
A more recent article on seborrheic dermatitis is available.
Am Fam Physician. 2000;61(9):2703-2710
Patient information: See related handout on seborrheic dermatitis, written by the authors of this article.
Seborrheic dermatitis is a chronic inflammatory disorder affecting areas of the head and trunk where sebaceous glands are most prominent. Lipophilic yeasts of the Malassezia genus, as well as genetic, environmental and general health factors, contribute to this disorder. Scalp seborrhea varies from mild dandruff to dense, diffuse, adherent scale. Facial and trunk seborrhea is characterized by powdery or greasy scale in skin folds and along hair margins. Treatment options include application of selenium sulfide, pyrithione zinc or ketoconazole-containing shampoos, topical ketoconazole cream or terbinafine solution, topical sodium sulfacetamide and topical corticosteroids.
The etiology of seborrheic dermatitis remains unknown, although many factors, including hormonal, have been implicated. This chronic inflammatory skin disorder is generally confined to areas of the head and trunk where sebaceous glands are most prominent. When seborrheic dermatitis occurs in the neonatal period, it usually disappears by six to 12 months of age, suggesting that it may be a response to maternal hormone stimulation.1
Seborrheic dermatitis frequently affects persons in postpuberty. Additional evidence of hormonal influence is provided by research demonstrating that the human sebocyte responds to androgen stimulation.2
Pityrosporum ovale, a lipophilic yeast of the Malassezia genus, has been implicated in the development of this condition.3 It has been suggested that seborrheic dermatitis is an inflammatory response to this organism, but this remains to be proved.4 P. ovale is present on all persons. Why some persons develop seborrheic dermatitis and others do not is unclear. The colonization rate of involved skin by this organism may be lower than that of uninvolved skin.3 Nonetheless, the fact that seborrheic dermatitis responds to antifungal medications is strongly suggestive of the role of yeast in this disorder.
Genetic and environmental factors, as well as other comorbid diseases, may predispose specific populations to the development of seborrheic dermatitis. Although seborrheic dermatitis affects only 3 percent of the general population, the incidence in persons with acquired immunodeficiency syndrome may be as high as 85 percent. The exact mechanism whereby human immunodeficiency virus infection promotes an atypical and explosive onset of seborrheic dermatitis (and other common inflammatory skin disorders) is unknown, but many factors have been explored, including CD4-positive T lymphocyte counts,5 P. ovale density6 and nutritional factors.7
Persons with central nervous system disorders (Parkinson's disease, cranial nerve palsies, major truncal paralyses) also appear to be prone to the development of seborrheic dermatitis, tend to develop more extensive disease and are frequently refractory to treatment. It has been postulated that seborrheic dermatitis in these patients is a result of increased pooling of sebum caused by immobility. This increased sebum pool permits growth of P. ovale, which induces seborrheic dermatitis.8
Clinical Manifestations
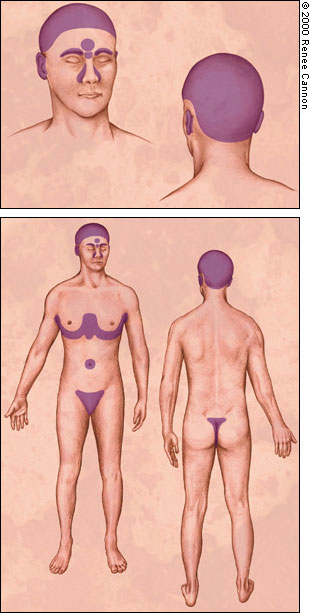
Seborrheic dermatitis typically affects areas of the skin where sebaceous glands appear in high frequency and are most active. The distribution is classically symmetric, and common sites of involvement are the hairy areas of the head, including the scalp (Figure 1), the scalp margin (Figure 2), eyebrows, eyelashes, mustache and beard. Other common sites are the forehead (Figure 3), the nasolabial folds (Figure 4), the external ear canals (Figure 5) and the postauricular creases. Seborrhea of the trunk may appear in the presternal area (Figure 6) and in the body folds, including the axillae, navel, groin, and in the inframammary and anogenital areas. Figure 7 illustrates the typically symmetric distribution of seborrheic dermatitis.






