
Am Fam Physician. 2008;77(3):282
Author disclosure: Nothing to disclose.
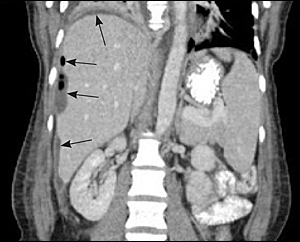
to the editor: A 27-year-old woman presented with a two-day history of right upper quadrant (RUQ) pain four days after giving birth to her first child. She had a spontaneous vaginal delivery after labor induction for post-dates. On the second postpartum day, she had an episode of severe right-sided abdominal pain after bending over. This pain resolved and she was discharged later that day with normal vital signs and laboratory results. She presented to the emergency department with worsening RUQ pain (now described as 10/10 on a pain scale), intermittent shortness of breath, and lower extremity edema. Vital signs were notable only for mild tachycardia, with pulse oximetry of 95 percent on room air. Radiographs showed RUQ gas with an air fluid level, as well as a right pleural effusion and basilar opacity. Abdominal/pelvic computed tomography showed abnormal fluid collection in the subdiaphragmatic, lateral subhepatic, and capsular regions extending into the right paracolic gutter (see accompanying figure). The appendix was not visualized, and the uterus was consistent with her postpartum state. A ruptured appendix was suspected, and found upon laparotomy, along with a large abscess extending up the right gutter to the diaphragm. The incision was left open, and closed six days later. A peritoneal fluid culture grew a mixture of gram positive and negative and anaerobic organisms. She was discharged with antibiotics and recovered.
Acute appendicitis is the most common condition requiring surgery during pregnancy, with an incidence of 0.4 to 1.4 per 1,000 pregnancies.1 Although the incidence of appendicitis is not increased during pregnancy, rupture of the appendix occurs two to three times more frequently than in non-pregnant patients secondary to delayed diagnosis. Although the literature contains many case series of appendicitis complicating pregnancy, only several1–3 include postpartum cases, comprising 6 to 19 percent of all cases in these series. In the two case series that separated data for the postpartum period, typical abdominal findings and tachycardia were often absent.1,2 In the third trimester and postpartum period, time from onset of symptoms to operation was longer, with rupture being more likely.
Abdominal guarding and rigidity, hallmarks of the acute abdomen, may not be present in the puerperium, likely because of decreased muscle tone of the abdominal wall.4 The white blood cell count and erythrocyte sedimentation rate will be normally elevated, making the diagnosis more difficult.
Round ligament pain, contractions, and other causes of abdominal pain can mimic appendicitis during pregnancy, and postpartum appendicitis can be confused with uterine involution, incisional pain from cesarean delivery, and urinary tract infection. Appendicitis in the postpartum period can be difficult to diagnose because of its frequent atypical presentation, and overlap of symptoms with other postpartum conditions.