
Am Fam Physician. 2001;63(10):1969-1975
See patient information handout on babesiosis, written by the author of this article.
In the past decade, cases of babesiosis in humans have been reported with increasing frequency, especially in the northeastern United States. Babesia microti (in the United States) and bovine strains (in Europe) cause most infections in humans. Most cases are tick-borne, although cases of transfusion-associated and transplacental/perinatal transmission have also been reported. Factors associated with more severe disease include advanced age, previous splenectomy and immunodeficient states. Symptoms include high fever, chills, diaphoresis, weakness, anorexia and headache. Later in the course of the illness, the patient may develop jaundice. Congestive heart failure, renal failure and acute respiratory distress syndrome are the most common complications. Therapy using the combination of quinine sulfate and clindamycin was the most commonly used treatment; however, atovaquone suspension plus azithromycin was recently reported an equally effective and less toxic therapy. Exchange transfusion, together with antibabesial chemotherapy, may be necessary in critically ill patients.
Babesiosis is a worldwide tick-borne hemolytic disease that is caused by intraerythrocytic protozoan parasites of the genus Babesia. The book of Exodus refers to a plague of “murrain” (hemoglobinuria) among cattle and other domestic animals. Possibly, this biblical reference was the first historical mention of babesial infection.1–3 Intraerythrocytic piroplasms consistent with Babesia were first described by Babès in 1888 in his evaluation of the cause of febrile hemoglobinuria in cattle in Romania.1–3
In the past decade, cases of babesiosis in humans have been reported with increasing frequency, especially along the northeastern coast of the United States. The aim of this article is to summarize the current knowledge of this infection and provide guidance to clinicians.
Pathogenesis
Of the more than 100 species of Babesia, Babesia microti (in the United States) and Babesia divergens and Babesia bovis (in Europe) cause most infections in humans. B. microti also infects various small mammals and primates, while B. divergens has been found to infect rats and gerbils as well as its main bovine host. Recently, a previously unknown species of Babesia (WA-1) was isolated from an immunocompetent man in Washington state who had clinical babesiosis.4,5 Researchers also described another probable new babesial species (MO1) associated with the first reported case of babesiosis acquired in the state of Missouri. MO1 is probably distinct from B. divergens but the two share morphologic, antigenic and genetic characteristics.6
Ixodid (or hard-bodied) ticks, in particular Ixodes dammini (Ixodes scapularis) and Ixodes ricinus, are the vectors of the parasite. Ticks ingest Babesia while feeding off the host, and the parasite multiplies within the tick's gut wall. The parasites then spread to the tick's salivary glands. Inoculation into a vertebrate host occurs by a tick larva, nymph or adult.2,3 Infection in humans usually occurs from late spring to early fall.
After an infectious tick bite, the parasites invade red blood cells and a trophozoite differentiates, replicating asexually by budding with the formation of two to four merozoites. A second type of undifferentiated trophozoite is also formed that does not replicate but enlarges and differentiates into gametocyte-like forms similar to that seen in Plasmodium species. Merozoites eventually disrupt infected erythrocytes and reinvade other red blood cells.1–3
Epidemiology
Babesiosis has rarely been reported outside the United States. Sporadic cases have been reported from a number of countries including France, the former Yugoslavia, United Kingdom, Ireland, the former Soviet Union and Mexico. In the United States, infections have been reported from many states but the most endemic areas are the islands off the coast of Massachusetts (including Nantucket and Martha's Vineyard) and New York (including eastern and south central Long Island, Shelter Island and Fire Island) and in Connecticut.1–3,7,8 In these areas, asymptomatic human infection seems to be common.