One of the characteristics of seborrheic dermatitis is dandruff, characterized by a fine, powdery white scale on the scalp. Many patients complain of the scalp itching with dandruff, and because they think that the scale arises from dry skin, they decrease the frequency of shampooing, which allows further scale accumulation. Inflammation then occurs and their symptoms worsen.
More severe seborrheic dermatitis is characterized by erythematous plaques frequently associated with powdery or greasy scale in the scalp (Figure 8), behind the ears (Figure 9) and elsewhere in the distribution described above. Besides an itchy scalp, patients may complain of a burning sensation in facial areas affected by seborrhea. Seborrhea frequently becomes apparent when men grow mustaches or beards and disappears when the facial hair is removed. If left untreated, the scale may become thick, yellow and greasy and, occasionally, secondary bacterial infection may occur.


Seborrheic dermatitis is more common in men than in women, probably because sebaceous gland activity is under androgen control. Seborrhea usually first appears in persons in their teens and twenties and generally follows a waxing/waning course throughout adulthood.
UV-A and UV-B light inhibit the growth of P. ovale,9 and many patients report improvement in seborrhea during summer.
Treatment
GENERAL TREATMENT OVERVIEW
Hygiene issues play a key role in controlling seborrheic dermatitis. Frequent cleansing with soap removes oils from affected areas and improves seborrhea. Patients should be counseled that good hygiene must be a lifelong commitment. Outdoor recreation, especially during summer, will also improve seborrhea, although caution should be taken to avoid sun damage.
Pharmacologic treatment options for seborrheic dermatitis include antifungal preparations (selenium sulfide, pyrithione zinc, azole agents, sodium sulfacetamide and topical terbinafine) that decrease colonization by lipophilic yeast and anti-inflammatory agents (topical steroids). Suggested products are listed in Table 1. For severe disease, keratolytics such as salicylic acid or coal tar preparations may be used to remove dense scale; then topical steroids may be applied. Other options for removing adherent scale involve applying any of a variety of oils (peanut, olive or mineral) to soften the scale overnight, followed by use of a detergent or coal tar shampoo.
As a last resort in refractory disease, sebosuppressive agents such as isotretinoin (Accutane) may be used to reduce sebaceous gland activity.
| Products | Over-the-counter? | Scalp | Beard | Face | Body | Instructions | Cost* | ||
|---|---|---|---|---|---|---|---|---|---|
| Shampoos | |||||||||
| Selenium sulfide, 1% (Selsun Blue) | Yes | X | X | X | X | 5- to 10-minute application daily initially; then twice weekly as needed | $3 per 120 mL bottle | ||
| Selenium sulfide, 2.5% (Exsel, Selsun) | No | X | X | X | X | Same as above | 15 per 120 mL (Exsel) | ||
| 12 per 120 mL (Selsun) | |||||||||
| Pyrithione zinc, 1% (Dandrex, Zincon, Head and Shoulders) | Yes | X | X | X | X | Same as above | 5 per 240 mL (Dandrex) | ||
| 3 per 120 mL (Zincon) | |||||||||
| 3 per 450 mL (Head and Shoulders) | |||||||||
| Pyrithione zinc, 2% (DHS Zinc, Sebulon, ZNP Bar, Theraplex Z) | Yes | X | X | X | X | Same as above | 7 per 240 mL (DHS Zinc) | ||
| 11 per 240 mL (Sebulon) | |||||||||
| 6 per 135 g (ZNP Bar) | |||||||||
| 7 per 240 mL (Theraplex Z) | |||||||||
| Coal tar | May be irritating, especially on the face | ||||||||
| Crude coal tar: | 5- to 10-minute application daily initially, then as needed | ||||||||
| DHS Tar (0.5%) | Yes | X | X | X | X | 5 per 120 mL (DHS Tar 0.5%) | |||
