
A more recent article on smell and taste disorders is available.
Am Fam Physician. 2000;61(2):427-436
See related patient information handout on problems with smell or taste, written by the author of this article.
Smell and taste disorders are common in the general population, with loss of smell occurring more frequently. Although these disorders can have a substantial impact on quality of life and may represent significant underlying disease, they are often overlooked by the medical community. Patients may have difficulty recognizing smell versus taste dysfunction and frequently confuse the concepts of “flavor” and “taste.” While the most common causes of smell disturbance are nasal and sinus disease, upper respiratory infection and head trauma, frequent causes of taste disturbance include oral infections, oral appliances (e.g., dentures), dental procedures and Bell's palsy. Medications can interfere with smell and taste, and should be reviewed in all patients with reported dysfunction. In addition, advancing age has been associated with a natural impairment of smell and taste ability. A focused history and a physical examination of the nose and mouth are usually sufficient to screen for underlying pathology. Computed tomographic scanning or magnetic resonance imaging of affected areas, as well as commercially available standardized tests, may be useful in selected patients. The causes of olfactory dysfunction that are most amenable to treatment include obstructing polyps or other masses (treated by excision) and inflammation (treated with steroids). Enhancement of food flavor and appearance can improve quality of life in patients with irreversible dysfunction.
The senses of smell and taste allow full appreciation of the flavor and palatability of foods and also serve as an early warning system against toxins, polluted air, smoke and spoiled food products.1 Physiologically, the chemical senses aid in normal digestion by triggering gastrointestinal secretions.2
Smell or taste dysfunction can have a significant impact on quality of life. Deficits of these senses can adversely affect food choice and intake, especially in the elderly, and have been implicated in weight loss, malnutrition, impaired immunity and worsening of medical illness.3,4 Patients frequently report increased use of sugar and salt to compensate for diminished senses of smell and taste,5,6 a practice that is detrimental to those with diabetes mellitus or hypertension.
Subjective complaints do not always accurately reflect the chemosensory disturbance experienced by a patient. Although most affected patients complain of problems with smell and taste, testing frequently demonstrates impairment that is primarily olfactory in nature7–9 (Figure 1).7 Patients commonly confuse symptoms of flavor loss, which results from smell disturbance, with taste dysfunction. For example, the common cold may distort the flavor of food, but a patient's ability to taste (i.e., salty, sweet, sour, bitter) remains intact. Most flavors depend on retronasal stimulation of the smell receptors.
Smell
ANATOMY AND PHYSIOLOGY
The human sense of smell depends on the functioning of not only cranial nerve I (olfactory nerve) but also portions of cranial nerve V (trigeminal nerve). Qualitative odor sensations (e.g., the smell of a rose, lemon or grass) are mediated by cranial nerve I (Figures 2a and 2b), whereas somatosensory overtones of odorants (e.g., warmth, coolness, sharpness and irritation) are mediated by the ophthalmic and maxillary divisions of cranial nerve V.
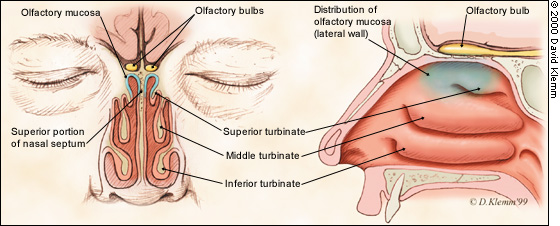
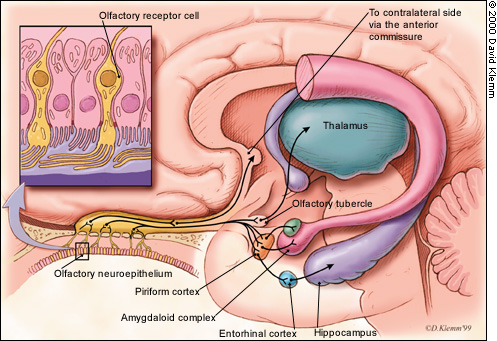
Smell receptors are located within the olfactory neuroepithelium, a region of tissue found over the cribiform plate, the superior septum and a segment of the superior turbinate. The free nerve endings of cranial nerve V are located diffusely throughout the nasal respiratory epithelium, including regions of the olfactory neuroepithelium. It is important to remember the distinctive nature of these two neural systems, because some odorants (e.g., ammonia) are sensed largely by the trigeminal nerve.
