
Am Fam Physician. 2019;99(2):88-94
Patient information: See related handout on patellofemoral pain syndrome, written by the authors of this article.
Author disclosure: No relevant financial affiliations.
Patellofemoral pain syndrome (PFPS) is one of the most common causes of anterior knee pain encountered in the outpatient setting in adolescents and adults younger than 60 years. The incidence in the United States is between 3% and 6%. The cardinal feature of PFPS is pain in or around the anterior knee that intensifies when the knee is flexed during weight-bearing activities. The pain of PFPS often worsens with prolonged sitting or descending stairs. The most sensitive physical examination finding is pain with squatting. Examining a patient's gait, posture, and footwear can help identify contributing causes. Plain radiographs of the knee are not necessary for the diagnosis of PFPS but can exclude other diagnoses, such as osteoarthritis, patellar fracture, and osteochondritis. If conservative treatment measures are unsuccessful, plain radiography is recommended. Treatment of PFPS includes rest, a short course of nonsteroidal anti-inflammatory drugs, and physical therapy directed at strengthening the hip flexor, trunk, and knee muscle groups. Patellar kinesiotaping may provide additional short-term pain relief; however, evidence is insufficient to support its routine use. Surgery is considered a last resort.
Patellofemoral pain syndrome (PFPS) is a common cause of knee pain in adolescents and adults younger than 60 years. A retrospective review of an orthopedic database including more than 30 million patients in the United States between 2007 and 2011 estimated the incidence of PFPS to be 1.75 million patients, or about 6%.1 Females accounted for 55% of cases. The highest percentage of cases occurred in the South (42%), and the lowest occurred in the Northeast (14%). In a prospective study of 1,319 healthy, physically active young adults without a previous PFPS diagnosis, 3% developed PFPS during 2.5 years of follow-up, and women were more likely to develop the condition than men.2
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Exercise therapies are most effective in improving short- and long-term pain in patients with patellofemoral pain syndrome. | A | 3 |
| Short courses of nonsteroidal anti-inflammatory drugs improve pain in patients with patellofemoral pain syndrome compared with placebo, but the effect may be limited to one week. | B | 28 |
| Patellar kinesiotaping improves patellar maltracking and may reduce short-term pain as an adjunct to exercise. | B | 30, 33, 34 |
Definition
A 2016 consensus statement defines PFPS as pain occurring around or behind the patella that is aggravated by at least one activity that loads the patella during weight-bearing on a flexed knee.4 Contributing activities include running, climbing stairs, jumping, and squatting. PFPS is also called runner's knee and anterior knee pain syndrome.4 Although the term PFPS was formerly used interchangeably with chondromalacia patellae, the latter specifically refers to the finding of softened patellofemoral cartilage on plain radiography, magnetic resonance imaging, or knee arthroscopy.6 Conversely, structural defects are absent in PFPS, and imaging is not required for the diagnosis.