| Zetar (1%) | Yes | X | X | X | X | 14 per 180 mL (Zetar 1%) | |||
| Ionil T Plus (2%) | Yes | X | X | X | X | 12 per 240 mL (Ionil T Plus 2%) | |||
| Coal tar combinations: | Same as above | 10 per 210 mL (Sebutone) | |||||||
| Sebutone (0.5% with salicylic acid, 2%, and sublimed sulfur, 2%) | Yes | X | X | X | X | ||||
| Coal tar distillate: | |||||||||
| Doak-Tar (3%) | Yes | X | X | X | X | Same as above | 7 per 60 mL (Doak-Tar) | ||
| Coal tar extract: | Same as above | ||||||||
| Neutrogena T/Gel (2%) | Yes | X | X | X | X | 4 per 132 mL (Neutrogena T/Gel) | |||
| Tegrin Dandruff (7%) | Yes | X | X | X | X | 5 per 210 mL (Tegrin Dandruff) | |||
| Pentrax (7.71 %) | Yes | X | X | X | X | 7 per 120 mL (Pentrax) | |||
| Coal tar topical solution: | |||||||||
| Denorex Medicated (9%) | Yes | X | X | X | X | Same as above | 4 per 120 mL (Denorex Medicated) | ||
| Denorex Extra Strength (12.5%) | Yes | X | X | X | X | 4 per 120 mL (Denorex Extra Strength) | |||
| Coal tar solution combinations: | Same as above | ||||||||
| Ionil T (5% with salicylic acid, 2%) | Yes | X | X | X | X | 8 per 120 mL (Ionil T) | |||
| X-Seb T Plus (10% with salicylic acid, 3%) | Yes | X | X | X | X | 12 per 120 mL (X-Seb T Plus) | |||
| Tarsum (10% with salicylic acid, 2%) | Yes | X | X | X | X | 7 per 120 mL (Tarsum) | |||
| Chloroxine | No | X | 3-minute application twice weekly | 20 per 120 mL | |||||
| Capitrol, 2% | |||||||||
| Ketoconazole | |||||||||
| Nizoral, 1% | Yes | X | X | X | X | 5- to 10-minute application to scalp before rinsing clear; use daily initially, then twice weekly | 7 per 120 mL (Nizoral 1%) | ||
| Nizoral, 2% | No | X | X | X | X | 21 per 120 mL (Nizoral 2%) | |||
| Steroid shampoo | No | X | X | 5- to 10-minute application to scalp before rinsing clear; use daily initially until inflammation clears, then as needed | 15 per 120 mL | ||||
| FS Shampoo (0.01% fluocinolone acetonide) | |||||||||
| Topical Preparations | |||||||||
| Corticosteroids | Yes | X | X | X | X | Apply once or twice daily until inflammation clears, then as needed For scalp preparations, apply to scalp nightly until inflammation clears, then 1 to 3 times weekly as needed | 3 per 15 g (Cortaid, 1%) 3 per 15 g (Cortizone 10) 12 per 15 g (Tridesilon) 25 per 30 g (Hytone) 18 per 120 mL (Derma-smoothe/GS Topical oil) | ||
| Cortaid, 1%; Cortizone 10 (hydrocortisone cream, 1%) | |||||||||
| Tridesilon (desonide, 0.5%) | No | X | X | X† | X | ||||
| Hytone (hydrocortisone cream, 2.5%) | No | X | X | X† | X† | ||||
| Derma-smoothe/FS Topical oil (fluocinolone acetonide, 0.01% in oil) | No | X† | |||||||
| Antifungals | Apply once or twice daily | 5 per 15 g (Micatin) | |||||||
| Miconazole cream, 2% (Monistat) | Yes | X | X | ||||||
| Clotrimazole cream, 1% (Lotrimin) | Yes | X | X | 6 per 12 g (Lotrimin) | |||||
| Terbinafine solution, 1% (Lamisil) | Yes | X | X | X | X | 33 per 15 g (Lamisil) | |||
| Ketoconazole cream, 2% (Nizoral) | No | X | X | 17 per 15 g (Nizoral) | |||||
| Other preparations | |||||||||
| Sodium sulfacetamide | Apply once or twice daily | ||||||||
| Sebizon (10% lotion) | No | X‡ | X‡ | X | X | 24 per 85 g (Sebizon) | |||
| Novacet (10% sodium sulfacetamide plus 5% sulfur) | No | X‡ | X‡ | X | X | 28 per 30 g (Novacet) | |||
| Sulfacet R Lotion (10% sodium sulfacetamide plus 5% sulfur) | No | X‡ | X‡ | X | X | 34 per 25 g (Sulfacet R Lotion) | |||
| Benzoyl peroxide washes | Apply to affected area for 5 to 10 minutes; then rinse off; may bleach clothing or hair | ||||||||
| Benzac AC Wash (2.5%, 5%, 10%) | No | X | X | 21 to 26 per 240 mL (Benzac AC Wash) | |||||
| Benzac W Wash (5%, 10%) | No | X | X | 21 to 23 per 240 mL (Benzac W Wash) | |||||
