
Am Fam Physician. 1999;60(7):2012-2018
A more recent article on patellofemoral pain syndrome is available.
Patient information: See related handout on patellofemoral pain syndrome, written by the author of this article.
Managing patellofemoral pain syndrome is a challenge, in part because of lack of consensus regarding its cause and treatment. Contributing factors include overuse and overload of the patellofemoral joint, biomechanical problems and muscular dysfunction. The initial treatment plan should include quadriceps strengthening and temporary activity modification. Additional exercises may be incorporated as dictated by the findings of the physical examination. Footwear should be closely evaluated for quality and fit, and the use of arch supports should be considered.
Patellofemoral pain syndrome can be defined as retropatellar or peripatellar pain resulting from physical and biochemical changes in the patellofemoral joint. It should be distinguished from chondromalacia, which is actual fraying and damage to the underlying patellar cartilage. Patients with patellofemoral pain syndrome have anterior knee pain that typically occurs with activity and often worsens when they are descending steps or hills. It can also be triggered by prolonged sitting. One or both knees can be affected. Consensus is lacking regarding the cause and treatment of the syndrome.1
Pathophysiology and Etiology
The patella articulates with the patellofemoral groove in the femur. Several forces act on the patella to provide stability and keep it tracking properly (Figure 1).
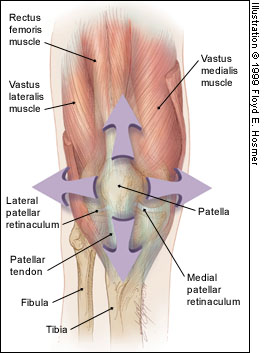
A common misconception is that the patella only moves in an up-and-down direction. In fact, it also tilts and rotates, so there are various points of contact between the undersurface of the patella and the femur.2,3 Repetitive contact at any of these areas, sometimes combined with maltracking of the patella that is often not detectable by the naked eye, is the likely mechanism of patellofemoral pain syndrome. The result is the classic presentation of retropatellar and peripatellar pain. This pain should not be confused with pain that occurs directly on the patellar tendon (patellar tendonitis).
Many theories have been proposed to explain the etiology of patellofemoral pain. These include biomechanical, muscular and overuse theories. In general, the literature and clinical experience suggest that the etiology of patellofemoral pain syndrome is multifactorial.
OVERUSE AND OVERLOAD
Because bending the knee increases the pressure between the patella and its various points of contact with the femur, patellofemoral pain syndrome is often classified as an overuse injury.4–8 However, a more appropriate term may be “overload,” because the syndrome can also affect inactive patients. Repeated weight-bearing impact may be a contributing factor, particularly in runners.3 Steps, hills and uneven surfaces tend to exacerbate patellofemoral pain. Once the syndrome has developed, even prolonged sitting can be painful (“movie-goer's sign”) because of the extra pressure between the patella and the femur during knee flexion.
BIOMECHANICAL PROBLEMS AND MUSCULAR DYSFUNCTION
Pes Planus (Pronation). The terms “flat feet” and “foot pronation” are often used interchangeably. Technically speaking, foot pronation is a combination of eversion, dorsiflexion and abduction of the foot. This condition often occurs in patients who lack a supportive medial arch (Figure 2). Foot pronation causes a compensatory internal rotation of the tibia or femur (femoral anteversion)11 that upsets the patellofemoral mechanism. This is the premise behind using arch supports or custom orthotics in patients with patellofemoral pain.

Pes Cavus (High-Arched Foot, Supination). Compared with a normal foot, a high-arched foot provides less cushioning for the leg when it strikes the ground. This places more stress on the patellofemoral mechanism, particularly when a person is running.3 Proper footwear, such as running shoes with extra cushioning and an arch support, can be helpful. (It is preferable to purchase such footwear from a reputable athletic shoe store with knowledgeable staff.)
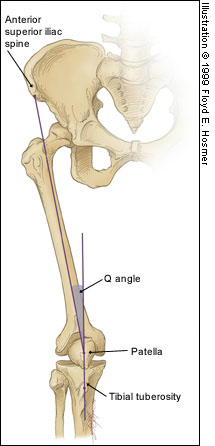
Q Angle. Although some investigators believe that a “large” Q angle (Figure 3) is a predisposing factor for patellofemoral pain, others question this claim. One study12 found similar Q angles in symptomatic and non-symptomatic patients. Another study6 compared the symptomatic and asymptomatic legs in 40 patients with unilateral symptoms and found similar Q angles in each leg. Furthermore, “normal” Q angles vary from 10 to 22 degrees,3 depending on the study, and measurements of the Q angle in the same patient vary from physician to physician.13 Therefore, the physician should be wary of placing too much emphasis on such biomechanical “variants,” as this can lead patients to believe that nothing can be done about their pain.
