
Am Fam Physician. 2000;61(10):3049-3056
A more recent article on managing hypertension using combination therapy is available.
The recommendation for first-line therapy for hypertension remains a beta blocker or diuretic given in a low dosage. A target blood pressure of less than 140/90 mm Hg is achieved in about 50 percent of patients treated with monotherapy; two or more agents from different pharmacologic classes are often needed to achieve adequate blood pressure control. Single-dose combination antihypertension therapy is an important option that combines efficacy of blood pressure reduction and a low side effect profile with convenient once-daily dosing to enhance compliance. Combination antihypertensives include combined agents from the following pharmacologic classes: diuretics and potassium-sparing diuretics, beta blockers and diuretics, angiotensin-converting enzyme (ACE) inhibitors and diuretics, angiotensin-II antagonists and diuretics, and calcium channel blockers and ACE inhibitors.
The sixth report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC VI)1 recommends that patients with hypertension and no comorbid illness begin antihypertensive drug therapy with a low dosage of a diuretic or beta blocker. This recommendation is supported by the results of a meta-analysis demonstrating that diuretics and beta blockers are the only agents shown to decrease the incidence of stroke and congestive heart failure in patients with hypertension.2 Diuretics administered in a low dosage have also been shown to decrease the incidence of coronary artery disease and total cardiovascular mortality.2
Although the documented decreases in morbidity and mortality make adequate treatment of hypertension important, the National Health and Nutrition Examination Survey (NHANES) report3 showed that blood pressure is controlled to a level below 140/90 mm Hg in only 27 percent of patients diagnosed with hypertension. Because monotherapy is effective in achieving this target goal in only about 50 percent of patients, treatment with two or more agents from different pharmacologic classes is often necessary to achieve adequate blood pressure control.4
The rationale for using fixed-dose combination therapy is to obtain increased blood pressure control by employing two antihypertensive agents with different modes of action and to enhance compliance by using a single tablet that is taken once or twice daily.5 Using low doses of two different agents can also minimize the clinical and metabolic effects that occur with maximal dosages of the individual components of the combined tablet.6 These potential advantages are such that some investigators have recommended using combination antihypertensive therapy as initial treatment, particularly in patients with target-organ damage or more severe initial levels of hypertension.7–9 Combination antihypertensive drugs are listed in Table 1.10
| Drug | Brand name | Cost (generic)* |
|---|---|---|
| Diuretic combinations | ||
| Amiloride and hydrochlorothiazide (5 mg/50 mg) | Moduretic | $18 (9 to 12) |