| Desquam-X Wash (5%, 10%) | No | X | X | 15 to 16 per 150 mL (Desquam-X Wash) | |||||
TREATMENT OF SCALP AND BEARD AREAS
Many cases of seborrheic dermatitis are effectively treated by shampooing daily or every other day with antidandruff shampoos containing 2.5 percent selenium sulfide or 1 to 2 percent pyrithione zinc. Alternatively, ketoconazole shampoo may be used.10 The shampoo should be applied to the scalp and beard areas and left in place for five to 10 minutes before rinsing. A moisturizing shampoo may be used afterward to prevent dessication of the hair. After the disease is under control, the frequency of shampooing with medicated shampoos may be decreased to twice weekly or as needed. Topical terbinafine solution, 1 percent, has also been shown to be effective in the treatment of scalp seborrhea.11
If the scalp is covered with diffuse, dense scale, the scale may first be removed by applying warm mineral oil or olive oil to the scalp and washing several hours later with a detergent such as a dishwashing liquid or a tar shampoo.12 An alternative is an overnight application of a coal tarkeratolytic combination or phenol-saline solution with or without occlusion with a plastic shower cap followed by shampooing in the morning.13
Extensive scale with associated inflammation may be treated by moistening the scalp and then applying fluocinolone acetonide, 0.01 percent in oil, to the entire scalp, covering overnight with a shower cap and shampooing in the morning. This treatment may be done nightly until the inflammation clears and then decreased to one to three times weekly as needed. Topical corticosteroid solutions, lotions or ointments may be used once or twice daily for one to three weeks in place of the overnight application of fluocinolone acetonide and may be stopped when itching and erythema disappear. Corticosteroid application may be repeated daily for one to three weeks until itching and erythema disappear, and then used as needed. Maintenance with an antidandruff shampoo may then be adequate. Patients should be advised to use potent topical steroids sparingly because excessive use may lead to atrophy of the skin and telangiectasis.
Infants frequently have seborrheic dermatitis, commonly known as “cradle cap.” Areas of possible involvement include the scalp, face and intertriginous areas. Involvement may be extensive, but this disorder frequently clears spontaneously by six to 12 months of age and does not recur until the onset of puberty.
A scaly scalp in a prepubertal child is usually caused by tinea capitis, not seborrheic dermatitis. Therapy for infantile seborrheic dermatitis includes frequent shampooing with an antidandruff shampoo. If scale is extensive in the scalp, the scale may be softened with oil, gently brushed free with a baby hairbrush and then washed clear.
Daily shampooing may not be reasonable for some populations, such as black persons or persons who are institutionalized. In general, weekly shampooing is recommended for black persons. As a substitute for daily washing, fluocinolone acetonide, 0.01 percent in oil, may be used as a scalp pomade. Other options include application of a moderate- to mid-potency topical corticosteroid in an ointment base. As with other modes of therapy, these agents are used every day or twice daily until the condition improves. Thereafter, topical corticosteroids are used as needed to keep the condition under control. After initial control is attained, fluocinolone acetonide, 0.01 percent shampoo (FS Shampoo), can be used as an alternative to or in addition to fluocinolone acetonide, 0.01 percent in oil (Derma-Smoothe/FS), for maintenance.
