
Am Fam Physician. 2003;68(10):1963-1969
A more recent article on pigmentation disorders is available.
This is part II of a two-part article on hyperpigmentation in adults. Part I, “Diagnostic Approach, Café au Lait Macules, Diffuse Hyperpigmentation, Sun Exposure, and Phototoxic Reactions,” appears in this issue on page 1955.
Nevi, or moles, are localized nevocytic tumors. The American Cancer Society's “ABCD” rules are useful for differentiating a benign nevus from malignant melanoma. While acanthosis nigricans may signal an underlying malignancy (e.g., gastrointestinal tumor), it more often is associated with insulin resistance (type 2 diabetes, polycystic ovary syndrome) or obesity. Melasma is a facial hyperpigmentation resulting from the stimulation of melanocytes by endogenous or exogenous estrogen. Treatments for melasma include bleaching agents, laser therapy, and a new medication that combines hydroquinone, tretinoin, and fluocinolone acetonide. Lesions that develop on the shins of patients with diabetic dermopathy often resolve spontaneously; no treatment is effective or recommended. Tinea versicolor responds to treatment with selenium sulfide shampoo and topical or oral antifungal agents. Postinflammatory hyperpigmentation or hypopigmentation can occur in persons of any age after trauma, skin irritation, or dermatoses.
Hyperpigmentation usually can be traced to the presence and activity of melanocytes. Part I of this two-part article presents a suggested approach to patients with increased pigmentation. Part II continues the review of conditions associated with hyperpigmentation.
New, Changing, or Symptomatic Localized Lesions
A localized hyperpigmented or irregularly pigmented lesion that is new in onset, arises within a congenital nevus, or causes pain or itching could be a malignant melanoma (Figures 1 through 3). The American Cancer Society has developed useful guidelines for identifying suspicious nevi (Table 1).1 [Evidence level C, consensus/expert guidelines]



