
Am Fam Physician. 2007;75(2):194-202
A more recent article on patellofemoral pain syndrome is available.
Patient information: See related handout on patellofemoral pain syndrome, written by the authors of this article.
Author disclosure: Nothing to disclose.
Patellofemoral pain syndrome (PFPS) is the most common cause of knee pain in the outpatient setting. It is caused by imbalances in the forces controlling patellar tracking during knee flexion and extension, particularly with overloading of the joint. Risk factors include overuse, trauma, muscle dysfunction, tight lateral restraints, patellar hypermobility, and poor quadriceps flexibility. Typical symptoms include pain behind or around the patella that is increased with running and activities that involve knee flexion. Findings in patients with PFPS range from limited patellar mobility to a hypermobile patella. To confirm the diagnosis, an examination of the knee focusing on the patella and surrounding structures is essential. For many patients with the clinical diagnosis of PFPS, imaging studies are not necessary before beginning treatment. Radiography is recommended in patients with a history of trauma or surgery, those with an effusion, those older than 50 years (to rule out osteoarthritis), and those whose pain does not improve with treatment. Recent research has shown that physical therapy is effective in treating PFPS. There is little evidence to support the routine use of knee braces or nonsteroidal anti-inflammatory drugs. Surgery should be considered only after failure of a comprehensive rehabilitation program. Educating patients about modification of risk factors is important in preventing recurrence.
Patellofemoral pain syndrome (PFPS) is the most common diagnosis in outpatients presenting with knee pain. Studies have shown PFPS to be the most common single diagnosis among runners and in sports medicine centers.1,2 Eleven percent of musculoskeletal complaints in the office setting are caused by anterior knee pain (which most commonly results from PFPS), and PFPS constitutes 16 to 25 percent of all injuries in runners.1,3,4
The diagnosis of PFPS is made clinically, and although management can be challenging, a well-designed, nonoperative treatment program usually allows patients to return to recreational and competitive activities. The following provides an update on the clinical evaluation and treatment of patients with PFPS.
Definition
The term “PFPS” is often used interchangeably with “anterior knee pain” or “runner's knee.” PFPS can be defined as anterior knee pain involving the patella and retinaculum that excludes other intraarticular and peri-patellar pathology.5 Chondromalacia patellae, a condition in which there is softening of the patellar articular cartilage, occurs in only a subset of patients who present with anterior knee pain.5–7
Anatomy and Biomechanics
The patellofemoral joint comprises the patella and the femoral trochlea. The patella acts as a lever and also increases the moment arm of the patellofemoral joint, the quadriceps and patellar tendons.8 Contact of the patella with the femur is initiated at 20 degrees of flexion and increases with further knee flexion, reaching a maximum at 90 degrees.9
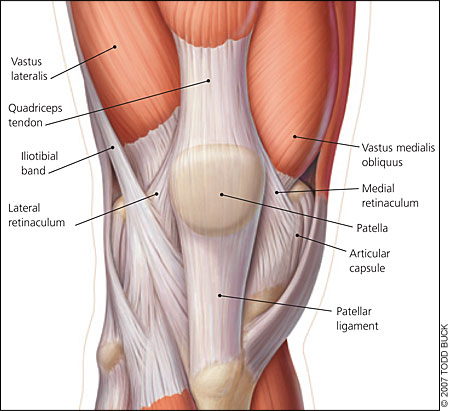
Stability of the patellofemoral joint involves dynamic and static stabilizers (Figure 1), which control movement of the patella within the trochlea, referred to as “patellar tracking.” Patellar tracking can be altered by imbalances in these stabilizing forces affecting the distribution of forces along the patellofemoral articular surface, the patellar and quadriceps tendons, and the adjacent soft tissues. Forces on the patella range from between one third and one half of a person's body weight during walking to three times body weight during stair climbing and up to seven times body weight during squatting.10 Abnormalities of patellar tracking must be understood to appreciate the possible causes of PFPS and to determine the focus of treatment.
