
Am Fam Physician. 2001;64(7):1237-1238
A 27-year-old man with an insignificant medical history presented with symptoms of low-grade fever, sore throat, malaise and rhinorrhea lasting four days. Azithromycin and antihistamines were prescribed, and the patient was sent home. The symptoms worsened over the next four days, with onset of high-grade fever with chills, and difficulty swallowing and breathing. These symptoms were followed by onset of midsternal chest pain and swelling of the neck. The patient had no history of painful swallowing or vomiting.
Examination revealed a morbidly obese man in moderate respiratory distress sitting in an upright position. Vital signs included a temperature of 36.8°C (98.3°F), pulse rate of 124, blood pressure readings of 90/60 mm Hg (right) and 95/65 mm Hg (left) and a respiratory rate of 24. His neck was swollen, with no palpable subcutaneous emphysema. The patient's oral hygiene was very poor with extensive gingivitis. No erythema or exudates were noticed in the throat. The tonsils were moderately enlarged with no deviation of the uvula. No lymphadenopathy was present. The patient did not move his neck, but there was no nuchal rigidity. The chest was clear to auscultation with decreased air entry bilaterally. The rest of the examination was unremarkable.

Question
Discussion
The answer is B: acute descending necrotizing mediastinitis. Acute descending necrotizing mediastinitis, a variant of acute mediastinitis, is a rare but life-threatening infection originating in the oropharynx and characterized by rapid tissue destruction in the mediastinum. Oropharyngeal infections (such as odontogenic infection, Ludwig's angina and retropharyngeal abscess) can occasionally descend to the mediastinum. The descent of the infection from the oropharynx to the mediastinum is enhanced by gravity and negative intrathoracic pressure.
Widening of the mediastinum or a bulge over the aorta is common in aortic dissection (85 to 90 percent of cases),1 but the young age of this patient, the absence of hypertension and lack of difference in blood pressure in the two arms make this diagnosis less likely. The computed tomographic (CT) scan of the chest is a reasonably sensitive and specific test that did not show any evidence of aortic dissection in this patient.
The most common presentation of lymphoma is asymptomatic cervical or supraclavicular adenopathy. A widened mediastinum may be a presenting feature of lymphoma. The lack of cervical or supraclavicular adenopathy and the rapid deterioration in this patient did not support a diagnosis of lymphoma.
Esophageal rupture is most commonly caused by instrumentation, trauma or forceful vomiting. Patients present with severe retrosternal chest pain that may increase with swallowing or deep breathing. Patients frequently have subcutaneous and mediastinal emphysema.
Thymoma, a usually benign tumor of the thymus gland, may be associated with myasthenia gravis but no fever or expansion into the neck would be likely.
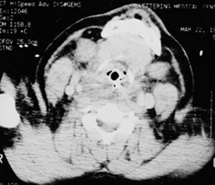
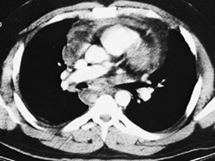
Chest radiographs in this patient showed widening of the mediastinum (Figure 1). Gastrografin barium swallow showed decreased peristalsis without obstruction or rupture of the esophagus. CT of the neck (Figure 2) showed marked retropharyngeal soft tissue swelling with compromise of the upper airway. CT scan of the chest and abdomen showed a widened mediastinum with soft tissue swelling and pericardial effusion (Figure 3). The patient's white cell count was 14,700 with 52 percent bands.
The patient was started on broad-spectrum antibiotics and underwent mediastinal drainage. Culture of the fluid drained showed heavy growth of Streptococcus intermedius and moderate growth of Streptococcus viridans. The patient recovered and was discharged home.
These infections are typically polymicrobial in nature, reflecting the usual aerobic and anaerobic oral flora.4 These patients are very ill, and the outcome may be catastrophic if not diagnosed early. The mortality rate (as high as 42 percent in the past) has been reduced to 25 percent with early diagnosis by CT scan, early surgical intervention and appropriate antibiotic coverage.5