| Asymmetry. One half of the mole does not match the other half. |
| Border irregularity. The edges of the mole are irregular, ragged, blurred, or notched. |
| Color. The color over the mole is not the same. There may be differing shades of tan, brown, or black, and sometimes patches of red, blue, or white. |
| Diameter. The mole is larger than 6 mm (about 1¼4 inch or about the size of a pencil eraser), although in recent years, physicians are finding more melanomas between 3 and 6 mm. |
| Other important signs of melanoma include changes in size, shape, or color of a mole or the appearance of a new spot. Some melanomas do not fit the ABCD rule described above, so it is particularly important to be aware of changes in skin lesions or new skin lesions. |
When possible, suspicious lesions should be excised totally for pathologic evaluation. If size or location precludes complete excision, incisional biopsy (usually punch biopsy) is performed.2
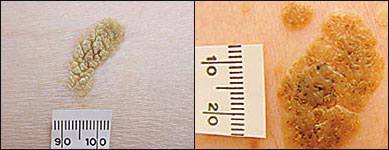
Seborrheic keratoses are localized, benign, hyperplastic, hyperpigmented lesions that may mimic melanomas. The hyperpigmentation is associated with hyperplasia of melanocytes.3 Experienced physicians usually can differentiate seborrheic keratoses based on their sharp borders; tan, brown, or black color; and typical appearance. These lesions have a “stuck-on” appearance, with a surface that is rough and craggy (Figure 4, left) or smooth with small keratin “pearls” (Figure 4, right).4
If seborrheic keratoses are symptomatic or there is a question about possible malignancy, the lesions should be removed and sent for pathologic evaluation.
Acanthosis Nigricans
Acanthosis nigricans, usually related to insulin resistance or obesity, ranges in appearance from a thickened, velvety brown streaking to a leathery, verrucous, papillomatous lesion (Table 2). The condition commonly occurs on the neck or in skin folds (e.g., in the axilla, under the breast, at the belt line, in the groin), but it may develop in other parts of the body. Patients with this condition may complain that they have a “dirty area” that cannot be cleansed (Figure 5).
| Disorder | Appearance | Age of onset | Hormone or medication related | Sun or otherexposure involved | Associated systemic complications | Treatment |
|---|---|---|---|---|---|---|
| Acanthosis nigricans | Velvety brown color, located in axillae, on neck, and in areas of skin folds | Adolescence to adulthood | Insulin resistance | Not involved | Increased risk of diabetes, polycystic ovary syndrome, dyslipidemia and, possibly, underlying malignancy | Treat underlying disease or condition. |
| With acute onset (especially on palms or soles) in nonobese adults, evaluate carefully for malignancy. | ||||||
| Melasma | Macular hyperpigmentation of cheeks, forehead, and upper lip | Adulthood | Pregnancy, use of oral contraceptive pills, phenytoin (Dilantin) therapy | Increased by sun exposure | None | Treat for cosmesis avoid sun exposure; use bleaching laser therapy, ordermabrasion. |
| Diabetic dermopathy | Papular pink or brown eruption evolving to macular, sometimes confluent brown eruption on anterior shins | Adulthood | Uncertain | Not involved | Multiorgan dysfunction related to underlying diabetes | Treat underlying diabetes. |
| Tinea versicolor | Dark or light scaly lesions, single or confluent patches on trunk | Adolescence through adulthood | Increased sebum production starting in adolescence | Hypopigmented appearance because tanning process is blocked | None | Treat with topical selenium sulfide shampoo, or topical or oral antifungal agents. |
| Postinflammatory hyperpigmentation | Localized, macular, brown hyperpigmentation at site of inflammation | Any age | Not related | Reaction to trauma (physical or chemical injury), skin irritation, or dermatoses | Inflammation of skin because of underlying injury or condition | Refer patient to cosmetic dermatologist. |
Microscopically, acanthosis nigricans is characterized by an increased number of melanocytes, with papillary hypertrophy and hyperkeratosis.5 Associated hypertrophy and hyperkeratosis cause acanthosis nigricans to be palpable rather than macular.
It is important for physicians to recognize acanthosis nigricans, because the condition can be associated with insulin resistance (as occurs in type 2 diabetes and polycystic ovary syndrome), obesity and, occasionally, malignancy. Type 2 diabetes is increasing in incidence in the United States, especially among black and hispanic children; 60 to 92 percent of these children have acanthosis nigricans.6 According to one study7 that compared 50 children with type 2 diabetes and 50 children with type 1 diabetes, acanthosis nigricans was present in 86 percent of the children with type 2 diabetes but in none of the children with type 1 diabetes.7 [Evidence level B, retrospective cohort study]
If a patient rapidly develops acanthosis nigricans, especially on the palms or soles, occult malignancy is a possibility. A thorough physical examination, a review of systems, a complete blood count, fecal occult blood testing, and chest radiography should be considered if the patient does not fit the typical clinical pattern of insulin resistance.8 [Evidence level C, consensus/expert guidelines] Adenocarcinomas are the most common malignancies found in patients with acanthosis nigricans; the tumors are most often present in the stomach (60 percent), followed by the colon, ovary, pancreas, rectum, and uterus.9
Treatment of acanthosis nigricans is directed at the underlying cause, rather than the appearance of the skin. If present, insulin resistance should be managed appropriately. Screening for hypercholesterolemia and coronary artery disease may be appropriate, depending on the clinical picture.
Melasma
Pregnancy or the use of hormones (e.g., oral contraceptive pills) can cause melasma, a localized facial hyperpigmentation (Figure 6). Melasma may be seen in patients who take phenytoin (Dilantin). While melasma may regress after pregnancy, it may increase with each subsequent pregnancy and become quite obvious. Because of the facial location, melasma may be quite disturbing to patients.