Muscular Causes. The potential muscular causes of patellofemoral pain can be divided into “weakness” and “inflexibility” categories (Table 1).3,4,6,7,9–11,14–23 Weakness of the quadriceps muscles is the most often cited area of concern. However, each potential cause should be evaluated and addressed appropriately to help guide conservative care.
| Etiology | Pathophysiology |
|---|---|
| Weakness of the quadriceps | The “quads” include the vastus medialis, vastus medialis obliquus (VMO), vastus intermedius, vastus lateralis and rectus femoris. Weakness may adversely affect the patellofemoral mechanism. Quad-muscle strengthening is often recommended.3,4,7,9,10,14–17 |
| Weakness of the medial Quadriceps, specifically VMO dysplasia | Weakness of the VMO allows the patella to track too far laterally. Although the role of the VMO is controversial,18–20 VMO strengthening is often recommended.6,7,11,15,16 However, the VMO is a difficult muscle to isolate,21 and most patients find general quadriceps strengthening easier to accomplish. |
| Tight iliotibial bands | A tight iliotibial band places excessive lateral force on the patella and can also externally rotate the tibia, upsetting the balance of the patellofemoral mechanism.22,23 This problem can lead to excessive lateral tracking of the patella. |
| Tight hamstring muscles | The hamstring muscles flex the knee. Tight hamstrings place more posterior force on the knee, causing pressure between the patella and femur to increase.7,15,16 |
| Weakness or tightness of the hip muscles (adductors, Abductors, external rotators) | The VMO originates on the adductor magnus tendon. This is the anatomic basis for recommending adductor strengthening.11,14,16 Abductor (gluteus medius) strengthening helps to stabilize the pelvis. Dysfunction of the hip external rotators results in compensatory foot pronation; a simple stretch can improve muscular efficiency.4 |
| Tight calf muscles | Tight calves can lead to compensatory foot pronation and, like tight hamstrings, can increase the posterior force on the knee.11,15,16 |
Treatment
A review of the literature yields few quality randomized, controlled trials on the treatment of patellofemoral pain syndrome.1,24 Prospective long-term follow-up studies provide the most useful data.8–10,25,26 Until long-term randomized, controlled clinical trials are conducted, the treatment of patellofemoral pain syndrome must be guided by the available literature and clinical experience.
EXERCISES AND PHYSICAL THERAPY
Exercises for patellofemoral pain are based on the muscular causes listed in Table 1.3,4,6,7,9–11,14–23 Quadriceps strengthening is most commonly recommended because the quadricep muscles play a significant role in patellar movement. Hip, hamstring, calf and iliotibial band stretching may also be important. The decision to incorporate these additional exercises depends on an accurate physical examination. (Exercises used in the treatment of patellofemoral pain are illustrated in a patient information handout that follows this article.)
Dedicated patients can often manage physical therapy on their own, with 20 minutes per day being a reasonable expectation. Guidance from a physical therapist can be helpful, but patients need to adhere to the therapist's recommended home program and should not expect overnight success. Patients may not experience improvement of symptoms for six weeks or much longer, and the syndrome may recur.
Good physician-therapist communication is important but unfortunately is lacking in many medical settings. The physician can improve communication by asking for regular, written updates from the therapist, similar to the reports expected from a subspecialist referral.
RELATIVE REST
Initially, knee activity should be reduced, at least relatively, because the theory that patellofemoral pain is an overuse/overload syndrome has merit.5–8 A patient with the movie-goer's sign can benefit from straightening the leg or walking periodically as needed. If the patient is a runner or engages in impact activity and insists on continuing some rigorous activity, swimming or another nonimpact aerobic activity is a reasonable recommendation. For example, the so-called “elliptical” nonimpact exercise machines at health clubs have become quite popular for providing nonimpact aerobic activity.
ICE AND ANTI-INFLAMMATORY DRUGS
Ice is the safest anti-inflammatory “medication,” but its successful use requires discipline. Applying ice for 10 to 20 minutes after activity is reasonable. A common complaint is the inconvenience of holding an ice bag on the knee, but a simple elastic wrap solves this problem. A frozen gel pack, crushed ice in a plastic bag or a bag of frozen vegetables also work well.