| Spironolactone and hydrochlorothiazide (25 mg/50 mg, 50 mg/50 mg) | Aldactazide | 15 (1 to 13) |
| Triamterene and hydrochlorothiazide (37.5 mg/25 mg, 50 mg/25 mg) | Dyazide | 14 (9 to 11) |
| Triamterene and hydrochlorothiazide (37.5 mg/25 mg, 75 mg/50 mg) | Maxzide-25 mg, Maxzide | 15 (4 to 10) |
| Beta blockers and diuretics | ||
| Atenolol and chlorthalidone (50 mg/25 mg, 100 mg/25 mg) | Tenoretic | 36 (4 to 27) |
| Bisoprolol and hydrochlorothiazide (2.5 mg/6.25 mg, 5 mg/6.25 mg, 10 mg/6.5 mg) | Ziac | 33 |
| Metoprolol and hydrochlorothiazide (50 mg/25 mg, 100 mg/25 mg, 100 mg/50 mg) | Lopressor HCT | 23 |
| Nadolol and bendroflumethazide (40 mg/5 mg, 80 mg/5 mg) | Corzide | 47 |
| Propranolol and hydrochlorothiazide (40 mg/25 mg, 80 mg/25 mg) | Inderide | 35 (6 to 10) |
| Propranolol ER and hydrochlorothiazide (80 mg/50 mg, 120 mg/50 mg, 160 mg/50 mg) | Inderide LA | 50 |
| Timolol and hydrochlorothiazide (10 mg/25 mg) | Timolide | 22 |
| ACE inhibitors and diuretics | ||
| Benazepril and hydrochlorothiazide (5 mg/6.25 mg, 10 mg/12.5 mg, 20 mg/12.5 mg, 20 mg/25 mg) | Lotensin HCT | 24 |
| Captopril and hydrochlorothiazide (25 mg/15 mg, 25 mg/25 mg, 50 mg/15 mg, 50 mg/25 mg) | Capozide | 28 (22) |
| Enalapril and hydrochlorothiazide (5 mg/12.5 mg, 10 mg/25 mg) | Vaseretic | 33 |
| Lisinopril and hydrochlorothiazide (10 mg/12.5 mg, 20 mg/12.5 mg, 20 mg/25 mg) | Prinzide | 30 |
| Lisinopril and hydrochlorothiazide (10 mg/12.5 mg, 20 mg/12.5 mg, 20 mg/25 mg) | Zestoretic | 31 |
| Moexipril and hydrochlorothiazide (7.5 mg/12.5 mg, 15 mg/25 mg) | Uniretic | 17 |
| Angiotensin-II receptor antagonists and diuretics | ||
| Losartan and hydrochlorothiazide (50 mg/12.5 mg, 100 mg/25 mg) | Hyzaar | 38 |
| Valsartan and hydrochlorothiazide (80 mg/12.5 mg, 160 mg/12.5 mg) | Diovan HCT | 36 |
| Calcium channel blockers and ACE inhibitors | ||
| Amlodipine and benazepril (2.5 mg/10 mg, 5 mg/10 mg, 5 mg/20 mg) | Lotrel | 48 |
| Diltiazem and enalapril (180 mg/5 mg) | Teczem | 51 |
| Felodipine and enalapril (5 mg/5 mg) | Lexxel | 37 |
| Verapamil and trandolapril (180 mg/2 mg, 240 mg/1 mg, 240 mg/2 mg, 240 mg/4 mg) | Tarka | 43 |
| Miscellaneous combinations | ||
| Clonidine and chlorthalidone (0.1 mg/15 mg, 0.2 mg/15 mg, 0.3 mg/15 mg) | Combipres | 26 (11) |
| Hydralazine and hydrochlorothiazide (25 mg/25 mg, 50 mg/50 mg, 100 mg/50 mg) | Apresazide | 15 (3 to 5) |
| Methyldopa and hydrochlorothiazide (250 mg/15 mg, 250 mg/25 mg, 500 mg/30 mg, 500 mg/50 mg) | Aldoril | 16 (6 to 14) |
| Prazosin and polythiazide (1 mg/0.5 mg, 2 mg/0.5 mg, 5 mg/0.5 mg) | Minizide | 21 |
Diuretics in Combination Antihypertensive Therapy
Diuretics are effective antihypertensive drugs. Treatment with a diuretic such as hydrochlorothiazide results in a dose-dependent blood pressure reduction that levels off with higher dosages (Table 2).11 In long-term trials, diuretics have been shown to reduce the incidence of stroke, congestive heart failure, coronary artery disease and total mortality from cardiovascular disease.