Anatomy and Pathophysiology
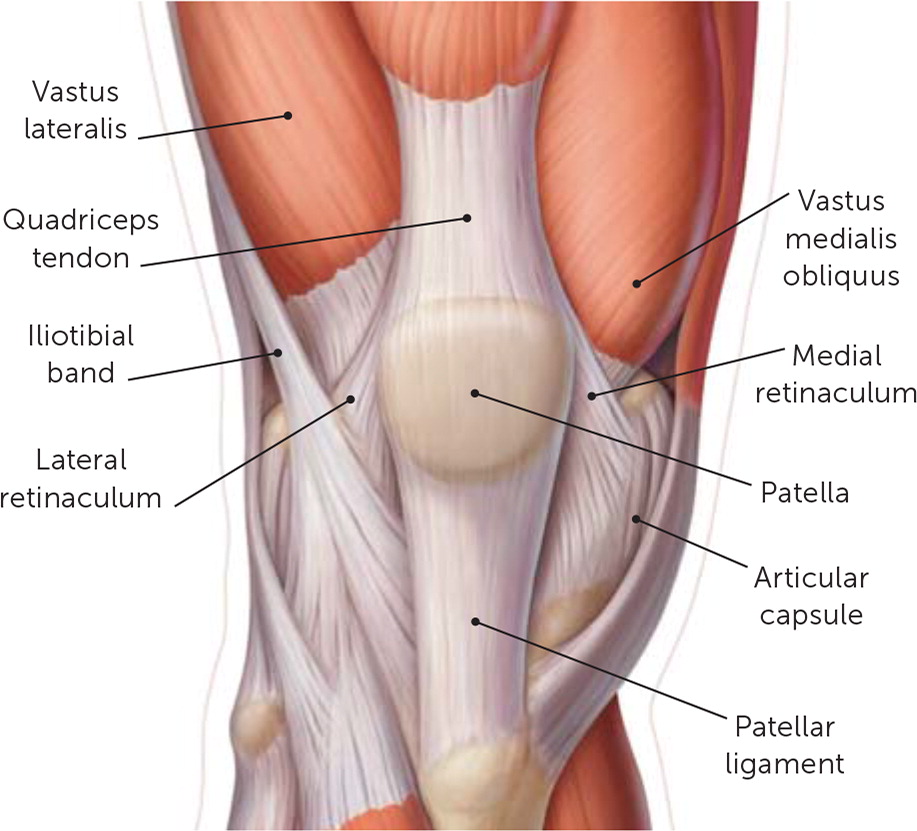
The patellofemoral joint consists of the patella and the trochlea of the femur and is important in knee extension and deceleration7 (Figure 18). The patella acts as a lever within the leg, decreasing the amount of force required by the quadriceps to extend the leg at the knee. The patellofemoral joint is stabilized by the quadriceps, patellar tendon, vastus medialis obliquus, medial patellofemoral ligament, medial patellotibial ligament, medial retinaculum, oblique lateral retinaculum, patellotibial band, epicondylopatellar bands, and lateral retinaculum.9
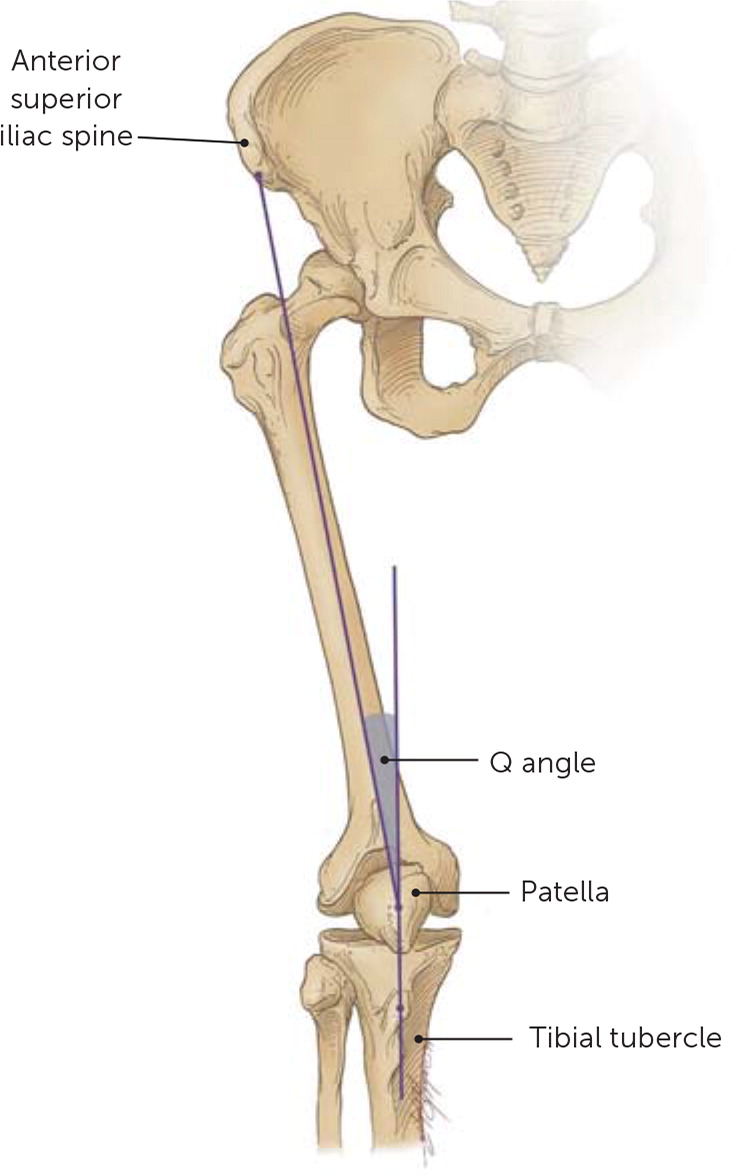
The force of the quadriceps is measured by the angle formed from the anterior superior iliac spine to the center of the patella to the tibial tubercle, which is known as the Q angle10 (Figure 211). The Q angle is approximately 14 degrees in men and 17 degrees in women.12 Because lateral forces on the patella are increased with higher Q angles, it has long been thought that a high Q angle increases the risk of PFPS; however, a higher Q angle has not been shown to be a clear contributing cause of PFPS in more recent research.12–14
Patellar maltracking is believed to play a role in PFPS. Patellar maltracking, or lateral translation, increases with load-bearing positions, such as squatting, in patients with PFPS. Stimulation of nerve endings within the retinacula, Hoffa (infrapatellar) fat pad, and peripatellar synovium may also contribute to the development of PFPS.15
Risk Factors
Established risk factors for PFPS (Table 1) include female sex and activities such as running, squatting, and going up and down stairs.1,2,16 In addition, a systematic review showed that decreased quadriceps strength was associated with a significantly higher risk of PFPS, likely because it can lead to patellar instability.16 Other etiologies of patellar instability, such as knee sprains, may also contribute to PFPS.17
| Activities such as running, squatting, and climbing up and down stairs |
| Dynamic valgus (increases patellar maltracking) |
| Female sex |
| Foot abnormalities (rearfoot eversion and pes pronatus) |
| Overuse or sudden increase in physical activity level |
| Patellar instability |
| Quadriceps weakness |
Dynamic valgus is another mechanism associated with PFPS. Dynamic valgus is a body position in which the knee collapses medially from excessive valgus, internal-external rotation, or both.18 This increases the lateral force on the patella, contributing to maltracking. Dynamic valgus is more common in female athletes, which may account for the higher incidence of PFPS in females.19 Foot abnormalities, such as rearfoot eversion and pes pronatus, lead to internal rotation of the tibia, which can also contribute to dynamic valgus.20