Patients with patellofemoral pain syndrome have not been conclusively shown to benefit from anti-inflammatory drugs (NSAIDs). Although the same statement can be made about many treatments for patellofemoral pain, the drawback of NSAIDs is that their potential side effects may be more significant than any adverse effects of ice application or rehabilitative exercises. However, considering the convenience of NSAID therapy, a judicious trial may be worthwhile.
KNEE SLEEVES AND BRACES
The use of knee sleeves and braces in patients with patellofemoral pain is controversial.1,5,27 Typically, knee braces have a C-shaped lateral buttress that keeps the patella from deviating too far laterally. However, the patellofemoral mechanism is not that simple, for the patella moves in several planes.2,3 Knee braces are probably best reserved for use in patients with lateral subluxation that can be seen with the naked eye and can be easily palpated. A simple elastic knee sleeve with a patellar cut-out may provide some benefit, although this remains unproved. The use of a knee brace or sleeve should not be considered a substitute for therapeutic exercises.
TAPING THE KNEE
Taping the patella into a certain position to reduce friction may be helpful, although the results of studies have varied.18,28–32 A technique embraced by some physical therapists is known as “McConnell taping.”31 Although this taping method is helpful in selected patients,28,31,32 the original study that claimed efficacy31 was severely limited by the lack of a control group. A prospective randomized study30 found that McConnell taping plus physical therapy was no better than physical therapy alone. Still, when performed correctly in selected patients, taping may offer short-term pain relief. Most physical therapists are trained in taping and can teach patients to tape themselves.
FOOTWEAR
Athletic and walking shoes have improved significantly in the past decade, perhaps to the point of confusion as so many choices are now available. Generally speaking, the quality and age of footwear are more important than the brand name. It is not uncommon to hear patients state that a new, quality shoe helped alleviate their knee pain. Most runners, for example, change their shoes every 300 to 500 miles. It would benefit the physician to become familiar with one or two reputable footwear stores that provide good customer service.
ARCH SUPPORTS AND CUSTOM ORTHOTICS
Arch supports or custom orthotics can be helpful in patients with a wide variety of lower extremity complaints, including patellofemoral pain.33,34 Although the reasons are not entirely clear, an arch support may improve lower extremity biomechanics by preventing overpronation in pes planus and by providing a broader base of support for the normal or pes cavus foot.
Over-the-counter arch supports are a reasonable and relatively inexpensive initial suggestion. Custom orthotics may be worth a try if an over-the-counter insert is not helpful, although the expense is greater and superior efficacy has not been clearly established.
SURGERY
Surgery for patellofemoral pain syndrome is considered a last resort. True chondromalacia (fraying of the retropatellar cartilage) may be amenable to an arthroscopic surgical procedure to smooth out the undersurface of the patella.35 Unfortunately, the chondromalacia may return.
If the problem is clearly caused by excessive lateral tracking, a “lateral release” is sometimes appropriate. This procedure involves cutting the lateral retinaculum to reduce the amount of lateral pull.
Before the decision is made to perform a lateral release, other options and treatments should be considered. For example, the physician should consider whether the lateral tracking could simply be due to a tight iliotibial band or weak quadriceps muscles. Taping the knee to enhance medial glide should be tried. Having the patient wear a quality running shoe or arch support is another measure to try before surgery is contemplated. Although the lateral release is effective in a select group of patients, it is often considered an overused procedure, even among some orthopedic surgeons.3
SPONTANEOUS RESOLUTION
Spontaneous resolution of patellofemoral pain may occur,5,25,36 although many patients have already tried a “wait and see” approach by the time they seek medical treatment. Patellofemoral pain may be related to normal musculoskeletal development in some children and adolescents.25,26 For this reason, a conservative approach is preferred in the skeletally immature patient.
IMAGING
Imaging should be considered to rule out unusual conditions such as osteochondritis dissecans, infection or neoplasm. In general, six weeks of no improvement in a compliant patient, particularly if the symptoms are unilateral, is a reasonable period to wait before ordering plain-film radiographs.
TREATMENT RECOMMENDATIONS
An initial conservative approach to patients with patellofemoral pain syndrome should include the following measures: (1) relative rest with consideration of a temporary change to nonimpact aerobic activity; (2) quadriceps strengthening; (3) evaluation of footwear; and (4) icing, especially after activity.
Definitive treatment should be individualized. The addition of hip strengthening and stretching or stretching of the iliotibial band, hamstrings and calves should be based on a physical examination. Consideration should also be given to use of over-the-counter or custom orthotics. Patient education is essential, and patients need to be given realistic treatment expectations.
Even though the etiology and treatment of patellofemoral pain syndrome remain uncertain, the good news is that most patients do well with conservative treatment, particularly if they maintain a disciplined approach.