Benztropine: 0.5-mg, 1-mg, and 2-mg tablets Trihexyphenidyl: 2-mg and 5-mg tablets | Benztropine: 0.5 mg 1 time per day at bedtime; titrate up by 0.5 mg weekly based on response and tolerability (maximum dosage: 6 mg per day) Administer in 2 to 4 divided doses with higher dosing Trihexyphenidyl: 1 mg per day; titrate up by 2-mg increments weekly based on symptoms (maximum dosage: 15 mg per day) Administer in 3 to 4 divided doses with higher dosing | Constipation, urinary retention, dry eyes, dry mouth, altered cognition, altered prolactin levels | Effective for managing tremors that are the predominant motor symptom | Not effective for bradykinesias or dyskinesias Adverse effect profile not well tolerated by older adults | Benztropine: $10 Trihexyphenidyl: $10 | |
| Dopamine agonists | ||||||||
| Nonergot: pramipexole (Mirapex), ropinirole (Requip XL), rotigotine (Neupro) | Early treatment of motor symptoms that are not too disruptive and an additive to carbidopa/levodopa therapy to minimize effects of off periods | Pramipexole and Mirapex: 0.125-mg, 0.25-mg, 0.5-mg, 0.75-mg, 1-mg, and 1.5-mg immediate-release tablets Pramipexole ER and Mirapex ER: 0.375-mg, 0.75-mg, 1.5-mg, 2.25-mg, 3-mg, 3.75-mg, and 4.5-mg tablets Ropinirole: 0.25-mg, 0.5-mg, 1-mg, 2-mg, 3-mg, 4-mg, and 5-mg immediate-release tablets Ropinirole ER and Requip XL: 2-mg, 4-mg, 6-mg, 8-mg, and 12-mg tablets Neupro: 1-mg, 2-mg, 3-mg, 4-mg, 6-mg, and 8-mg transdermal patches | Pramipexole and ropinirole: start with lowest dose 3 times per day Pramipexole ER and ropinirole ER: start with lowest dose 1 time per day May titrate up every 5 to 7 days as needed for symptom management Rotigotine transdermal patch: start with lowest dose applied 1 time per day May titrate up every 5 to 7 days Do not discontinue abruptly; taper over several weeks | Impulse control disorder, psychosis, hallucinations, delusions, dyskinesias, lower extremity edema, constipation, nausea, somnolence, sleep attacks, insomnia, dizziness, orthostasis, hypotension, melanoma Pramipexole: heart failure exacerbation | Good initial option to treat motor symptoms but not as effective as levodopa therapy Lower risk of motor complications with prolonged use compared with levodopa therapy | High risk of impulse control disorder May require decrease in dose or stopping completely to manage impulse control disorder Inquire about sleep attacks and excessive daytime somnolence Has potential to exacerbate dyskinesias Monitor for melanoma on regular basis | Pramipexole: $10 Mirapex: $220 Pramipexole ER: $80 Mirapex ER: $650 Ropinirole: $20 Ropinirole ER: $20 Requip XL: $25 Neupro: $700 | |
| Apomorphine (Apokyn) | Apomorphine for severe freezing episodes | Apokyn subcutaneous injection: 30 mg per 3 mL | Apomorphine: start with lowest dose possible and may titrate as needed every few days to effect; pen is marked in mL, not mg, which makes it prone to dosing errors; must have first dose administered in office; antiemetic should be administered 3 days before test dose | Hypersensitivity reaction, severe hypotension, severe nausea, vomiting (premedicate with antiemetic trimethobenzamide [Tigan] before use), pulmonary fibrosis, somnolence, dyskinesias, QTc prolongation, confusion, altered cognitive function | Works quickly to resolve freezing episodes | Initial test doses should be administered in the office and observed for at least 1 hour and up to 2 hours for response to off periods and safety (hypotension) Most patients will not take long-term because of the adverse effect profile | Apokyn: NA; only available through specialty pharmacies | |