Between 1968 and 1993, more than 450 Babesia infections were confirmed in the United States by blood smears or serologic testing, but the prevalence of babesiosis is difficult to estimate because of lack of surveillance, and because infections are often asymptomatic. A recent study9 evaluated the seroprevalence and seroconversion for tick-borne diseases in a high-risk population in the northeast United States. In this one-year seroconversion study of patients in New York state who were at high risk for tick-borne diseases, antibodies to B. microti were seen in seven of 671 participants (1 percent), including one asymptomatic seroconversion during the year of observation.9
Transfusion-associated babesiosis has also been described.10 The risk factors for the donors have included exposure to endemic areas and being a recipient of blood transfusions. Patients receiving erythrocyte transfusions are at highest risk, while infection after transfusion of plasma has not been reported. In a survey of 779 blood donors in Cape Cod, Mass., seropositivity ranged from 3.3 to 4.9 percent, which was comparable with that in Boston, a nonendemic area.11
Overall, the risk of acquiring babesiosis from a blood transfusion is very low. In Connecticut, the risk of acquiring babesiosis from a transfused unit of packed red blood cells was estimated at about 0.17 percent (95 percent CI, 0.004 to 0.9 percent) and was even lower from a transfused unit of platelets (95 percent CI, 0.0 to 0.8 percent).12 Finally, transplacental/perinatal transmission has been reported.2,3
Clinical Features
In the United States, the clinical spectrum of the infection ranges from asymptomatic to rapidly progressive and fatal. Although babesiosis can affect persons of all ages, most patients present in their 40s or 50s. After a recognized tick bite, the incubation period of babesiosis varies from five to 33 days.1,3,7
Symptoms include high fever (up to 40° C [104°F]), chills, diaphoresis, weakness, fatigue, anorexia and headache (Table 1). Later in the course of the illness, the patient may develop jaundice and dark urine. Physical examination may reveal hepatomegaly and splenomegaly or evidence of shock. Rash is an uncommon symptom in babesiosis.1,2,3,7 Signs of central nervous system involvement include headache, photophobia, neck and back stiffness, altered sensorium and emotional lability.3,7,15
| Generalized weakness |
| Fever |
| Gastrointestinal symptoms (anorexia, nausea, abdominal pain, vomiting, diarrhea, etc.) |
| Headache |
| Myalgia |
| Weight loss |
| Arthralgia |
| Respiratory symptoms (cough, shortness of breath, etc.) |
| Dark urine |
Congestive heart failure, disseminated intravascular coagulation and acute respiratory distress syndrome (that can occur even a few days after the onset of effective antimicrobial treatment) are the most common complications of human babesiosis (Table 2). Renal failure and myocardial infarction also have been associated with severe babesiosis. Researchers reviewed the clinical data and prognostic factors among 139 hospitalized cases in New York state between 1982 and 1993.16 Nine patients (6.5 percent) died, one fourth of the patients were admitted to the intensive care unit and one fourth of the patients required hospitalization for more than 14 days. The most common symptoms were fatigue/malaise/weakness (91 percent), fever (91 percent), shaking chills (77 percent) and diaphoresis (69 percent). Fifty-two percent of patients had a history of chronic disease. On average, a 12- to 14-day delay was noted between onset of symptoms and initiation of appropriate antibiotic treatment. Alkaline phosphatase levels greater than 125 U per L, white blood cell counts greater than 5 X 109 per L, history of cardiac abnormality, history of splenectomy, presence of heart murmur and parasitemia values of 4 percent or higher were associated with disease severity.16
| Acute respiratory distress syndrome |
| Anemia requiring transfusion |
| Congestive heart failure |
| Disseminated intravascular coagulation |
| Hypotension/shock |
| Myocardial infarction |
| Renal failure |
Diagnosis
Mild to severe hemolytic anemia and a normal to slightly depressed leukocyte count are common nonspecific findings in babesiosis. Usually, the diagnosis is based on typical morphologic picture on the blood smear in conjunction with epidemiologic information. A Wright- or Giemsa-stained peripheral blood smear is most commonly used to demonstrate the presence of intraerythrocytic parasites (Figure 1). Rarely, tetrads of merozoites are visible.
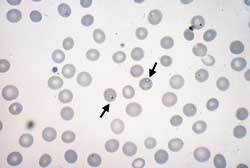
The organisms are intraerythrocytic ring forms closely resembling Plasmodium, the organism causing malaria. Three distinguishing features differentiate the two organisms. Babesial organisms usually form tetrads (“Maltese cross”), do not have hemozoin pigments within the affected red blood cells and have extracellular merozoites.17,18
Serologic evaluation with the indirect immunofluorescent antibody test with use of B. microti antigen is available in a few laboratories. The cutoff titer for determination of a positive result varies with the particular laboratory protocol used, but in most laboratories, titers of more than 1:64 are considered consistent with B. microti infection. Tenfold to 20-fold higher titers can be observed in the acute setting, with a gradual decline over weeks to months. The correlation between the level of the titer and the severity of symptoms is poor.1–3
Detection of B. microti by polymerase chain reaction (PCR) was first described in 1992.19 A more recent study,20 in which PCR was used prospectively for diagnosing suspected cases in the northeastern United States has shown that PCR is more sensitive and equally specific for the diagnosis of acute cases, in comparison with direct smear examination and hamster inoculation. PCR-based methods may also be indicated for monitoring of the infection.20
Treatment
Babesiosis may continue for more than two months after treatment and when left untreated, silent babesial infection may persist for months or even years. Researchers21 compared the duration of parasitemia in persons who had received specific antibabesial therapy with that in silently infected persons who had not been treated. Babesial DNA persisted for 16 days in 22 acutely ill subjects who received clindamycin and quinine therapy (P = 0.03). Among the subjects who did not receive specific therapy, symptoms of babesiosis persisted up to 114 days.21
Treatment with the combination of quinine (Quinamm; 650 mg of salt orally, three times daily) and clindamycin (Cleocin; 600 mg orally, three times daily, or 1.2 g parenterally, twice daily) for seven to 10 days is the most commonly used treatment. The pediatric dosage is 20 to 40 mg per kg per day for quinine and 25 mg per kg per day for clindamycin. The fortuitous discovery of this regimen for babesiosis in humans was made during the management of a patient with presumed transfusion-acquired malarial infection. The patient was initially treated with chloroquine (Aralen Injection); however, because of lack of response, treatment was changed to quinine and clindamycin.2,3,22,23
Several other drugs have been evaluated, including tetracycline, primaquine, sulfadiazine (Microsulfon) and pyrimethamine (Fansidar). Results have varied. Pentamidine (Pentam) has proved to be moderately effective in diminishing symptoms and decreasing parasitemia.