Diagnosis
| Cause | Comment |
|---|---|
| Articular cartilage injury | Possible history of trauma; mechanical symptoms may occur if loose body is present |
| Bone tumors | Pain may be insidious; may have tenderness of bony structures |
| Chondromalacia patellae | Retropatellar pain, may have history of trauma, may have effusion on examination |
| Hoffa disease | Pain and tenderness localized to the Hoffa (infrapatellar) fat pad |
| Iliotibial band syndrome | Typically presents as lateral pain and tenderness over the lateral femoral epicondyle |
| Lateral patellar compression syndrome | Poor patellar alignment sometimes caused by a tight lateral retinaculum results in anterior knee pain |
| Loose bodies | Symptoms vary; may have intermittent sharp pain, locking, or effusion |
| Osgood-Schlatter disease | Tenderness and swelling at patellar tendon insertion at the tibial tubercle in an adolescent |
| Osteochondritis dissecans | Symptoms vary; may have intermittent pain, swelling, or locking |
| Patellar instability/subluxation | Intermittent pain with the sensation of instability or movement of the patella; may have swelling; locking can occur with loose body formation; may have tenderness over the medial retinaculum |
| Patellar stress fracture | May have tenderness directly over the patella |
| Patellar tendinopathy | Tenderness of the tendon; tendon may be thickened if chronic |
| Patellofemoral osteoarthritis | May have crepitus or effusion; characteristic radiographic findings |
| Patellofemoral pain syndrome | Pain in or around the anterior knee that intensifies when the knee is flexed during weight-bearing activities; usually no effusion; may have findings of patellar maltracking |
| Pes anserine bursitis | Pain usually described as medial rather than anterior; tenderness over the pes anserine bursa |
| Plica syndrome | May be medial or lateral to the patella; if symptomatic, tenderness can be demonstrated on examination |
| Prepatellar bursitis | Characteristic swelling anterior to the patella following trauma |
| Quadriceps tendinopathy | Tenderness over the tendon |
| Referred pain from the lumbar spine or hip joint pathology | Symptoms depend on the origin of pain; knee examination is usually normal |
| Saphenous neuritis | Pain is usually medial but poorly localized; may have history of surgery |
| Sinding-Larsen-Johansson syndrome | Tenderness at the patellar tendon insertion at the inferior pole of the patella in an adolescent |
