
A more recent article on management of head and neck injuries is available.
Am Fam Physician. 2006;74(8):1357-1364
Patient information: See related handouts on concussions athttps://familydoctor.org/familydoctor/en/diseases-conditions/concussion.html, and on burners athttps://familydoctor.org/familydoctor/en/diseases-conditions/burners.html.
Author disclosure: nothing to disclose.
Injuries to the head and neck are common in sports. Sideline physicians must be attentive and prepared with an organized approach to detect and manage these injuries. Because head and neck injuries often occur simultaneously, the sideline physician can combine the head and neck evaluations. When assessing a conscious athlete, the physician initially evaluates the neck for spinal cord injury and determines whether the athlete can be moved safely to the sideline for further evaluation. This decision is made using an on-field assessment of the athlete’s peripheral sensation and strength, as well as neck tenderness and range of motion. If these evaluations are normal, axial loading and Spurling testing can be performed. Once the neck has been determined to be normal, the athlete can be assisted to the sideline for assessment of concussion symptoms and severity. This assessment should include evaluations of the athlete’s reported symptoms, recently acquired memory, and postural stability. Injured athletes should be monitored with serial examinations, and those with severe, prolonged, or progressive findings require transport to an emergency department for further evaluation.
Although catastrophic injuries are rare in sports, they are the main reason for the presence of physicians at the sideline of school and community athletic events. Family physicians who volunteer for this duty must be prepared to treat such injuries when they occur. Coaches, athletes, and their families depend on the sideline physician to lead the management of athletic injuries. Furthermore, a legal precedent has been set for malpractice litigation against team physicians when an injury is mishandled.1 Although sports-related injuries to the head and neck are much less common than injuries to the extremities, an estimated 70 percent of mortality and 20 percent of permanent disability result from injuries to the head and neck.2
Because head and neck injuries often occur simultaneously, sideline physicians should associate any blow to the head with potential trauma to the neck. When assessing a conscious athlete, the physician initially evaluates the neck for spinal cord injury and determines whether the athlete can be moved safely. If the neck evaluation is normal, the athlete can be assisted to the sideline for assessment of concussion symptoms and severity.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Because sport-related head and neck injuries share the same mechanism and often occur simultaneously, evaluation of athletes with head injuries should begin with an assessment of the neck. | C | 2–4,8 |
| Football players with an abnormal neck examination after injury are presumed to have an unstable cervical spine and should be immobilized on a backboard with pads and helmet both on or both off. | B | 2,3,5–7,9,10 |
| To assess concussion, the sideline physician should ask orientation questions that evaluate recently acquired memory. | C | 11,17 |
| The Balance Error Scoring System should be used as part of the sideline evaluation to help detect concussion in athletes. | C | 17,18 |
| Brief loss of consciousness does not correlate with severity or outcome of a sports-related concussion. | C | 16,20–23,28 |
| Certain neuropsychological test batteries have been shown to reliably detect concussion in athletes. Although not particularly helpful to the sideline physician, these tests are used by professional and collegiate physicians, researchers, and those counseling players after severe or multiple concussions. | C | 13,20,23,28,30,31 |
| Athletes should not return to play until all symptoms of concussion have cleared. | C | 12–15 |
Neck Injuries
The goal in assessing neck injuries is to detect spinal cord injury and the potential for such injury resulting from instability of the cervical spine.
Cervical spine instability and the accompanying potential for neurologic loss may be commonly underdiagnosed. When 108 freshmen recruits to the University of Iowa football team underwent radiographic assessment of the neck, 35 were found to have evidence of previous cervical spine injury.3 These injuries included old compression fractures, posterior element fractures, and disk narrowing with resultant instability.
INITIAL EVALUATION IN CONSCIOUS ATHLETES
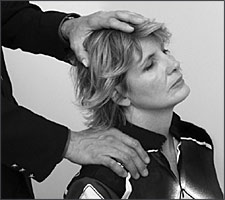
The evaluation of neck injuries requires a regimented examination and a defined management protocol. A stepwise evaluation, including a Spurling test (Figure 1), is recommended for neck injuries in conscious patients (Table 1).4 Each step in this examination presents a progressively greater risk to the spinal cord; therefore, if any part of the examination is abnormal, instability is presumed and testing is stopped. Furthermore, if an abnormality is found at any point of the examination, the neck should be immobilized and the patient prepared for transport to an emergency department.4
| 1. Note exact time of injury. Management decisions are based on duration of symptoms. |
| 2. Assess loss of consciousness. Management of unresponsive athletes should follow the ABCs of trauma care (i.e., check airway, breathing, and circulation). |
| 3. Assess peripheral strength and sensation without moving the athlete’s head or neck. |
| 4. Palpate the neck for asymmetric spasm or tenderness at the spine. |
| 5. Assess isometric neck strength without moving the athlete’s head or neck. |
| 6. Assess active range of motion at the neck. |
| 7. Perform axial compression and Spurling test (Figure 1). If negative, athlete may be moved. |
| 8. Assess recent memory and postural instability. |
| 9. Inquire about symptoms such as headache, nausea, dizziness, or blurred vision. |
Any focal neurologic symptom suggests a potential central nervous system injury. In particular, bilateral symptoms must be considered carefully.