Once odorants enter the nose, they must move to the nasal vault and dissolve within the covering mucous layer in order to stimulate the olfactory receptors.1,10 Mucous has an important role in dispersing scents to the underlying receptors. The nasal turbinates are also important because they provide moderate resistance and a moist environment, thereby allowing optimal stimulation of olfactory neurons by airborne compounds.11,12
NATURAL HISTORY OF SMELL DEFICITS
CAUSES OF SMELL LOSS
| Common causes |
| Nasal and sinus disease (e.g., allergic or vasomotor rhinitis, chronic sinusitis, nasal polyps, adenoid hypertrophy) |
| Upper respiratory infection |
| Head trauma (e.g., frontal skull fracture, occipital injury, nasal fracture) |
| Cigarette smoking |
| Neurodegenerative disease (e.g., Alzheimer's disease, Parkinson's disease, multiple sclerosis) |
| Age |
| Less common causes |
| Medications (see Table 2) |
| Cocaine abuse (intranasal) |
| Toxic chemical exposure (e.g., benzene, benzol, butyl acetate, carbon disulfide, chlorine, ethyl acetate, formaldehyde, hydrogen selenide, paint solvents, sulfuric acid, thrichloroethylene) |
| Industrial agent exposure (e.g., ashes, cadmium, chalk, chromium, iron carboxyl, lead, nickel, silicone dioxide) |
| Nutritional factors (e.g., vitamin deficiency [A, B6, B12], trace metal deficiency [zinc, copper], malnutrition, chronic renal failure, liver disease [including cirrhosis], cancer, acquired immunodeficiency syndrome) |
| Radiation treatment of head and neck |
| Congenital conditions (e.g., congenital anosmia, Kallmann's syndrome) |
| Uncommon causes |
| Neoplasm or brain tumor (e.g., osteoma, olfactory groove or cribiform plate meningioma, frontal lobe tumor, temporal lobe tumor, pituitary tumor, aneurysm, esthesioneuroblastoma, melanoma, squamous cell carcinoma) |
| Psychiatric conditions (e.g., malingering, schizophrenia, depression, olfactory reference syndrome) |
| Endocrine disorders (e.g., adrenocortical insufficiency, Cushing's syndrome, diabetes mellitus, hypothyroidism, primary amenorrhea, pseudohypoparathyroidism, Kallmann's syndrome, Turner's syndrome, pregnancy) |
| Epilepsy (olfactory aura) |
| Migraine headache (olfactory aura) |
| Cerebrovascular accident |
| Sjögren's syndrome |
| Systemic lupus erythematosus |
It is important to have a high index of suspicion for subacute sinusitis, because decreased smell (hyposmia) can occur without other nasal or sinus symptoms typically associated with sinusitis (e.g., congestion, headache, a “throbbing” pressure sensation). Medications are also an important, frequently overlooked cause of smell impairment (Table 2).1,6,7,15 Olfactory impairment is estimated to occur in nearly 10 percent of patients with head trauma.17 Post-traumatic smell loss is usually caused by shearing injuries to the olfactory nerve fibers at the level of the cribiform plate, but it can also be caused by direct injury to the olfactory bulbs, olfactory tracts or frontal and temporal lobes.18,19
| Antibiotics |
| Ampicillin |
| Azithromycin (Zithromax) |
| Ciprofloxacin (Cipro) |
| Clarithromycin (Biaxin) |
| Griseofulvin (Grisactin) |
| Metronidazole (Flagyl) |
| Ofloxacin (Floxin) |
| Tetracycline |
| Anticonvulsants |
| Carbamazepine (Tegretol) |
| Phenytoin (Dilantin) |
| Antidepressants |
| Amitriptyline (Elavil) |
| Clomipramine (Anafranil) |
| Desipramine (Norpramin) |
| Doxepin (Sinequan) |
| Imipramine (Tofranil) |
| Nortriptyline (Pamelor) |
| Antihistamines and decongestants |
| Chlorpheniramine |
| Loratadine (Claritin) |
| Pseudoephedrine |
| Antihypertensives and cardiac medications |
| Acetazolamide (Diamox) |
| Amiloride (Midamor) |
| Betaxolol (Betoptic) |
| Captopril (Capoten) |
| Diltiazem (Cardizem) |