| Symptomatic bipartite patella | May have tenderness directly over the patella with characteristic radiographic findings |
HISTORY
Patients should be asked about previous knee injuries and surgeries, current activity level, and recent changes in activity. PFPS is a common form of knee overuse injury. Less commonly, patients may experience knee buckling, which is due to weakness or pain in the quadriceps resulting in a brief loss of muscle tone, not instability of the intrinsic knee joint.8 Locking and clicking in the knee are not consistent with PFPS, and instead suggest internal knee derangements such as meniscal tears.
PHYSICAL EXAMINATION
A physical examination of the knee should be performed in all patients presenting with a chief symptom of knee pain. Large joint effusion, erythema, and increased warmth are not features of PFPS and should prompt consideration of an alternative diagnosis such as infection, acute trauma, and inflammatory arthropathy.
In a meta-analysis, the presence of pain with squatting was the most sensitive physical examination finding for PFPS, and a positive result on the patellar tilt test carried the highest positive likelihood ratio.21 Table 3 includes commonly performed physical examination tests and their value in diagnosing PFPS.21–23
| Test | Sensitivity (%) | Specificity (%) | LR– | LR+ |
|---|---|---|---|---|
| Clarke test (https://www.youtube.com/watch?v=pRqnODPqxFs)* | 39 to 48 | 67 to 75 | 0.7 to 0.91 | 1.18 |
| Medial or lateral patellar facet tenderness† | 92 | 65 | 0.96 | Not determined |
| Pain during squatting | 91 | 50 | 0.2 | 1.8 |
| Patellar apprehension test (https://www.youtube.com/watch?v=4TnCQppTy1g) | 7 to 32 | 86 to 92 | 0.8 to 1.0 | 0.9 to 2.3 |
| Patellar tilt test (https://www.youtube.com/watch?v=DlHoesKkvTM) | 43 | 92 | 0.6 | 5.4 |
Examining the patient's gait and posture is also helpful in identifying contributing causes of PFPS, such as exaggerated lumbar lordosis, asymmetric hip height, or atrophic quadriceps, which in turn helps guide physical therapy.7 The patient's footwear should also be inspected. Excess wear patterns on the medial aspect of the shoe could suggest pes pronatus (https://www.youtube.com/watch?v=Wxx7O8HoOzI) or rearfoot eversion (https://www.youtube.com/watch?v=fiHX1ZWUl6c).8 Tight hamstrings have been associated with patellofemoral pain, possibly because of cocontraction of the hamstrings and quadriceps causing increased forces on the joint during exercise.24,25 Tight hamstrings can be assessed using the passive knee extension test (https://www.physio-pedia.com/Passive_knee_extension_test).