TREATMENT OF THE FACE
Involved areas of the face may be washed frequently with shampoos that are effective against seborrhea as detailed above. Alternatively, ketoconazole cream, 2 percent, may be applied once or twice daily to affected areas. Often, 1 percent hydrocortisone cream will be added once or twice daily to affected areas and will aid with resolution of erythema and itching. Sodium sulfacetamide, 10 percent lotion, is also an effective topical agent for seborrheic dermatitis.
TREATMENT OF THE BODY
Seborrhea of the trunk may be treated with frequent application of zinc or coal tar containing shampoos or by washing with zinc soaps. Additionally, topical ketoconazole cream, 2 percent, and/or a topical corticosteroid cream, lotion or solution applied once or twice daily will prove useful. Benzoyl peroxide washes are also helpful in controlling seborrhea of the trunk. Patients should be cautioned to rinse thoroughly after application of these agents as they will bleach clothing and bed linens. These agents may be drying, and the patient may benefit from application of a moisturizer after treatment.
TREATMENT OF SEVERE SEBORRHEA
An occasional patient with severe seborrhea that is unresponsive to the usual topical therapy may be a candidate for isotretinoin therapy.14 Isotretinoin can induce up to a 90 percent reduction in sebaceous gland size, with a corresponding reduction in the production of sebum. Isotretinoin also has anti-inflammatory properties. Treatment with daily doses of isotretinoin as low as 0.1 to 0.3 mg per kg may result in improvement in severe seborrhea after four weeks of therapy. Thereafter, a dose as low as 5 to 10 mg per day may be effective as maintenance therapy over several years. However, isotretinoin has potentially serious side effects and few patients with seborrhea are appropriate candidates for therapy. The most devastating side effect is teratogenicity, but other serious side effects include hyperlipidemia, neutropenia, anemia and hepatitis. Mucocutaneous adverse effects include cheilitis, xerosis, conjunctivitis, urethritis and hair loss. Long-term use has been associated with the development of diffuse idiopathic skeletal hyperostosis (DISH). This agent must be used cautiously and only by physicians who are well versed in all of its adverse effects.
A more practical approach to the refractory patient may be to first try different combinations of the usual agents: a dandruff shampoo, an antifungal agent and a topical steroid. If this fails, short-term use of a more potent topical steroid in a “pulse fashion” may put some refractory patients into remission and actually decrease the total steroid exposure. Therapeutic choices for pulse therapy may include a nonfluorinated class III steroid such as mometasone furoate (Elocon) or an extra-potent class I or class II topical steroid such as clobetasol propionate (Temovate) or fluocinonide (Lidex). The class III topical steroid should be tried first, but if the condition remains unresponsive, the clinician may then choose to use a class I agent. These more potent agents may be applied once or twice per day, even on the face, but must be stopped after two weeks because of the increased frequency of side effects. If the patient responds before the two-week limit, the agent should be stopped immediately. Adjuvant therapy including use of a dandruff shampoo, an anti-fungal agent, or both, is essential during the “pulse” period and should be continued as maintenance therapy after each pulse.
Most corticosteroids are available as solutions, lotions, creams and ointments. Which vehicle to use is often determined by the patient and the treatment site. Lotions and creams are frequently used on all areas of the face and body, whereas solutions and ointments are more commonly used on the scalp. In general, application of a scalp solution is preferred by white and Asian patients but may be too drying for black patients. Ointments may be a better option. The vehicle affects the potency of a topical steroid. In most circumstances, the same steroid in an ointment is more potent than the steroid in a cream, which, in turn, is more potent than the same chemical in a lotion.
When to Refer
Patients should be referred to a dermatologist if the diagnosis is in doubt or if they are not responding to treatment. Seborrhea may be difficult to distinguish from atopic dermatitis, psoriasis, rosacea or superficial fungal infections. Chronic treatment with topical corticosteroids may lead to permanent skin changes, such as atrophy and telangiectasia. The explosive onset of seborrheic dermatitis in a young patient should give rise to consideration of underlying human immunodeficiency virus infection. One should consider referral to a dermatologist for patients with severe seborrhea in whom treatment with oral isotretinoin is contemplated, particularly if long-term therapy will likely be required.