| Catechol O-methyltransferase inhibitors | ||||||||
| Entacapone (Comtan) Tolcapone (Tasmar) Opicapone (Ongentys) | Additive to carbidopa/levodopa therapy to minimize effects of off periods; do not administer as monotherapy | Entacapone and Comtan: 200-mg tablets Also available as combination carbidopa/entacapone/levodopa (Stalevo): 12.5-mg/50-mg/200-mg, 18.75-mg/75-mg/200-mg, 25-mg/100-mg/200-mg, 31.25-mg/125-mg/200-mg, 37.5-mg/150-mg/200-mg, 50-mg/200-mg/200-mg tablets Tolcapone: 100-mg tablets Opicapone: 50-mg tablets; FDA approved in April 2020 but NA in U.S. market | Entacapone: 200 mg with each dose of carbidopa/levodopa up to 8 times per day (maximum dosage: 1,600 mg per day) Opicapone: 50 mg once nightly; dosage decrease with moderate hepatic dysfunction to 25 mg 1 time per day | Orthostatic hypotension, potential to worsen dyskinesias when added to levodopa therapy, urine discoloration (e.g., dark orange or brown), constipation, fatigue | Increases effectiveness (reduces off effects) of carbidopa/levodopa therapy | Tolcapone associated with fulminant hepatic failure; use should be limited | Entacapone: $35 Comtan: $660 Tolcapone: $1,425 Tasmar: $11,150† Carbidopa/levodopa/entacapone: $55 Stalevo: $100 Opicapone: NA in U.S. market | |
| Adenosine A2A antagonists | ||||||||
| Istradefylline (Nourianz) | Additive to carbidopa/levodopa therapy to minimize effects of off periods; do not administer as monotherapy | Nourianz: 20-mg and 40-mg | Start with 20 mg 1 time per day; may increase to 40 mg based on response and tolerability | Dyskinesias when added to carbidopa/levodopa therapy, dizziness, constipation, nausea, hallucinations, insomnia, impulse control disorder, psychosis | Increases effectiveness (reduces off effects) of carbidopa/levodopa therapy | Cost because it will only be available as brand-name medication | Nourianz: $1,500 | |
| Carbidopa/levodopa (Sinemet; Rytary; Inbrija; Duopa) | First choice for management of motor symptoms | Carbidopa/levodopa and Sinemet: 10-mg/100-mg, 25-mg/100-mg, and 25-mg/250-mg immediate-release and orally disintegrating tablets Carbidopa/levodopa ER: 25-mg/100-mg and 50-mg/200-mg tablets Rytary immediate and extended release combined: 23.75-mg/95-mg, 36.25-mg/145-mg, 48.75-mg/195-mg, 61.25-mg/245-mg capsules Inbrija: 42 mg powder for inhalation Duopa: 4.63-mg/20-mg per mL enteral suspension | Carbidopa/levodopa is most effective on an empty stomach Start with lowest immediate-release dose 3 times per day Once a patient is taking 3 of the 25-mg/100-mg tablets 3 times per day, increasing the dose further adds no additional benefit and more frequent dosing intervals should be considered May require dosing over time with a higher dose 4 to 5 times per day Controlled-release dose converted from immediate-release dosing equivalents administered 2 times per day; controlled release has sporadic absorption in some patients Rytary: start with lowest dose 3 times per day; may require higher, more frequent dosing (4 to 5 times per day) over time Inbrija: 84 mg as needed for off periods up to 5 times per day Duopa: dose to be administered based on conversion of immediate-release dosing (maximum dosage: 2,000 mg per day) administered over 16 hours; nighttime