| Enalapril (Vasotec) |
| Hydrochlorothiazide (Esidix) and combinations |
| Nifedipine (Procardia) |
| Nitroglycerin |
| Propranolol (Inderal) |
| Spironolactone (Aldactone) |
| Anti-inflammatory agents |
| Auranofin (Ridaura) |
| Colchicine |
| Dexamethasone (Decadron) |
| Gold (Myochrysine) |
| Hydrocortisone |
| Penicillamine (Cuprimine) |
| Antimanic drug |
| Lithium |
| Antineoplastics |
| Cisplatin (Platinol) |
| Doxorubicin (Adriamycin) |
| Methotrexate (Rheumatrex) |
| Vincristine (Oncovin) |
| Antiparkinsonian agents |
| Levodopa (Larodopa; with carbidopa: Sinemet) |
| Antipsychotics |
| Clozapine (Clozaril) |
| Trifluoperazine (Stelazine) |
| Antithyroid agents |
| Methimazole (Tapazole) |
| Propylthiouracil |
| Lipid-lowering agents |
| Fluvastatin (Lescol) |
| Lovastatin (Mevacor) |
| Pravastatin (Pravachol) |
| Muscle relaxants |
| Baclofen (Lioresal) |
| Dantrolene (Dantrium) |
Taste
ANATOMY AND PHYSIOLOGY
Many nerves are responsible for transmitting taste information to the brain (Figure 3). Because of these multiple pathways, total loss of taste (ageusia) is rare. As in the olfactory system, somatosensory sensations (e.g., stinging, burning, cooling and sharpness) can be induced by many foods (e.g., hot peppers) through trigeminal nerve fibers in the tongue and oral cavity.
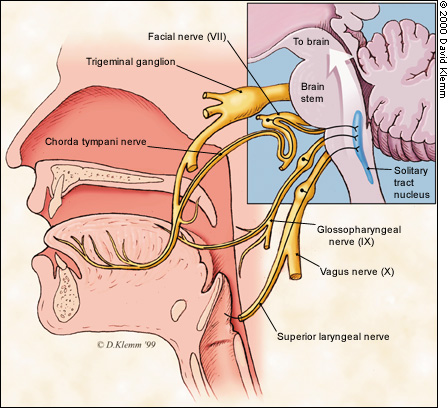
Taste receptors are found within taste buds located not only on the tongue but also on the soft palate, pharynx, larynx, epiglottis, uvula and first one third of the esophagus.20–22 Taste buds are continually bathed in secretions from the salivary glands, and excessive dryness can distort taste perception.
NATURAL HISTORY OF TASTE DEFICITS
CAUSES OF TASTE LOSS
| Common causes |
| Oral and perioral infections (e.g., candidiasis, gingivitis, herpes simplex, periodontitis, sialadenitis) |
| Bell's palsy |
| Medications (see Table 2) |
| Oral appliances (e.g., dentures, filling materials, tooth prosthetics) |
| Dental procedures (e.g., tooth extraction, root canal) |
| Age |
| Less common causes |
| Nutritional factors (e.g., vitamin deficiency [B3, B12], trace metal deficiency [zinc, copper], malnutrition, chronic renal failure, liver disease [including cirrhosis], cancer, acquired immunodeficiency syndrome) |
| Tumor or lesions associated with taste pathways (e.g., oral cavity cancer, neoplasm of skull base) |
| Head trauma |
| Toxic chemical exposure (e.g., benzene, benzol, butyl acetate, carbon disulfide, chlorine, ethyl acetate, formaldehyde, hydrogen selenide, paint solvents, sulfuric acid, thrichloroethylene) |
| Industrial agent exposure (e.g., chromium, lead, copper) |
| Radiation treatment of head and neck |
| Uncommon causes |
| Psychiatric conditions (e.g., depression, anorexia nervosa, bulimia) |
| Epilepsy (gustatory aura) |
| Migraine headache (gustatory aura) |
| Sjögren's syndrome |
| Multiple sclerosis |
| Endocrine disorders (e.g., adrenocortical insufficiency, Cushing's syndrome, diabetes mellitus, hypothyroidism, panhypopituitarism, pseudohypoparathyroidism, Kallmann's syndrome, Turner's syndrome) |
Alteration of taste can occur because of the release of bad-tasting materials as a result of an oral medical condition (e.g., gingivitis, sialadenitis). It can also occur because of problems with the transport of taste chemicals to the taste buds (e.g., as a result of excessive dryness of the oral cavity or damage to taste pores from a burn) because of the destruction or loss of taste buds. Another mechanism of taste loss is damage to one or more of the neural pathways innervating the taste buds (e.g., subsequent to viral Bell's palsy or dental or surgical procedures). Rarely, central neural factors (e.g., tumor or epilepsy) result in loss of taste.