INITIAL EVALUATION IN UNCONSCIOUS ATHLETES
The neck evaluation guideline cannot be used with unconscious athletes, and the detection of an unstable fracture is impossible. Instead, instability must be assumed, and care must be taken to avoid manipulation of the neck. In the absence of immediate danger, an unconscious injured athlete should remain at the site of the injury until the spine is fully immobilized. Three or four trained persons are required to safely “log roll” the athlete into a supine position on a backboard. This procedure may require leaving the patient at the site until emergency medical personnel arrive. The physician should remind others involved in assisting the player that preventing further injury is the priority; the athlete should not be rushed from the field for the sake of continuing play.
NECK IMMOBILIZATION
Sideline physicians must protect the spinal cord from injury whenever instability is a consideration. A cervical collar alone never should be considered adequate protection for the spinal cord. Instead, full immobilization on a backboard is required to stabilize the neck.
When immobilizing the neck, physicians should avoid movement and maintain proper alignment of the cervical vertebrae. This usually can be done with the helmet and other protective gear (e.g., shoulder pads) in place, and such equipment should not be removed. Studies using football equipment on cadavers showed that removing the helmet and shoulder pads results in excessive movement of the cervical spine.5,6 Another study used radiographs of cadavers to show that immobilizing the neck with only the helmet or only the shoulder pads in place (but not both) caused cervical spine malalignment.7 In the football setting, the athlete should be immobilized with the pads and helmet both on or both off. When direct access to the face is required, the face mask may be removed from the helmet with a screwdriver or cutting tool.
“BURNER” SYNDROME
Severe, immediate, burning pain and paresthesia radiating from the neck to one arm characterize “burners,” which are common among football players.8 The pain is usually in a C-5 to C-6 dermatomal distribution and may be associated with weakness or numbness. Burners are differentiated from serious neck injuries by their brevity, unilateral limitation of symptoms, and lack of associated pain or reduced range of motion at the neck.9 Strength testing should examine the supraspinatus, deltoid, biceps (C-5), and wrist extensor (C-6) muscles. Athletes whose symptoms resolve completely within minutes can safely return to play.10
Head Injuries and Concussion
Concussion is a clinical syndrome characterized by immediate, transient, post-traumatic impairment of neural function caused by brainstem involvement (e.g., changes in consciousness, disturbance of vision or equilibrium).11 Symptoms of concussion are neurologic in nature, occur immediately after a trauma, and are transient (Table 212)
| Altered taste or smell | |
| Amnesia or memory difficulty | |
| Anxiety | |
| Attention deficit | |
| Blurred vision | |
| Delayed verbal or motor response | |
| Dizziness, vertigo | |
| Emotional lability or irritability | |
| Fatigue | |
| Headache | |
| Impaired coordination | |
| Intolerance to light or smells | |
| Lethargy | |
| Loss of consciousness | |
| Nausea, vomiting | |
| Postural instability | |
| Sleep disturbance | |
| Tinnitus | |
| Vacant stare |
Concussion is common in sports; by conservative estimates, there are more than 300,000 sports-related concussions in the United States each year.13 However, studies of relatively mild brain injuries, such as those typically sustained in sports, are limited. As a result, there is no universal agreement on clinical markers of concussion severity or the appropriate management of these injuries. The two best-known guidelines for the management of concussion are presented in Table 314,15 and Table 4.12 Since the publication of these guidelines, new evidence has become available.
| Grade | Description | Management |
|---|---|---|
| 1 | No LOC |
|
| PTA* or symptoms lasting less than 30 minutes | ||
| 2 | LOC less than one minute, or PTA* or symptoms lasting more than 30 minutes |
|
| 3 | LOC more than one minute, or PTA* or symptoms lasting more than 24 hours |
|
| Grade | Description | Management |
|---|---|---|
| 1 | Transient confusion |
|
| No LOC | ||
| Symptoms lasting less than 15 minutes | ||
| 2 | Transient confusion |
|
| No LOC | ||
| Symptoms lasting more than 15 minutes | ||
| 3 | Any LOC |
|
EVALUATING NEUROLOGIC STATUS
Orientation vs. Recent Memory
Orientation questions concerning time and place, which are components of the Mini-Mental Status Examination, are less sensitive in detecting concussion than questions that assess recent memory.11 A series of questions can be used to assess recent memory in athletes with possible concussion:
At which field are we playing?