symptoms are managed with immediate-release levodopa Dose and frequency adjustments are required to manage dyskinesias and off periods over time Do not withhold therapy for long periods, even if the patient is directed to take nothing by mouth, because it could result in akathisia and neuroleptic malignant syndrome Do not discontinue abruptly; taper over several weeks | Hallucinations, delusions, dyskinesias, lower extremity edema, nausea, somnolence, dizziness, orthostasis, depression, suicidal ideation Inbrija: cough, upper respiratory infection Duopa: site complications, abdominal pain, infections | Immediate-release formulation is first choice for treatment of motor symptoms Rytary may improve a patient's on time (when medication is effectively controlling symptoms), but dyskinesias similar to immediate release Inbrija may help with freezing and off periods that are unpredictable Duopa may improve on time and severe dyskinesias | High risk of developing motor complications from use Prone to off periods as disease progresses, which may present as anxiety, akathisia, apathy, depression, bradykinesias, and freezing | Carbidopa/levodopa: $9 Carbidopa/levodopa orally disintegrating tablet: $37 Carbidopa/levodopa ER: $30 Rytary: $352 Inbrija: NA Duopa: NA | |
| Monoamine oxidase-B inhibitors | ||||||||
| Rasagiline (Azilect) Selegiline (Zelapar) Safinamide (generic not currently available in United States; Xadago) | Early treatment of motor symptoms that are not too disruptive (rasagiline and selegiline only) and an additive to carbidopa/levodopa therapy to minimize effects of off periods (all) | Rasagiline and Azilect: 0.5-mg and 1-mg tablets Selegiline: 5-mg tablets and capsules Zelapar: 1.25-mg orally disintegrating tablet Xadago: 50-mg and 100-mg tablets | Rasagiline: 1 mg 1 time per day Selegiline: 5 mg 2 times per day (maximum dosage: 10 mg per day) Xadago: 50 mg 1 time per day; may increase in 2 weeks to maximum dosage of 100-mg 1 time per day based on symptoms | Nausea, dizziness, hallucinations, dry mouth, vivid dreams, headaches, dyskinesias when used with a dopamine agonist or carbidopa/levodopa therapy Rasagiline: increased risk of melanoma | Improves on time when added to levodopa therapy Generally well tolerated | Not as effective as carbidopa/levodopa therapy for motor symptoms Limited risk of serotonin syndrome with other serotonergic medications but is not risk-free | Rasagiline: $70 Azilect: $825 Selegiline: $40 Zelapar: $2,250 Xadago: $825 | |
One-third to one-half of patients being treated with levodopa develop dyskinesias within four to six years of initiation, and 100% experience dyskinesias after 20 years.14,15 Risk factors for dyskinesias include young age at the onset of Parkinson disease, longer duration of Parkinson disease, increased disease severity, higher levodopa doses, and prolonged levodopa use.15,17,21 Carbidopa/levodopa is the first-line choice for initial therapy in adults older than 65 years and patients with significant motor dysfunction at diagnosis.10–12 Table 2,10–12 Table 3,10–12 and Figure 110–12 describe treatment considerations for the management of motor symptoms in Parkinson disease.
| Treatment options | Considerations |
|---|---|
| Amantadine | Limited use for patients younger than 65 years who only have tremor; limited effectiveness and significant adverse effect potential |