Risk Factors
| Anatomic anomalies (e.g., hypoplasia of the medial patellar facet, patella alta) |
| Malalignment and altered biomechanics of the lower extremity (static or dynamic) |
| Muscle dysfunction (e.g., quadriceps weakness, improper firing pattern) |
| Patellar hypermobility |
| Poor quadriceps, hamstring, or iliotibial band flexibility |
| Previous surgery |
| Tight lateral structures (i.e., lateral retinaculum and iliotibial band) |
| Training errors or overuse |
| Trauma |
Lower extremity malalignment (caused by abnormalities such as an increased standing Q angle, pes planus, or subtalar pronation) often has been implicated as a cause of PFPS. However, evidence to support a causal relationship between static measures of lower extremity malalignment and lower extremity injury is limited.11,16,17 In one prospective study, a small subgroup of runners with PFPS was found to have differences in ankle dorsiflexion, genu varum, and forefoot varus compared with noninjured participants.11 Analyses that include a dynamic component may eventually yield more useful information on the role of lower extremity morphology in the development of PFPS.11
Diagnosis
| Cause | Comment |
|---|---|
| Articular cartilage injury | May describe history of trauma; mechanical symptoms may occur if loose body present; may have effusion; may have tenderness of involved structure (e.g., femoral condyles, patella) |
| Bone tumors | Pain may be insidious; may have tenderness of bony structures |
| Chondromalacia patellae | Retropatellar pain; may have history of trauma; may have effusion on examination |
| Hoffa's disease | Pain and tenderness localized to infrapatellar fat pad |
| Iliotibial band syndrome | Typically presents with lateral pain and tenderness over lateral femoral epicondyle |
| Loose bodies | Symptoms variable; may have intermittent sharp pain, locking, or effusion |
| Osgood-Schlatter disease | Tenderness and swelling at insertion of patellar tendon at tibial tubercle in an adolescent |
| Osteochondritis dissecans | Symptoms variable; may have intermittent pain, swelling, or locking |
| Patellar instability/subluxation | Intermittent pain with sensation of instability or movement of patella; may have swelling; locking can occur with loose body formation; may have tenderness over medial retinaculum |
| Patellar stress fracture | May have tenderness directly over patella |
| Patellar tendinopathy | Tenderness of tendon; tendon may be thickened if chronic |
| Patellofemoral osteoarthritis | May have crepitus or effusion; characteristic radiographic findings |
| Patellofemoral pain syndrome | Anterior knee pain “behind” or around patella; usually no effusion; may have findings of patellar maltracking |
| Pes anserine bursitis | Pain usually described as medial rather than anterior; tenderness over pes anserine bursa |
| Plica synovialis | May be medial or lateral to patella; if symptomatic, tenderness can be demonstrated on examination |
| Prepatellar bursitis | Characteristic swelling anterior to patella following trauma |
| Quadriceps tendinopathy | Tenderness over tendon |
| Referred pain from the lumbar spine or hip joint pathology | Symptoms depend on origin of pain; knee examination usually normal |
| Saphenous neuritis | Pain usually medial but poorly localized; may have history of surgery |
| Sinding-Larsen-Johansson syndrome | Tenderness at patellar tendon insertion at inferior pole of patella in an adolescent |
| Symptomatic bipartite patella | May have tenderness directly over patella with characteristic radiographic findings |
HISTORY
Patients with PFPS typically describe pain “behind,” “underneath,” or “around” the patella. The symptoms are usually of gradual onset, although some cases can be caused by trauma, and may be bilateral. Common symptoms include stiffness or pain, or both, on prolonged sitting with the knees flexed (sometimes called the “theater sign”), and pain with activities that load the patellofemoral joint, such as climbing or descending stairs, squatting, or running. The pain can be difficult for the patient to localize. If asked to point to the location of pain, patients may place their hands over the anterior aspect of the knee or draw a circle with their fingers around the patella (the “circle sign”). The pain usually is described as “achy,” but it can be sharp at times.
Patients may complain of the knee giving way. This usually does not represent true patellar instability but rather transient inhibition of the quadriceps because of pain or deconditioning.13 However, it is important to determine whether patellar subluxation or dislocation has occurred, because patellar instability can be associated with PFPS.
Swelling of the knee is not characteristic of PFPS, although patients may report a sensation of stiffness, especially when the knee is flexed. A “popping” or “catching” sensation may be described. Locking of the joint is not a symptom of PFPS and suggests a meniscal tear or loose bodies.
Because PFPS often is related to overuse, recent changes in activities and any changes in the frequency, duration, and intensity of training should be noted. Other possible contributors include inappropriate or excessively worn footwear, and lower extremity resistance training and conditioning activities (particularly squats and lunges). A history of injuries, including patellar subluxation or dislocation, trauma, or surgeries, should be noted because they may cause direct injury to the articular cartilage or alter the forces across the patellofemoral joint, resulting in anterior knee pain.