IMAGING
Although PFPS is a clinical diagnosis, imaging may be helpful to rule out other causes of knee pain. Imaging may be beneficial if the patient's pain has not improved after four to eight weeks of conservative measures. Plain radiography of the knee can rule out osteoarthritis in patients older than 50 years, patellar fractures in patients with a history of trauma, and osteochondritis if these diagnoses are suggested by the history or physical examination.7 The anteroposterior, lateral, and sunrise or Merchant views can be particularly helpful. Structural abnormalities such as minor patellar cartilage defects, bone marrow lesions, and increased signal in the Hoffa fat pad that are visible on magnetic resonance imaging are not associated with PFPS.26 Therefore, magnetic resonance imaging is not recommended in the evaluation for PFPS.26
Treatment
Treatment of PFPS should focus on early pain relief.27 Relative rest, ice, and analgesics are recommended to reduce pain, but physical therapy is the cornerstone of treatment.
MEDICATIONS
Analgesics, such as nonsteroidal anti-inflammatory drugs (NSAIDs), glucocorticoids, and glycosaminoglycan polysulphates, have been studied in randomized trials. A 2004 Cochrane review of pharmacotherapy for PFPS found low-quality evidence and conflicting results.28 If analgesics are used, a short course of NSAIDs is preferred. In one small double-blind randomized trial, one week of naproxen improved pain compared with placebo. High-quality studies showing pain reduction with longer courses of NSAIDs are lacking.28
PHYSICAL THERAPY
Because of the multiple contributing factors of PFPS, therapy should be individualized.27 Exacerbating movements or activities should be avoided, although the patient should otherwise remain as active as possible.5 A Cochrane review concluded that patients who exercise generally have improvement in short-term and long-term pain, both at rest and with activity, when compared with those who do not exercise.3 Exercise regimens should focus on the hip, trunk, and knee. There are no high-quality data to recommend one type of exercise over another.3 Core muscle strengthening reduces pressure on the patellofemoral joint by stabilizing muscle recruitment.29 Strengthening exercises and flexibility training of the associated muscle groups should be performed three times per week for six to eight weeks.30 Several commonly recommended exercises were illustrated previously in American Family Physician (https://www.aafp.org/afp/2015/1115/p875.html#sec-2).30 Exercise should be continued for long-term pain relief and improved functionality.31
OTHER THERAPIES
Beyond rest and exercise, other early therapies for PFPS include taping and foot orthotics.32 Kinesiotaping (Figure 3) can temporarily help improve patellar maltracking in athletes, although it is likely more beneficial earlier in the course of PFPS.30 In a single randomized trial of 90 patients, kinesiotaping improved short-term pain when added to exercises and physical therapy.33 However, a Cochrane review of five older trials found that the overall evidence is insufficient to recommend routine use of kinesiotaping.34 Foot orthotics can help correct dynamic valgus secondary to pes pronatus and rearfoot eversion, although it is unclear if they reduce pain.33–35 Combining exercise with foot orthotics is likely more beneficial than either treatment alone. Knee braces have not demonstrated benefit over exercise.36

Patellofemoral mobilizations and electrophysical therapies such as therapeutic ultrasound and transcutaneous electrical nerve stimulation are not recommended.31 Surgery has not been studied sufficiently to demonstrate improved clinical outcomes over conservative strategies, and should be performed only after conservative measures have failed and subsequent imaging elucidates a surgical indication.37
This article updates previous articles on this topic by Dixit, et al.,8 and Juhn.11
Data Sources: The search strategy centered primarily on identifying systematic reviews, meta-analyses, and randomized controlled trials that focused on treatment of patellofemoral pain syndrome. The key words used were patellofemoral pain syndrome, specifically conservative treatment, risk factors, demographics, Q angle, taping, exercise, and patellofemoral joint anatomy. Key sources included PubMed, Cochrane, UpToDate, Essential Evidence Plus, and the references from the 2009 AFP article on patellofemoral pain syndrome. Search dates: September 13 to December 18, 2017.
The opinions and assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the U.S. Army Medical Department or the U.S. Army Service at large.