| Anticholinergics | Limited use for patients younger than 65 years who only have tremor |
| Carbidopa/levodopa | First-line therapy to manage motor symptoms Potential to develop motor complications and dyskinesias with use; therefore, first-line use in early disease limited to adults 65 years and older and patients with significant motor symptoms impacting quality of life |
| Monoamine oxidase-B inhibitors | Considered first-line therapy for patients younger than 65 years with mild motor symptoms at time of diagnosis |
| Nonergot dopamine agonists | Considered first-line therapy for patients younger than 65 years with mild motor symptoms at time of diagnosis Avoid use in patients with a history of psychosis and addiction |
| Treatment options | Considerations |
|---|---|
| For the treatment of motor fluctuations: Consider adjusting dose or dosing interval of carbidopa/levodopa first; if not effective, consider adding therapy If not prescribed already, add monoamine oxidase-B inhibitors, nonergot dopamine agonists, catechol O-methyltransferase inhibitors, or istradefylline (Nourianz) or Consider changing oral carbidopa/levodopa administration during the day to intrajejunal carbidopa/levodopa | Monoamine oxidase-B inhibitors, nonergot dopamine agonists, or catechol O-methyltransferase inhibitors are generally added first unless contraindicated Istradefylline is the newest drug to the market and is the most expensive Intrajejunal carbidopa/levodopa is reserved for patients resistant to other treatment options |
| For the treatment of dyskinesias: | Adverse effect profile of amantadine is not well tolerated; cannot be used long-term |
| Consider decreasing dose of carbidopa/levodopa, which may necessitate adjusting the dosing frequency to offset waning with a lower dose May need to consider adding amantadine | |
| For the treatment of freezing (severe episodes): Consider apomorphine (Apokyn), intranasal carbidopa/levodopa, or low-dose immediate-release carbidopa/levodopa | Apomorphine works quickly but is poorly tolerated Intranasal carbidopa/levodopa does not work as quickly but is well tolerated Low-dose immediate-release carbidopa/levodopa works slowly but is well tolerated |
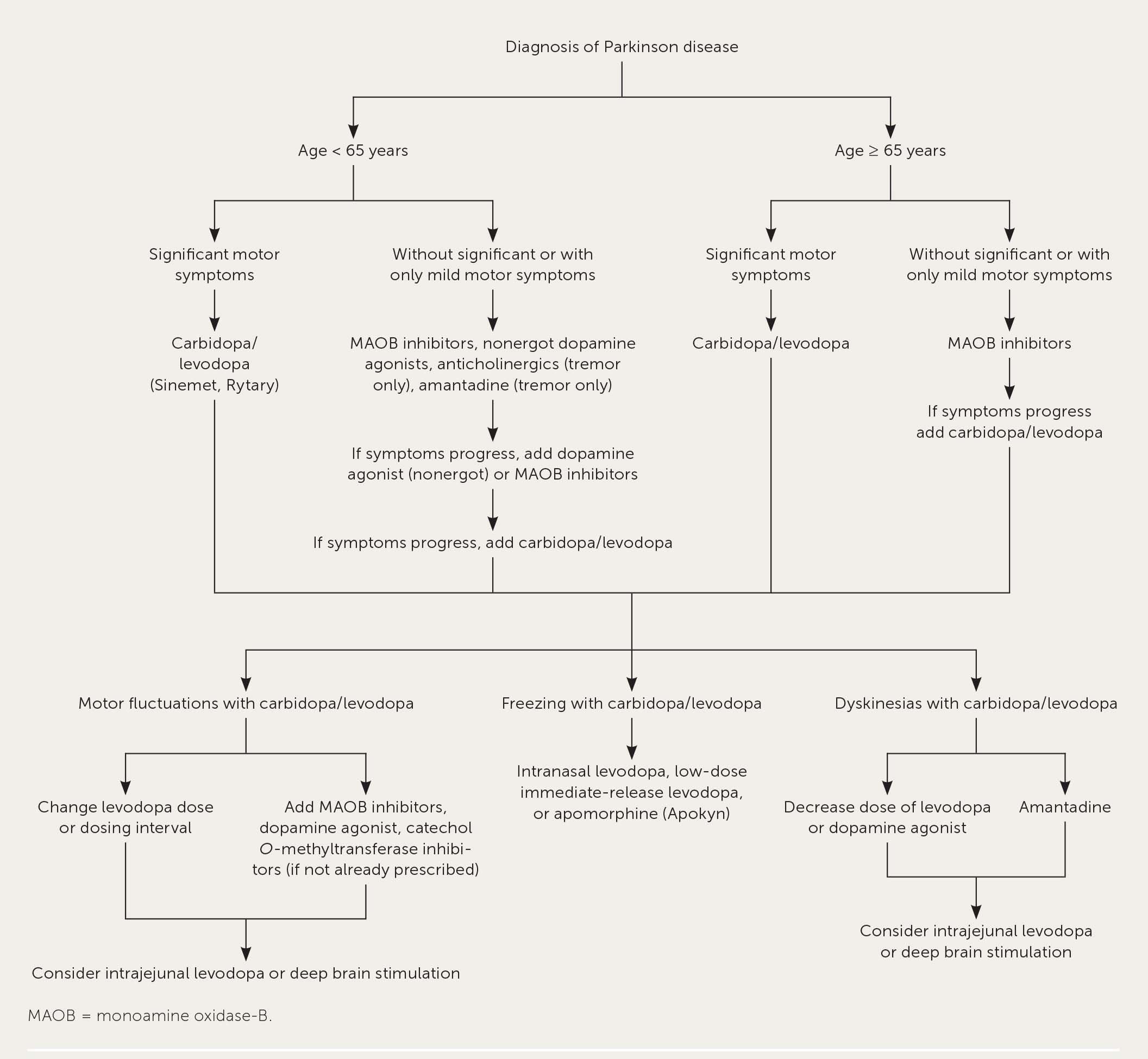
MAOB inhibitors are considered first-line therapies in younger patients and those with mild motor symptoms at diagnosis.10–12,21 MAOB inhibitors (i.e., selegiline [Zelapar], rasagiline [Azilect], and safinamide [Xadago]), and nonergot dopamine agonists (i.e., pramipexole [Mirapex], ropinirole [Requip XL], and rotigotine [Neupro]) are not as effective as carbidopa/levodopa for motor symptoms, but they do not cause the motor fluctuations and dyskinesias associated with levodopa.14 Physicians should be aware of possible serotonin syndrome when using MAOB inhibitors with other serotonergic agents. Selective MAOB inhibitors are less likely to cause serotonin syndrome than are nonselective MAOB inhibitors. Rasagiline is the preferred MAOB inhibitor because of its safety profile.14,16 [corrected]
Nonergot dopamine agonists may be more effective for the management of motor symptoms than MAOB inhibitors, but they have a higher likelihood of causing somnolence, hallucinations, and impulse control disorder. Patients with psychiatric disorders should avoid dopamine agonists if possible. All nonergot dopamine agonists have similar effectiveness and adverse effect profiles; therefore, drug selection is based on cost, insurance coverage, and the preferred administration route. Ergot dopamine agonists (i.e., bromocriptine [Parlodel]) should be avoided in Parkinson disease management because of the association with pulmonary fibrosis and heart valve issues.14,16