PHYSICAL EXAMINATION
| Component and finding | Comment | ||
|---|---|---|---|
| Inspection | |||
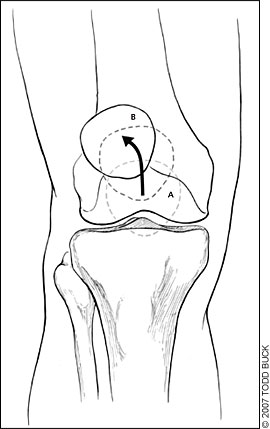
| Lateral patellar tracking (“J” sign; Figure 2) | Suggests patellar maltracking as a result of tight lateral restraints or VMO dysfunction | ||
| Poor VMO tone | May be displayed in PFPS | ||
| Palpation | |||
| Effusion | Rare in PFPS; should prompt evaluation for other causes of pain | ||
| Tenderness of: | |||
| Medial or lateral retinaculum | Common in PFPS; tenderness of the medial retinaculum also may be found in patellar instability | ||
| Medial and lateral facets | May be found in PFPS; may indicate articular cartilage injury | ||
| Patella | Usually not tender in PFPS; may indicate patellar contusion or stress reaction; can be tender in symptomatic bipartite patella; tenderness at insertion sites of quadriceps and patellar tendons can be found in tendinopathies and Sinding-Larsen-Johansson syndrome | ||
| Quadriceps and patellar tendons | Suggestive of tendinopathy or tear if injury is acute | ||
| Pes anserine bursa | Tenderness and swelling typical of pes anserine bursitis | ||
| ITB, lateral femoral epicondyle | Suggests ITB syndrome | ||
| Surface of medial or lateral femoral condyles | Direct tenderness suggests contusion or articular cartilage injury; may be tender with injuries of the collateral ligaments | ||
| Infrapatellar fat pad | May be seen in Hoffa's disease | ||
| Joint line | Suggests meniscal injury | ||
| Plica synovialis | Nontender plicae may be found in asymptomatic knees; tenderness that reproduces symptoms denotes plica syndrome | ||
| Range of motion | Knee and hip range of motion usually normal in PFPS | ||
| Crepitus | Nonspecific finding; may occur with PFPS; can be appreciated in asymptomatic knees and those with osteoarthritis | ||
| Popping/clicking | Patella may produce a palpable pop, click, or clunk with palpation during passive or active range of motion; may be a sign of patellar maltracking, perhaps caused by synovial hypertrophy, plica synovialis, or cyst formation; a popping sensation with marked lateral deviation of the patella in extension indicates patellar instability | ||
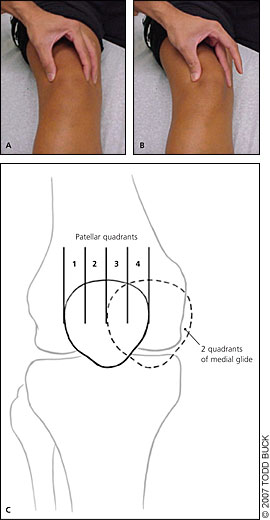
| Patellar glide (Figure 3) | Assesses patellar mobility; displacement of less than one quadrant indicates tight lateral structures; displacement of more than three quadrants suggests patellar hypermobility caused by poor medial restraints | ||
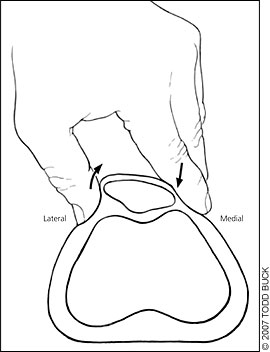
| Patellar tilt (Figure 4) | Positive test (i.e., lateral aspect of patella is fixed and cannot be raised to at least horizontal position) indicates tight lateral structures | ||
| Patellar grind (Figure 5) | Pain with test may indicate PFPS; must be compared with contralateral knee | ||
| Patellar apprehension | Positive test (i.e., pain or discomfort with lateral translation of the patella) suggests lateral patellar instability as a cause of pain | ||
| Flexibility | Flexibility of quadriceps, hamstrings, ITB, hip flexors, and gastrocnemius should be assessed routinely | ||
Inspection. Patients initially should be examined “from the ground up” while standing in shorts. Although the clinical utility of static measurements of lower extremity alignment appears to be limited, such measurements may be performed at this point in the examination. Observation of the patient's gait may reveal excessive subtalar pronation.