| Dosage (mg per day) | Blood pressure reduction (mm Hg) | |
|---|---|---|
| Systolic | Diastolic | |
| 50 | 23 | 17 |
| 25 | 21 | 14 |
| 12.5 | 14 | 11 |
| 6.25 | 7 | 6 |
Unfortunately, the degree of improvement in cardiovascular mortality is less than would have been expected based on epidemiologic data. One postulated but not yet proven explanation is that the higher diuretic dosages used in the large trials cause relative hypokalemia, as well as increased serum lipid levels, insulin resistance and uric acid levels. These adverse metabolic effects counteract the positive cardiovascular benefits of blood pressure reduction. Such effects do not occur when diuretics are administered in a low dosage, such as 6.25 or 12.5 mg per day of hydrochlorothiazide.11
Because diuretics blunt the sodium- and water-retaining effects of many other antihypertensive drugs, they are the most commonly used medication in combination antihypertensive agents. The JNC VI states clearly, “If a diuretic is not chosen as the first drug, it is usually indicated as a second-step agent because its addition will enhance the effects of other agents.”1(p2429)
POTASSIUM-SPARING AND THIAZIDE DIURETICS
The discrepancy between the JNC VI recommendations for first-line use of thiazide diuretics and the actual use of these agents in clinical practice may be attributable to physicians' concerns about the development of hypokalemia and hypomagnesemia, as well as the marketing of newer agents by pharmaceutical companies. Combination therapy with a potassium-sparing diuretic and a thiazide diuretic attempts to reduce the risk of adverse metabolic effects. Combination therapy does not obviate the need for serial monitoring of serum electrolyte levels, but it does decrease the incidence of thiazide-induced hypokalemia without an increased risk of hyperkalemia.12
Fixed-dose potassium-sparing–thiazide diuretic combinations have been in use for more than 20 years. Current combinations include spironolactone-hydrochlorothiazide (Aldactazide), triamterene-hydrochlorothiazide (Dyazide, Maxzide) and amiloride-hydrochlorothiazide (Moduretic). These combination drugs do not appear to differ significantly in efficacy or adverse effects.13 The described improvement in the bioavailability of Maxzide over Dyazide has not been shown to yield improved blood pressure control.14
All potassium-sparing–thiazide diuretic combinations seem to reduce blood pressure to the same degree as thiazide diuretics alone.15–18 In one large postmarketing surveillance study of patients treated with triamterene-hydrochlorothiazide,12 the incidence of hypokalemia was approximately one half to one third that expected in hydrochlorothiazide monotherapy. In addition, the amiloride-hydrochlorothiazide combination caused significantly less alteration of serum potassium levels than did hydrochlorothiazide given alone in dosages of 25 to 100 mg per day.15 The clinical applicability of the findings may be questionable because the studies used hydrochlorothiazide dosages that were significantly higher than those currently recommended.
The low dosages of hydrochlorothiazide (12.5 to 25 mg per day) advocated in the JNC VI provide significant blood pressure reduction while minimizing electrolyte abnormalities.19 It remains unclear whether the addition of a potassium-sparing agent confers additional benefit compared with a low dosage of hydrochlorothiazide alone.
BETA BLOCKERS AND DIURETICS
Beta blockers cause retention of sodium and water. Diuretics can cause mild volume reduction that leads to an increase in renin secretion by the kidney. The rationale for combining beta blockers with diuretics is twofold: beta blockers blunt the increase in the plasma renin level that is induced by diuretics, and diuretics decrease the sodium and water retention that is caused by beta blockers.6,20
The combination of a beta blocker and a diuretic produces additive effects compared with monotherapy using either agent alone. A recent study21 assessed the safety and efficacy of antihypertensive therapy using the cardioselective beta blocker bisoprolol alone and in combination with low dosages of hydrochlorothiazide. The dosages of bisoprolol were 2.5, 5 and 10 mg per day. The hydrochlorothiazide dosages were 6.25 and 25 mg per day. The study showed that monotherapy with either agent was more effective than placebo, but that when combination therapy was used, the beneficial effects were greater than when either agent was used alone (Figure 1).21
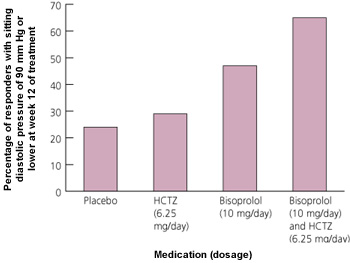
In the same study,21 combination therapy was associated with a low incidence of adverse effects. Side effects for combined hydrochlorothiazide in a dosage of 6.5 mg per day and bisoprolol in all dosages included fatigue (9 percent of recipients), dizziness (6 percent), somnolence (3 percent), impotence (2 percent) and diarrhea (4 percent). When used in combination with bisoprolol, hydrochlorothiazide (6.25 mg) did not cause hypokalemia or any adverse effects on the lipid profile. Side effects increased with the use of higher dosages of bisoprolol or hydrochlorothiazide. The incidence of hypokalemia and hyperuricemia was greater for 25 mg per day of hydrochlorothiazide than for 6.25 mg per day. With higher bisoprolol dosages, the frequency and severity of asthenia, diarrhea, dyspepsia and somnolence increased significantly.