Anticholinergic agents (i.e., benztropine and trihexyphenidyl) and amantadine can be initial therapy for patients younger than 65 years with tremors only. Because of significant adverse effects and limited effectiveness, these medications are reserved for certain patients with early Parkinson disease.16,20
PROGRESSIVE MOTOR SYMPTOMS
Multiple medications are needed to manage motor symptoms as Parkinson disease progresses. Medications are typically added to the existing regimen unless there is a concern for adverse effects with medications such as dopamine agonists in older adults and anticholinergics. Medication selection or adjustment depends on symptoms, patient characteristics (e.g., preexisting psychosis or hallucinations, depression, impulse control disorder, hypotension), and preferences. MAOB inhibitors, dopamine agonists, and carbidopa/levodopa are added to initial therapy for motor symptom management with disease progression.10–14,20 After either an MAOB inhibitor or a dopamine agonist is initiated, the other may be added before levodopa to minimize motor fluctuations and dyskinesias. As motor symptoms progress, levodopa should be considered to minimize symptom burden and maximize quality of life.10–12
Levodopa should be adjusted to address progressive motor symptoms through increasing doses (i.e., administer lowest doses possible to manage symptoms) or adding dosing intervals; however, when dopamine agonists or catechol O-methyltransferase (COMT) inhibitors are added, levodopa doses should be decreased up to 30% to minimize adverse effects.10–12 Immediate-release carbidopa/levodopa is preferred because of more predictable pharmacokinetics and product availability. Controlled-release products may be considered for certain patients who have difficulty adhering to frequent dosing intervals. However, higher doses are usually needed for controlled-release formulations compared with immediate-release formulations because of erratic pharmacokinetics, resulting in dyskinesias, freezing, and off periods.2 Rytary is an immediate-release/extended-release product with a more consistent extended-release profile than older controlled-release formulations.18
Several medications can be added to manage the effects of levodopa during off periods.10–12,14–16,21 MAOB inhibitors, dopamine agonists, or COMT inhibitors may be added to levodopa if not already prescribed. One agent from each class should be added in a stepwise approach. The preferred COMT inhibitor is carbidopa/entacapone/levodopa (Stalevo) because of the safety profile and product availability.15 One agent in the COMT inhibitor class, tolcapone, is associated with fulminant hepatic failure; use should be limited.18 Istradefylline (Nourianz) is the newest drug on the market for the treatment of off-period effects.
In patients with advanced Parkinson disease who are experiencing wearing-off effects and are unresponsive to treatment, administering carbidopa/levodopa with an intrajejunal pump may be helpful. Pump therapy is reserved for patients experiencing more off effects and dyskinesias to carbidopa/levodopa over time because of the higher cost and complexity of administration.