What team are we playing?
Which quarter (period, half) is it?
How far into the quarter (period, half) is it?
Which team scored last?
What team did we play last week?
Did we win?16
Postural Instability
The Balance Error Scoring System is a screening tool that may be used by the sideline physician to assist in determining return-to-play readiness; it can be administered in minutes at the sideline using only a block of foam.18 Athletes are asked to close their eyes and hold their hands at their hips while assuming six trials for 20 seconds each. Trials consist of three stances (i.e., double-, tandem-, and single-leg) on two surfaces (firm and foam). Athletes are watched for balance errors (i.e., stepping, stumbling, opening eyes, lifting hands from the iliac crests, lifting forefoot or heel, moving hip into more than 30 degrees of f lexion or abduction, or remaining out of the test position for more than five seconds). After a concussion, athletes typically have at least 12 errors in this series of trials.18
Loss of Consciousness
The presence of loss of consciousness (LOC) does not correlate with the severity or outcome of a concussion.19–23 To date, multiple studies have shown no statistical relationship between brief LOC and postconcussive impairment.19–23 There is mounting evidence that brief LOC may not be a reliable marker of severity in sports-related brain trauma. Rarely, however, LOC can signify serious vascular brain injuries such as hematomas. As a result, current guidelines recommend that athletes who experience LOC should not return to play on the day of the injury.24
REPEATED CONCUSSIONS AND SECOND IMPACT SYNDROME
The effects of repeated concussion are not well understood. Studies have shown that an initial concussion increases the likelihood of subsequent concussion four- to sixfold.25,26 However, it is not known if this risk is the result of brain injury or an aggressive playing style. Repeated concussions do not result in greater neurocognitive impairment than that caused by previous concussions of similar severity.27 However, repeated concussions result in more reported symptoms and a greater risk of persistent postconcussion symptoms.27
A possible explanation for sudden collapse and death among athletes is the second impact syndrome theory. This theory refers to rapid swelling of the brain that presumably occurs when a second head trauma is sustained before the symptoms of a previous concussion resolve.28 Athletes with second impact syndrome remain alert for several seconds before they collapse; they may suffer brainstem herniation and die from respiratory failure. The existence of this syndrome has been questioned. Only 17 cases were reported between 1984 and 1997, most of which reportedly had insufficient evidence of either a first or a second head trauma.19 A critical appraisal of those cases concluded that second impact syndrome probably does not exist or has been overdiagnosed.29 In addition, sudden collapse and death are known to occur after a single blow to the head. Persons who question the syndrome note that traumatic brain swelling is poorly understood and may be unrelated to a second impact.
NEUROPSYCHOLOGICAL TESTING
The assessment of concussion is hindered by its dependence on reported symptoms. Because LOC is an unreliable marker of severity and because athletes commonly underreport their symptoms, neuropsychological testing has been proposed as a method to detect concussion after sports-related injuries. Although studies indicate that these tests objectively measure the persistent effects of concussion,13,20–23,30 neuropsychological testing requires considerable time for administration (i.e., two to four hours) and must be interpreted by a neuropsychologist, making it impractical for use at the sideline.31
Some of the problems associated with neuropsychological testing can be overcome by computer-based testing programs, which are commonly used by collegiate and professional sports teams to assist in return-to-play decisions. However, any use of neuropsychological tests should be done with an understanding of their limitations. The tests are designed to detect a change from baseline, and two preseason assessments may be needed to establish a baseline. This repeated administration may allow some athletes to practice some components of the tests. Furthermore, there is no agreement on a cutoff point for “abnormal” that would minimize missed concussions or unnecessary play restrictions. There also is no agreement on test selection or on the amount of recovery necessary to allow a safe return to play.13 Finally, the limited data that exist on the use of these tests in female athletes and adolescents suggest that neuropsychological tests are less reliable in adolescents and require separate “normal” values for female athletes.32
APPROACH TO PATIENTS WITH CONSUSSION
Sideline physicians can conduct an evaluation of athletes with concussion in a stepwise manner: (1) assess for LOC; (2) inquire about symptoms commonly associated with concussion; (3) evaluate recently acquired memory; and (4) evaluate postural stability.
Team physicians should restrict from play any athlete with persistent symptoms of concussion because these symptoms place them at risk of reinjury if they return prematurely. In addition, concussion is defined by transient symptoms, and until those symptoms resolve, other diagnoses must be considered.
Athletes with memory loss, imbalance, or symptoms reported 15 minutes after the injury should be restricted from play for the rest of the day. Athletes with neurologic symptoms persisting longer than 30 minutes—particularly those with prolonged LOC or any focal neurologic sign—should be monitored closely and may require transport to an emergency department. Finally, athletes with seizures, persistent vomiting, or suspected skull fracture should be urgently evaluated in an emergency department.