Frequently called the “mask of pregnancy,” melasma (chloasma) differs from the ruborous glow of pregnancy. Histologically, women who have this condition develop an increased number of melanocytes, with the deposition of additional melanin and a background of solar elastosis, typically on the cheeks, forehead, and upper lip.10 Examination using a Wood's light in a darkened room demonstrates enhanced contrast if hyperpigmentation affects the epidermal layer of skin.11
Patients with hyperpigmentation of the superficial epidermal layer who desire treatment may attempt a trial of bleaching agents after patch testing elsewhere on the body to confirm low levels of inflammation. Use of bleaching agents on inflamed skin could lead to postinflammatory changes and further hyperpigmentation.
Tretinoin 0.1 percent (Retin-A) cream and hydroquinone (Eldoquin Forte), a bleaching agent available in 2 to 4 percent creams and gels, have been the mainstays of topical treatment. Combining tretinoin and hydroquinone (applied at different times during the day) can potentiate the effect.
A new medication that contains tretinoin, hydroquinone, and fluocinolone acetonide (Tri-Luma) has been effective in the treatment of melasma. In a company-sponsored, double-blind, randomized controlled trial of the triple-combination agent, 77 percent of patients showed complete or nearly complete clearing of melasma, compared with 47 percent for hydroquinone and tretinoin, 42 percent for fluocinolone acetonide and hydroquinone, and 27 percent for tretinoin and fluocinolone acetonide.12 [Evidence level B, lower quality randomized controlled trial] The triple-combination agent should be applied daily, 30 minutes before bedtime. Azelaic acid (20 percent), kojic acid formulations, and alpha-hydroxy acids also have been useful in the treatment of melasma.13
Side effects of all topical treatments include allergic and contact dermatitis, depigmentation of surrounding normal skin, and post-inflammatory hyperpigmentation. Tretinoin alone or combined with hydroquinone and fluocinolone acetonide should not be used during pregnancy.
If no increase in contrast is seen with use of the Wood's light, the deeper dermal tissues usually are involved, and bleaching agents will not help.11 Laser therapy may be used for superficial epidermal or deeper dermal melasma, but strict avoidance of sun exposure is important to prevent recurrence.14 [Evidence level C, expert opinion]
Diabetic Dermopathy
Diabetic dermopathy (pigmented pretibial papules) develops in up to 70 percent of patients with diabetes.15 This condition usually affects the skin of the anterior tibial area, where it starts as a papular pink or brown eruption and progresses to a macular, sometimes confluent, brown dermatitis, with the coloration caused by hemosiderin deposition (Figure 7). The exact cause of the lesions is unknown.

The lesions of diabetic dermopathy may resolve spontaneously, even as new lesions arise. Treatment should focus on the patient's diabetes. No treatment for the asymptomatic cutaneous lesions is effective or recommended.16
Tinea Versicolor
While tinea versicolor is not truly a hyperpigmentation disorder, it is included in this review because affected skin on the trunk may appear darker than normal. Tinea versicolor rarely occurs until after adolescence, when production of sebum increases, especially in the skin of the anterior trunk and back. The increased sebum production allows the proliferation of Pityrosporum ovale or Pityrosporum orbiculare (Malassezia furfur),17 which can cause a brown, pink, or reddish discoloration of the skin.
Technically a papulosquamous eruption, tinea versicolor presents as numerous macules or slightly raised papules with subtle scale. Patients may have a coalescence of lesions or a single patch with an irregular border. The lesions of tinea versicolor may be several centimeters in diameter, or they may cover most of the trunk.
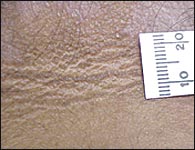
Over time, the Pityrosporum species can block the conversion of tyrosine to melanin,18 leading to hypopigmented patches instead of increased coloration. The scale on the surface of the affected skin (Figure 8) and the “spaghetti and meatball” appearance of fungal forms on a potassium hydroxide preparation help to clarify the diagnosis.

Tinea versicolor may be treated with topical selenium sulfide shampoo in a daily or weekly treatment regimen. Once a day for one week, the selenium sulfide shampoo is allowed to dry on the affected skin for 10 minutes before the patient showers. Alternatively, once a week for four weeks, the selenium sulfide shampoo is left on the skin for 12 to 24 hours, after which time the patient showers.
Topical antifungal agents (e.g., allylamines, azoles, undecenoic acid) also are effective therapies for tinea versicolor.19 [Evidence level A, Cochrane review] Because of the amount of topical medication required and the length of treatment (several weeks), orally administered agents have been studied and found to be effective.20 [Evidence level A, Cochrane review] A 2 percent ketoconazole shampoo, left in place for five minutes, has been shown to have a cure rate of 69 percent after one application.21
Postinflammatory Hyperpigmentation
Trauma (physical or chemical injury), skin irritation, and dermatoses can lead to postinflammatory hyperpigmentation or hypopigmentation in persons of any age. Investigators in one study22 theorized that some persons have an inherited tendency for weak melanocytes that respond to inflammation by decreasing melanin production, or for strong melanocytes that respond by increasing melanin production. While more effect is evident when lighter-skinned persons respond with hyperpigmentation (Figure 9) or darker-skinned persons respond with hypopigmentation, persons of all races can respond to inflammation with hyperpigmentation or hypopigmentation.

With time and resolution of the inflammation, the pigmentary changes usually tend to normalize. If cosmesis is desired, it should be performed by a physician with experience in cosmetic dermatology, because treatments such as bleaching agents can cause further postinflammatory pigmentary changes.