For patients experiencing freezing episodes, several options exist such as apomorphine (Apokyn) subcutaneous injections, inhaled carbidopa/levodopa, and low-dose immediate-release carbidopa/levodopa. Apomorphine works quickly to resolve freezing but is poorly tolerated secondary to severe nausea, vomiting, and orthostasis. Inhaled carbidopa/levodopa is better tolerated than apomorphine but has a slower onset. Apomorphine and inhaled carbidopa/levodopa are costly. Immediate-release carbidopa/levodopa is well-tolerated and affordable but takes much longer to resolve freezing.
If levodopa-associated dyskinesias become too disruptive, the first approach should be to decrease the dose of levodopa or the dopamine agonist.21 However, decreased dosing often leads to more significant waning effects, which may require more frequent administration. Other options for the management of dyskinesias include changing levodopa administration to a pump during the day or adding amantadine.10–12,21,23 The adverse effect profile of amantadine can limit its long-term use.23
NONMOTOR SYMPTOMS
Unfortunately, the evidence base for managing nonmotor symptoms is limited.11,20,24–26 Table 4 summarizes the most common nonmotor symptoms and potential therapies to consider when treating a patient with Parkinson disease.11,24–26 Nonmotor symptoms of Parkinson disease should be reviewed and addressed at each visit.24
| Symptom | Agents for management | Considerations for use |
|---|---|---|
| Constipation | Probiotics Polyethylene glycol (Miralax) Lubiprostone (Amitiza) | Lifestyle modifications are first-line choice with diet, adequate fluid intake, and activity or exercise; most patients will need drug therapy in addition to lifestyle modifications Polyethylene glycol is a good first-line agent Administer lubiprostone for patients who do not respond to lifestyle modifications, polyethylene glycol, or probiotics Most patients with Parkinson disease need multiple agents to manage constipation as disease progresses |
| Daytime somnolence and sleep attacks | Modafinil (Provigil) | Review annually for effectiveness and adverse effects Should review dose of dopamine agonists because they can contribute to sleep attacks |
| Dementia | Acetylcholinesterase inhibitors | Rivastigmine (Exelon) has the most data on use in later stages of Parkinson disease No data support the effectiveness of memantine (Namenda) in Lewy body–associated dementia |
| Depression | Serotonin-norepinephrine reuptake inhibitors Selective serotonin reuptake inhibitors Tricyclic antidepressants | Use drug therapy in combination with cognitive behavior therapy Serotonin-norepinephrine reuptake inhibitors are preferred based on current data May have antidepressant effects from use of agents to manage motor symptoms (monoamine oxidase-B inhibitors, dopamine agonists) |
| Drooling | OnabotulinumtoxinA (Botox) injections, glycopyrrolate | Nonpharmacologic interventions (e.g., speech therapy) should be tried first |
| Erectile dysfunction | Sildenafil (Viagra) | — |
| Insomnia | Melatonin, ramelteon (Rozerem) | — |
| Orthostasis | Midodrine, fludrocortisone | Adjust hypertension medications and try nonpharmacologic lifestyle interventions first Adjust motor therapies for Parkinson disease when possible (e.g., dopamine agonists, anticholinergics) May consider adding drug therapy specifically for orthostasis if other options are ineffective |
| Psychosis | Quetiapine (Seroquel), clozapine (Clozaril), pimavanserin (Nuplazid) | Start with lower doses and titrate slowly because the patient may be more sensitive to effects (effectiveness and safety) Clozapine is reserved for patients who are intolerant or who have a poor response to other options because of the safety profile |
| Rapid eye movement sleep disorder | Clonazepam (Klonopin), melatonin | Start low and titrate slowly because the patient may be more sensitive to clonazepam effects (safety) Melatonin may be safer and better tolerated than clonazepam |
| Urinary incontinence | Solifenacin (Vesicare), mirabegron (Myrbetriq) | Start with lower doses and titrate slowly; monitor for urinary retention, dry mouth, and worsening of constipation with solifenacin Mirabegron takes 8 weeks to reach full effect; monitor for increases in blood pressure with mirabegron |
Nonpharmacologic Treatment
SURGERY
Deep brain stimulation (DBS) is the surgical implantation of an intracranial electrode device in the subthalamic nucleus or the globus pallidus interna.15 DBS should be used for patients who do not achieve adequate control of symptoms with levodopa. DBS is most effective for patients with significant motor fluctuations, dyskinesias, and tremors.27,28 Earlier referral is useful for patients with severe symptoms. DBS is not ideal for patients with dementia, untreated depression, severe postural instability, and atypical Parkinson disease.16 Potential adverse effects of DBS include stroke; infection; cognition changes; changing or worsening psychological symptoms; impacts on speech, gait, and vision; and new-onset parasthesias.15
PHYSICAL ACTIVITY
Patients should be encouraged to be physically active to their functional ability because exercise has been shown to improve functionality and motor skills.15 Community-based classes designed for patients with Parkinson disease, such as boxing programs and Parkinson disease–specific speech therapy programs, can help improve quality of life and possibly slow disease progression. Adequate hydration is necessary to avoid the common symptom of constipation.