Medications can be responsible for taste loss and should be reviewed in all patients with gustatory disturbance1,6,15,23 (Table 2). Angiotensin-converting enzyme inhibitors (notably captopril [Capoten]) are among the medications most commonly associated with taste disturbances, including decreased sense of taste (hypogeusia) and a strongly metallic, bitter or sweet taste.6 Excessive dryness of the oral cavity is a common side effect of a number of medications (e.g., anticholinergics, antidepressants, antihistamines) and disease states (e.g., Sjögren's syndrome, xerostomia, diabetes mellitus).
Clinical Evaluation of Smell and Taste
MEDICAL HISTORY
Because olfactory dysfunction is more common than taste dysfunction (Figure 1) and the three most common causes of loss of smell are nasal and sinus disease, upper respiratory infection and head trauma, it may be helpful to direct the history and physical examination toward these diagnoses. Intermittent olfactory loss may suggest an inflammatory process rather than a sensorineural lesion (Table 4).
| Findings | Diagnoses to consider |
|---|---|
| History | |
| Sudden loss of function | Head trauma (less likely with taste loss), cerebrovascular accident, acute upper respiratory infection, psychiatric condition |
| Intermittent loss of function | Inflammatory process (e.g., allergy, infection, chemical exposure) |
| Gradual loss of function | Nasal polyps, chronic upper respiratory infection |
| Difficulty passing air through nose | Obstruction secondary to polyps, inflammation or fracture |
| Physical examination | |
| Rhinorrhea | Rhinitis (e.g., allergy, infection, irritation) head trauma (fracture of cribiform plate) |
| Intranasal mass lesion | Polyps, neoplasm or tumor |
| Oral or perioral skin lesion | Viral infection (e.g., herpes simplex) |
| White plaque on tongue | Candidiasis, human immunodeficiency virus infection, acquired immunodeficiency syndrome, immunocompromised state, leukoplakia |
| Facial droop | Bell's palsy |
| Memory impairment | Alzheimer's disease |
| Motor findings (e.g., bradykinesia, cogwheel rigidity, akathisia, tremor, instability, ataxia, weakness) | Parkinson's disease, multiple sclerosis |
| Laboratory tests | |
| Low hematocrit, low hemoglobin level | Anemia, cancer, malnutrition |
| Altered red cell indexes | Nutritional deficiencies (e.g., vitamin B12) |
| Elevated white blood cell count | Infection |
| Elevated blood urea nitrogen level, elevated creatinine level | Renal disease |
| Elevated blood glucose level | Diabetes mellitus |
| Elevated liver enzyme level | Viral hepatitis, liver disease |
| Elevated bilirubin level, elevated alkaline phosphatase level | Liver disease |
| Elevated prothrombin time | Malnutrition, liver disease |
| Altered thyroid function tests | Thyroid disease |
| Elevated erythrocyte sedimentation rate | Sjögren's syndrome, systemic lupus erythematosus |
| Elevated eosinophil count | Allergy |
| Elevated immunoglobulin E level | Allergy |
The patient should be asked about the use of tobacco or cocaine, because these substances can adversely affect the sense of smell. Inquiry into the patient's diet and oral habits may reveal exposure to oral irritants. Specific questions should be asked about dryness of the mouth, periodontal disease, foul breath odor, recent dental procedures, recent radiation exposure, gastric reflux and medication use. Questions should also be directed at identifying any family history of systemic disease such as diabetes mellitus or hypothyroidism.