Dynamic patellar tracking can be assessed by having the patient perform a single leg squat and stand. Imbalance between the medial and lateral patellar forces (caused by vastus medialis obliquus [VMO] dysfunction or lateral structure tightness) can be manifested by an abrupt medial deviation of the patella as the patella engages the trochlea early in flexion, known as the “J” sign.13 Alternatively, the “J” sign may be observed with the patient supine or seated and the knee extended from a flexed position. Lateral deviation of the patella can be observed during the terminal phase of extension (Figure 2).18
Quadriceps muscle bulk, especially the VMO, should be assessed by visual inspection and comparison with the opposite side. Measurement of quadriceps muscle girth can be used as a baseline in assessing progress with rehabilitation. Any surgical scars should be noted.
Palpation. This portion of the examination should be performed with the patient supine and the knee extended. The knee should be assessed for an effusion. A joint effusion is uncommon in PFPS and should prompt evaluation for other causes of knee pain. Quadriceps muscle tone can be assessed by direct palpation at rest and with isometric contraction. Careful palpation should be performed in an attempt to isolate the location of the pain (Figure 1; Table 312,13 ). The ligaments also should be examined as part of the comprehensive examination.
Range of Motion. Passive and active range of motion of the knee and hip should be assessed. Pain with internal or external rotation of the hip could indicate referred pain resulting from hip joint pathology and should be evaluated further. Patients with PFPS usually demonstrate a full range of motion of the knee. Asymptomatic crepitus with range of motion is a nonspecific finding, although painful crepitus may indicate an articular cartilage injury or osteoarthritis.
Special Aspects. Clinical tests for patellar mobility and position, and provocative tests for pain should be performed. The patellar glide (Figure 314 ), patellar tilt (Figure 418 ), and patellar grind (Figure 5) tests should be performed as part of the routine assessment of patients with anterior knee pain (Table 312,13 ). Positive results on these tests are consistent with the diagnosis of PFPS. The patellar apprehension test is used to assess for lateral instability and is positive when pain or discomfort occurs with lateral translation of the patella.

Medial patellar instability can be assessed by displacing the patella medially with the knee extended, then flexing the knee and releasing the patella. Pain indicates medial subluxation.14 Finally, flexibility of the iliotibial band (ITB), quadriceps, hamstrings, hip flexors, and the gastrocnemius should be evaluated. Tightness of the ITB and tightness of the quadriceps have been shown to be risk factors for PFPS.15,19 Poor flexibility in these areas may contribute to stress across the patellofemoral joint, and attention should be directed to this in therapy.
Imaging
PFPS is primarily a clinical diagnosis and, for many patients, treatment can be initiated without imaging. Radiography is an adjunct to the history and physical examination and should be performed in patients with a history of trauma or surgery, those with an effusion, and those whose pain does not improve with treatment. Radiography also may be helpful if a symptomatic bipartite patella is suspected.
In persons older than 50 years, radiography should be considered to assess for patellofemoral osteoarthritis. In patients who are skeletally immature, radiography may be helpful to evaluate for other causes of anterior knee pain, such as osteochondritis dissecans, physeal injury, or bone tumors. Other radiographic findings that may mimic PFPS include loose bodies and occult fractures.
When indicated, radiography should include the following views: weight-bearing anterior-posterior, weight-bearing true lateral, and axial. The axial view is taken with 20 to 45 degrees of knee flexion. Abnormalities of lateral patellar displacement, lateral patellar tilt, and dysplasia of the trochlea can be assessed on the axial view. Although these findings may indicate malalignment, they also may be seen in asymptomatic patients and are not predictive of outcome.20,21 In symptomatic patients, such findings, in combination with the physical examination, may assist in tailoring treatment.
Computed tomography and magnetic resonance imaging (MRI) are not necessary for most patients with PFPS. MRI can be helpful in detecting articular cartilage injuries, chondromalacia patellae, patellar stress fractures, and loose bodies. In addition, a pattern of marrow edema involving the medial aspect of the patella and the lateral aspect of the femoral condyle, and tears of the patellofemoral ligament can be seen with MRI and are suggestive of patellar subluxation or dislocation.
Treatment
The management of PFPS should focus on the implementation of a comprehensive rehabilitation program. It is important to communicate to the patient that a successful return to recreational or competitive activities requires compliance with the rehabilitation plan.