DIET
Patients with Parkinson disease are at higher risk of sarcopenia and osteoporosis.16 Levodopa should be administered at least 30 to 45 minutes before a high-protein meal because levodopa competes with amino acids in the gut for transport to the brain.13 Adequate amounts of vitamin D and calcium should be consumed in the diet or via supplementation. Adequate protein and calorie intake can be difficult because of feeding challenges associated with tremors and rigidity, and decreased appetite from delayed gastrointestinal transit. At this time no data show that antioxidants are useful for the treatment of Parkinson disease.29
INTERPROFESSIONAL CARE
Patients with Parkinson disease often require an interprofessional care team to provide comprehensive care throughout the various stages of disease. Care from a multidisciplinary team improves motor scores and quality of life, and lowers depression scores.30 In addition to the patient's primary care physician and neurologist, members of the care team may include a social worker, physical therapist, occupational therapist, psychologist, pharmacist, dietitian, and speech therapist14 (eTable A).
| Member | Role |
|---|---|
| Dietitian | Reviews dietary intake and recommends strategies to improve intake of nutrients |
| Neurologist | Specializes in the treatment of Parkinson disease |
| Occupational therapist | Assists with improving self-care in activities of daily living and improving functionality for work and maintaining leisure activities |
| Pharmacist | Reviews medications on a continuous basis for prevention and identification of adverse drug events |
| Physical therapist | Assists with gait, balance, mobility, and fall issues |
| Primary care physician | Oversees total care of the patient, treats Parkinson disease and overall health |
| Psychologist | Assists with coping strategies and treatment of depression, anxiety, and psychosis |
| Social worker | Assists with transportation issues from limited mobility, financial burdens of therapies, and affordability of full-time care needs |
| Speech therapist | Assists with microphonia and swallowing issues |
Prognosis
Parkinson disease progression is variable, and there is currently no available method to predict how it will progress. No therapies, including levodopa, have demonstrated the ability to slow progression.14,20 A 2012 study showed approximately 77% of patients had poor outcomes (i.e., death, postural instability, or dementia) 10 years after disease onset.31 The transition from disease impairment (i.e., difficulty with activities but maintaining independence) to disability (i.e., loss of independence) happens between three and seven years after the onset of Parkinson disease.32 Risk factors for rapid motor function decline include advanced age and bradykinesia or rigidity as presenting symptoms. A prominent tremor at presentation may predict slower disease progression rates.7 Indicators of limited life expectancy and hospice eligibility for patients with Parkinson disease include swallowing issues, aspiration pneumonia, and weight loss attributed to anorexia and difficulty feeding.19 The prevalence of dementia in Parkinson disease is 40% and increases with the duration of disease and age of onset. Psychosis, most commonly auditory and visual hallucinations, and paranoid delusions occur in 20% to 40% of patients with Parkinson disease and are the most influential risk factors for a patient's placement in a nursing home.33
This article updates previous articles on this topic by Young34 ; Rao, et al.35 ; and Gazewood, et al.7
Data Sources: A PubMed search was completed using the key terms Parkinson disease, motor symptoms, nonmotor symptoms, dyskinesias, and motor fluctuations. The search included randomized controlled trials, clinical trials, reviews, meta-analyses, case reports, and evidence-based guidelines. Also searched were Essential Evidence Plus, the Cochrane database, UpToDate, DynaMed, the National Institute for Health and Care Excellence, the American Academy of Neurology, and International Parkinson and Movement Disorder Society guideline recommendations. Search dates: August 19, September 9, October 7, and November 18, 2019; and June 26, 2020.