ACE INHIBITORS AND DIURETICS
Angiotensin-converting enzyme (ACE) inhibitors are among the best tolerated antihypertensive drugs and have been used extensively as initial agents in the treatment of hypertension. The JNC VI1 recommends ACE inhibitors as second-line agents in most patients with hypertension and as first-line choices only in selected patients, including those with left ventricular systolic dysfunction and those with diabetes and microalbuminuria or proteinuria.
The reninangiotensin-aldosterone axis is important in the maintenance of systemic blood pressure. By causing volume and sodium depletion, thiazide diuretics stimulate the production of renin and angiotensin. This leads to a relative increase in blood pressure and sodium retention, which counteracts some of the other antihypertensive effects of the thiazide diuretics. ACE inhibitors interfere with the conversion of angiotensin I to angiotensin II and thereby decrease angiotensin II levels. These effects lead to decreased sodium retention and an enhanced antihypertensive effect.
Synergism between ACE inhibitors and diuretics is especially prominent in black patients, a population in whom monotherapy with ACE inhibitors has been shown to be less effective than it is in white patients. One small study22 of black patients with hypertension (N= 38) compared monotherapy using 20 mg per day of enalapril with combination therapy consisting of 20 mg of enalapril plus 12.5 mg of hydrochlorothiazide per day. Combination therapy significantly reduced systolic, diastolic and 24-hour ambulatory blood pressure measurements compared with monotherapy. Combination therapy controlled blood pressure to a level of less than 140/90 mm Hg in 74 percent of patients.
In this study,23 505 patients with diastolic blood pressures of 100 to 114 mm Hg received placebo, lisinopril (10 mg per day), hydrochlorothiazide (12.5 or 25 mg per day) or the combination of lisinopril (10 mg per day) and hydrochlorothiazide (12.5 or 25 mg per day). All drug therapies were more effective than placebo in lowering blood pressure, but the combination antihypertensive therapies produced the greatest effect (Figure 2).23
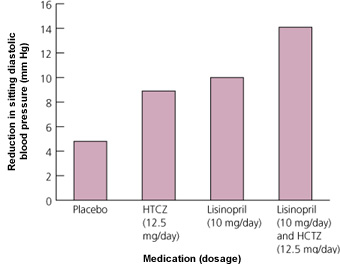
No significant differences in blood pressure reduction were observed for the two dosages of hydrochlorothiazide, whether the drug was used alone or in a combination.23 Adverse metabolic effects were observed only for regimens containing hydrochlorothiazide in a dosage of 25 mg per day. Serum potassium levels were significantly lower only for monotherapy with 25 mg per day of hydrochlorothiazide. Serum glucose measurements increased with the 25-mg dosage used as monotherapy or in combination with lisinopril.
The study23 found that the combination consisting of 10 mg per day of lisinopril and 12.5 mg per day of hydrochlorothiazide was well tolerated. The most commonly observed side effects were pharyngitis (14 percent of recipients), increased cough (6 percent), dizziness (2 percent), headache (12 percent) and asthenia (4 percent). Cough was the only side effect that was more prevalent in this group than in the placebo group.
Based on this large study,23 antihypertensive drug combinations containing an ACE inhibitor and a lower dose of hydrochlorothiazide are more desirable. It is important to be aware that the doses of ACE inhibitor in the antihypertensive drug combinations do not reach the target doses of ACE inhibitors recommended for the treatment of congestive heart failure, which may be a limitation in these patients.26
ANGIOTENSIN-II ANTAGONISTS AND DIURETICS
In patients for whom ACE inhibitor–diuretic combinations are indicated but not tolerated because of cough, angiotensin-II receptor antagonist–diuretic combinations are available. Angiotensin-II receptor antagonists work by blocking specific angiotensin II subtype I, thereby selectively inhibiting the vasoactive properties of angiotensin II.