RELATIVE REST
Reduction of loading to the patellofemoral joint and surrounding soft tissues is the first step to reduce pain. If resistance training exercises have been identified as playing a role in causing the injury, cessation of specific exercises such as full squats and lunges is indicated. Runners should reduce mileage to a level that does not provoke pain (while running or the day after running). Alternative activities such as bicycling, swimming, or the use of an elliptical trainer can be used to maintain fitness while treatment is ongoing. Ice or other methods of cold application may further reduce symptoms. Heat is generally not recommended. Patients may find ice application after activity particularly helpful. Although symptoms usually abate with these methods, further treatment is necessary to avoid recurrence.
PHYSICAL THERAPY
A well-structured rehabilitation program is the mainstay of treatment. Several studies have shown physical therapy to be effective in treating PFPS.21–24 However, there is no one program that will be effective for all patients. The rehabilitation program should focus on correcting maltracking of the patella by addressing the findings identified on the physical examination. Some patients may require significant strengthening of the quadriceps. Others may have excellent quadriceps strength but excessively tight lateral structures or poor quadriceps flexibility. Soft tissue techniques and flexibility exercises can be helpful for these patients. A detailed assessment of the imbalances of patellar tracking is therefore essential to tailoring treatment. Specific exercises can then be prescribed as part of a home rehabilitation program. Patients who require further assessment or ongoing instruction can be referred to a physical therapist.
ADDRESSING THE UNDERLYING CAUSE
In most patients with PFPS, a careful history will identify a precipitating event. Changes in activity patterns, such as an increase in running mileage, running stadium steps for conditioning, or the addition of resistance training exercises that affect the patellofemoral joint, often are associated with symptom onset. Excessively worn or inappropriate footwear also may contribute. Discussing these issues with the patient and developing a specific plan to avoid repeating the causal behavior are important in preventing a recurrence.
OTHER TREATMENTS
Analgesics. Although nonsteroidal anti-inflammatory drugs (NSAIDs) are commonly prescribed for patients with PFPS, there is little evidence supporting their effectiveness.25 NSAIDs or acetaminophen may be considered at the initiation of treatment for patients with symptoms during daily activities and for those whose symptoms are not controlled with ice applications.
Patellar Taping. Patellar taping has been suggested as a method to treat PFPS by improving alignment and quadriceps function. Although the results from uncontrolled studies were encouraging, the results of three randomized clinical trials have not been consistent: two found no benefit when patellar taping was added to a program of physical therapy.29–31 More studies are needed to determine the role of patellar taping in treating PFPS.
Foot Orthoses. As discussed above, prospective studies have yet to demonstrate strong relationships between static measures of lower extremity malalignment and lower extremity injuries. Moreover, alignment was not found to be predictive of outcome in patients with PFPS in two long-term studies.32,33 Other studies, however, have shown that orthoses can be effective in some patients with PFPS.22,34 Over-the-counter soft orthoses are a reasonable choice for patients who have PFPS with malalignment. For those with persistent symptoms, a custom orthotic can be considered.
Long-term Outcomes
There are few long-term studies on the treatment of PFPS. Two studies in which patients were instructed on a program of home exercises reported successful outcomes in approximately 75 to 85 percent of patients with PFPS.33,35 A study of athletes who visited a sports medicine clinic and were instructed on VMO training found that 54 percent were pain free or had mild symptoms after nearly six years.36 Interestingly, arthroscopy findings of the patellar articular surface have not been shown to be predictive of outcome.33 Findings associated with a poorer result include a hypermobile patella, older age, bilateral symptoms, and patellar pain and crepitation on examination.35,36
Surgical Consultation
Surgical consultation for PFPS may be considered for those patients whose symptoms persist despite their completing at least six to 12 months of a thorough program of rehabilitation, and in whom other causes of anterior knee pain have been excluded.
Most studies of surgical treatment for patellofemoral disorders are uncontrolled case series. Controlled studies of surgical outcomes are limited and are highly dependent on proper patient selection. Because it is essential that the surgical procedure specifically address the individual characteristics of patellar maltracking in each patient, consultation should be obtained from a surgeon with significant experience in treating patellofemoral joint disorders.
Surgical options include release of the lateral retinaculum, articular cartilage procedures, proximal realignment, and distal realignment—often with antero-medialization of the tibial tubercle.14 Patients with tight lateral structures may benefit from lateral release, with proximal realignment in some cases. Distal realignment with anteromedialization of the tibial tubercle may benefit those with lateral compression and associated articular cartilage injury. A full discussion of the various surgical procedures and indications is beyond the scope of this review.