PHYSICAL EXAMINATION
A thorough examination of the head and neck should be performed to look for obstruction, inflammation and infection. Mucous membranes should be evaluated for dryness, leukoplakia and exudate. The patient's teeth and gums should also be examined, because severe dental caries, gingivitis and intraoral abscess can result in a malodorous and caustic oral environment that disturbs the senses of smell and taste.
Oral candidal infections in immunocompromised patients (e.g., those who have received chemotherapy or who have acquired immunodeficiency syndrome) can produce white patches or diffuse erythema. Viral infections (e.g., herpes simplex virus, coxsackievirus) tend to cause the development of vesicles with surrounding erythema, which then evolve into erosions or ulcers.
The neurologic examination should include a careful evaluation of cranial nerve function. Specific signs of damage to cranial nerve VII may include taste alterations in the anterior two thirds of the tongue, decreased salivation, auditory hyperacusis (resulting from paralysis of the stapedius muscle) and facial paralysis on the ipsilateral side.
LABORATORY TESTS
Clinical laboratory tests may be helpful in ruling out coexisting medical conditions suggested by the history and physical examination, such as infection, nutritional deficiency, allergy, diabetes mellitus and thyroid, liver or kidney disease (Table 4).
Although the history is routinely used to screen for cranial nerve I impairment, specific olfactory testing may be helpful in evaluating the patient with suspected loss of smell. The most widely available olfactory test is the Smell Identification Test.24 This test evaluates the ability to identify 40 microencapsulated “scratch and sniff” odorants. The odors are released by rubbing the microencapsulated strips with a pencil. The patient's test scores are then compared with norms for the same age and gender.14 It may be useful to test each side of the nose separately, because unilateral deficits in smell function may suggest a reversible cause (e.g., obstruction by a deviated septum, nasal polyps or another mass).10
Evaluation of taste is more difficult because no convenient standardized tests are presently available. A detailed history is generally the best screening tool. Research centers often use four ready-made solutions containing sucrose (sweet), sodium chloride (salty), quinine (bitter) and citric acid (sour) to obtain information about taste discrimination.
IMAGING TECHNIQUES
Plain radiographs have substantial limitations. These images do not provide sufficient detail for structures such as the osteomeatal complex. In particular, more detailed images are needed when endoscopic surgery is to be performed.
Computed tomographic (CT) scanning is the most useful and cost-effective technique for assessing sinonasal tract inflammatory disorders. Coronal CT scans are particularly valuable in assessing paranasal anatomy. Scanning with thin cuts (5 mm) is useful in identifying bony structures in the ethmoid, cribiform plate and olfactory cleft, as well as the temporal bone in proximity to cranial nerve VII or chorda tympani nerves; however, CT scanning is less effective than magnetic resonance imaging (MRI) in defining soft tissue disease.23,29 The use of intravenous contrast media helps to better identify vascular lesions, tumors, abscess cavities and meningeal or parameningeal processes.
MRI is superior to CT scanning in the evaluation of soft tissues, but it poorly defines bony structures. MRI is the technique of choice for assessing the olfactory bulbs, olfactory tracts, facial nerve and intracranial causes of chemosensory dysfunction. It is also the preferred technique for evaluating the skull base for invasion by sinonasal tumors. Gadolinium enhancement is useful for detecting dural or leptomeningeal involvement at the skull base.
Studies such as positron emission tomography and single photon emission computed tomography do not play a significant diagnostic role outside of major academic institutions.