Atovaquone suspension (Mepron; 750 mg twice daily) plus azithromycin (Zithromax; 500 to 1,000 mg per day) is a very effective treatment. This treatment was found to be effective for the prevention and treatment of babesiosis in hamsters. Clindamycin plus quinine was also effective but less so than atovaquone. When treatment was not started until parasitemia became established, atovaquone in dosages of 300, 150 and 80 mg per kg per day was effective in the recovery of all animals compared with 50 percent of those receiving 10 mg per kg per day and 10 percent of untreated control subjects.24 Of note is that, in the same model, when atovaquone was used as monotherapy, the disease recurred. Organisms obtained from these animals, when inoculated into uninfected animals, proved to be unresponsive to atovaquone therapy, suggesting the emergence of drug resistance. Resistant organisms did not emerge in hamsters treated with the combination of atovaquone and azithromycin.25
In humans, a prospective, randomized study26 comparing the efficacy of clindamycin and quinine with that of atovaquone and azithromycin has been conducted. This study included 58 patients with non–life-threatening babesiosis. Forty received atovaquone and azithromycin and 18 received clindamycin and quinine. The resolution of symptoms and parasitemia were similar between the two groups and both treatments were effective for all patients. However, 72 percent of the patients who received quinine and clindamycin suffered side effects from the antibiotics, compared with 15 percent of patients in the atovaquone and azithromycin group.26
Exchange transfusion, together with antibabesial chemotherapy, may be necessary in critically ill patients. This treatment is usually reserved for patients who are extremely ill—with blood parasitemia of more than 10 percent, massive hemolysis and asplenia.17
Prevention
Prevention of babesiosis involves avoiding endemic regions during the peak transmission months of May through September. This recommendation may be especially relevant for asplenic or immunocompromised persons in whom babesiosis can be a devastating illness.1,2 Using insect repellant is advised during outdoor activities, especially in wooded or grassy areas. One of the most effective tick repellents is N, N-diethyl-m-toluamide (DEET). It is commercially available in concentrations up to 100 percent. However, serious toxic and allergic reactions have been reported in persons who have used it frequently or in high concentrations. In young children, toxic encephalopathy has occurred.2,3 Products with 10 to 35 percent DEET will provide adequate protection under most conditions.
Early removal of ticks is important; the tick must remain attached for at least 24 hours before the transmission of B. microti occurs. Therefore, daily self-examination is recommended for persons who engage in outdoor activities in endemic areas. Pets also must be examined for ticks because they may carry ticks into the home.
Co-infection with Other Species of Tick-Transmitted Diseases
Co-infection with Borrelia burgdorferi and B. microti may be relatively common in endemic areas of the northeastern and upper midwestern United States. Approximately 10 percent of patients with Lyme disease in southern New England are co-infected with babesiosis in sites where both diseases are zoonotic. The number of symptoms and duration of illness in patients with concurrent Lyme disease and babesiosis are greater than in patients with either infection alone.27,28
Co-infection with Ehrlichia species may also be seen. Three species of Ehrlichia have been described that infect humans, Ehrlichia chaffeensis, Ehrlichia phagocytophila and Ehrlichia ewingii. Typically, patients have a nonspecific febrile illness. Rash is uncommon with human granulocytic ehrlichiosis but common with human monocytic ehrlichiosis. Laboratory findings often include leukopenia, thrombocytopenia and increases in serum hepatic enzyme activities. In areas endemic for Lyme disease and ehrlichiosis, it maybe advisable to add doxycycline (Vibramycin), 100 mg twice a day by mouth, in the management of patients with babesiosis until serologic confirmation has been made.