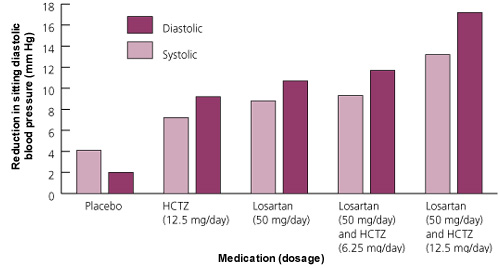
One study27 evaluated the efficacies of losartan in a dosage of 50 mg per day, hydrochlorothiazide in a dosage of 12.5 mg per day and combination therapy with 50 mg per day of losartan and 6.25 or 12.5 mg per day of hydrochlorothiazide. The treatments were compared with each other and with placebo (Figure 3).27 The greatest antihypertensive effect occurred with the combination of 50 mg of losartan and 12.5 mg of hydrochlorothiazide. This treatment reduced diastolic blood pressure to less than 90 mm Hg (or a reduction of 10 mm Hg or greater) in 78 percent of patients. The combination of losartan with the lower hydrochlorothiazide dose (6.25 mg) demonstrated no benefit over monotherapy with losartan. No significant differences in adverse events were attributable to the combination of losartan (50 mg) and hydrochlorothiazide (12.5 mg) compared with placebo.
Calcium Channel Blockers and ACE Inhibitors
The combination of a calcium channel blocker and an ACE inhibitor is appealing on theoretic grounds. Although calcium antagonists exert much of their antihypertensive effect through a vasodilatory action, they also have diuretic and natriuretic properties.28 ACE inhibitors blunt the stimulation of the reninangiotensin-aldosterone axis that may result from this diuretic effect. These agents also inhibit the central sympathetic stimulation that may result from calcium antagonist–associated vasodilatation, although both classes of drugs are potent vasodilators.29
ACE inhibitors and calcium channel blockers work effectively in combination to lower blood pressure.30–32 In one representative study,33 diastolic blood pressures were reduced by 3.6 mm Hg more with a trandolapril-verapamil combination than with monotherapy using either agent. No increase in side effects was observed for treatment with combined trandolapril and verapamil.
Calcium antagonists and ACE inhibitors may also work together to favorably influence target-organ disease independent of their effect on blood pressure. Together they appear to have a renal-protective effect,34 to promote reduction of left ventricular mass35 and to decrease mediators of vascular disease.36 The relatively low dose of ACE inhibitor in some combinations may not confer the same degree of renal or cardiac protection that has been demonstrated for higher doses.
Calcium channel blocker–ACE inhibitor combinations may result in fewer or milder side effects than occur with either agent alone. The addition of an ACE inhibitor to therapy with a dihydropyridine calcium antagonist significantly reduces the incidence of peripheral edema and reflex tachycardia. Neither class of medications has prominent metabolic side effects, an advantage in patients with diabetes and renal disease.
Four fixed-dose combinations of calcium channel blockers and ACE inhibitors are currently available in the United States. These combinations have yet to be proved more efficacious than antihypertensive combinations containing diuretics.
Miscellaneous Combination Agents
Other combination antihypertensive agents that have existed for many years include diuretics with a direct-acting vasodilator (hydralazine-hydrochlorothiazide [Apresazide]), a central alpha-adrenergic agonist (methyldopa-hydrochlorothiazide [Aldoril] and clonidine-chlorthalidone [Combipres]) or a peripheral alpha-adrenergic blocker (prazosin-polythiazide [Minizide]). No trials have indicated survival benefit with their use.
The JNC VI specifically mentioned that the three nondiuretic classes represented in these combinations “are not well suited for initial monotherapy because they produce annoying adverse effects in many patients.”1(p2426) No studies have provided conclusive evidence of increased tolerance when these agents are taken orally in combination with a diuretic. Therefore, these combinations are not indicated for first-line therapy.
Final Comment
The JNC VI1 continues to recommend monotherapy with a diuretic or beta blocker as initial treatment for the undifferentiated patient with hypertension. At the same time, it is recognized that monotherapy will not provide adequate blood pressure control in a large proportion of patients, and that many patients will experience unacceptable side effects with higher dosages of a single agent. Fixed-dose combination antihypertensive medications are a useful and appropriate treatment option in this large group of patients.