Treatment
SMELL DYSFUNCTION
Olfactory disorders are more likely to be treated successfully when the patient has a reversible cause of intranasal interference such as nasal polyps, rhinitis, allergies or mechanical blockage.16 Because inflammatory nasal disease results in swelling of the olfactory clefts and the release of inflammatory mediators that likely alter the olfactory mucosa, the use of corticosteroids topically (e.g., aqueous nasal spray) or systemically (e.g., oral prednisone) may be helpful. However, some investigators have suggested that topical steroids do not reliably restore smell function.30 A useful dosing regimen for oral prednisone is 60 mg per day for four days, with the dosage tapered by 10 mg each day thereafter.30
Medical treatments generally are not effective in restoring olfactory function in patients with smell dysfunction after an upper respiratory infection.7,31 However, some investigators have suggested that absence of smell function (anosmia) subsequent to an upper respiratory infection may improve over time without specific treatment.32
Cigarette smoking by itself does not cause complete loss of the sense of smell. Patients who quit smoking typically have improved olfactory function and flavor sensation over time.33
Patients with permanent smell dysfunction need to develop adaptive strategies for dealing with personal hygiene, appetite, safety and health. Enhancement of food flavor may make eating more enjoyable. For example, marinating chicken in chicken-flavored bouillon may increase the palatability of the meat. Enhanced flavorings need not be spices and usually do not cause stomach irritation.
TASTE DYSFUNCTION
Many taste disorders (dysgeusias) resolve spontaneously within a few years of onset.34 However, several immediate steps can be taken to help correct a taste disturbance. For example, some drug-related dysgeusias can be reversed with cessation of the offending agent. Conditions such as radiation-induced xerostomia and Bell's palsy generally improve over time. An artificial saliva (e.g., Xerolube) may be helpful in patients with xerostomia.
Patients should be cautioned not to overindulge as compensation for the bland taste of food. For example, patients with diabetes may need help in avoiding excessive sugar intake as an inappropriate way of improving food taste. Patients with chemosensory impairment should use measuring devices when cooking, not “cook by taste.” Optimizing food texture, aroma, temperature and color may improve the overall food experience when taste is limited.
REFERRAL
Patients with persistent smell and taste complaints that are refractory to standard treatment and significantly impair their quality of life may need to be referred to an otolaryngologist, a neurologist or a subspecialist at a smell and taste center (Table 5). Referral centers specialize in detailed quantitative testing of smell and taste function. Specialized procedures such as functional imaging, endoscopy and biopsy with pathologic evaluation are available.
| Chemosensory Clinical Research Center |
| 925 Chestnut St. |
| Philadelphia, PA 19107 |
| Telephone: 215-955-5652 |
| Clinical Olfactory Research Center |
| State University of New York Health Science Center at Syracuse College of Medicine |
| 750 E. Adams St. |
| Syracuse, NY 13210 |
| Telephone: 315-464-5588 |
| Connecticut Chemosensory Clinical Research Center |
| University of Connecticut Health Center |
| 263 Farmington Ave. |
| Farmington, CT 06032 |
| Telephone: 860-679-2459 |
| MCV Smell and Taste Clinic |
| Medical College of Virginia, Virginia Commonwealth University |
| P.O. Box 980551 |
| Richmond, VA 23298-0551 |
| Telephone: 804-828-9350 |
| Nasal Dysfunction Clinic |
| University of California, San Diego, Medical Center |
| 9350 Campus Point Dr. |
| La Jolla, CA 92037 |
| Telephone: 858-657-8590 |
| Office of Health Communications |
| National Institutes of Health |
| NIH Building 31, Room 3C-35 |
| 31 Center Dr., MSC 2320 |
| Bethesda, MD 20892 |
| Telephone: 301-496-7243 |
| Rocky Mountain Taste and Smell Center |
| University of Colorado Health Science Center |
| Denver, CO 80262 |
| Telephone: 303-315-6600 |
| University of Cincinnati Taste and Smell Center |
| University of Cincinnati College of Medicine |
| 222 Piedmont Ave. |
| Cincinnati, OH 45219 |
| Telephone: 513-558-5469 |
| University of Pennsylvania Smell and Taste Center |
| Hospital of the University of Pennsylvania |
| 3400 Spruce St. |
| Philadelphia, PA 19104-4283 |
| Telephone: 215-662-6580 |