
Am Fam Physician. 2009;80(10):1096-1102
A more recent article on common fractures of the radius and ulna is available.
Author disclosure: Nothing to disclose.
Fractures of the forearm are common injuries in adults. Proper initial assessment includes a detailed history of the mechanism of injury, a complete examination of the affected arm, and appropriate radiography. Open fractures, joint dislocation or instability, and evidence of neurovascular injury are indications for emergent referral. Fractures demonstrating significant displacement, comminution, or intra-articular involvement may also warrant orthopedic consultation. In the absence of these findings, many forearm fractures can be managed by a primary care physician. Initial management of forearm fractures should follow the PRICE (protection, rest, ice, compression, and elevation) protocol, with the exception of compression, which should be avoided in the acute setting. Distal radius fractures with minimal displacement can be treated with a short arm cast. Isolated ulnar fractures can usually be managed with a short arm cast or a functional forearm brace. Mason type I radial head fractures can be treated with a splint for five to seven days or with a sling as needed for comfort, along with early range-of-motion exercises. Patients with an olecranon fracture are candidates for nonsurgical treatment if the elbow is stable and the extensor mechanism is intact.
Upper extremity fractures are often evaluated by primary care physicians at the patient's initial presentation or at follow-up after the emergency department. These fractures account for approximately 2 million emergency department visits annually.1 Eighteen percent of the visits are for humeral fractures; 31 percent are for radial or ulnar fractures; and 51 percent are for carpal, metacarpal, or phalangeal fractures. Falls are the leading cause of upper extremity fractures.2
Initial fracture management generally follows the traditional PRICE (protection, rest, ice, compression, and elevation) protocol. The injured arm should be protected and placed at rest using splinting and a sling. Ice and elevation can help control pain and swelling. In the acute setting, compression of the limb should be avoided because of possible complications from swelling, such as acute compartment syndrome. Analgesics may be prescribed as necessary for pain control. Definitive treatment of forearm fractures can range from functional bracing to surgical fixation. Because loss of mobility is the most common complication, early mobilization is usually recommended.3
| Clinical recommendation | Evidence rating | References | Comments |
|---|---|---|---|
| Nonsurgical treatment of displaced intra-articular fractures of the distal radius is associated with an increased risk of radiocarpal arthritis. | C | 4, 6, 7, 11 | Expert opinion suggests that even minimal articular incongruency is associated with increased complications |
| Isolated ulnar shaft fractures that are not displaced by more than 50 percent of the bone diameter and that are angulated less than 10 degrees can be treated with a functional brace or short arm cast. | C | 16 | Based on systematic review of treatment methodologies (not RCTs) |
| Early mobilization is favored in the treatment of Mason type I radial head fractures. | A | 20, 21, 23 | Based on consistent findings from several RCTs |
| There is no benefit of casting in the initial treatment of Mason type I radial head fractures. | B | 21 | Based on one RCT |
Initial Evaluation
The goals of initial evaluation of forearm fractures are to define the mechanism of injury, delineate the extent of the fracture, and identify any additional injuries. This requires a thorough examination of the entire arm. Any breaks in the skin must be assessed to rule out the possibility of an open fracture. Joint dislocation, open fractures, and neurovascular injury are among the indications for immediate orthopedic referral (Table 1).4–7 Neurovascular examination includes assessment of capillary refill, as well as pulses in the radial and ulnar arteries. Sensory and motor function of the hand and wrist should be documented, with focus on the function of the median nerve because of its propensity for injury in forearm trauma.
| Absolute indications |
| Joint dislocation |
| Joint instability |
| Neurovascular injury |
| Open fractures |
| Relative indications |
| Comminution |
| Displacement |
| Intra-articular involvement |
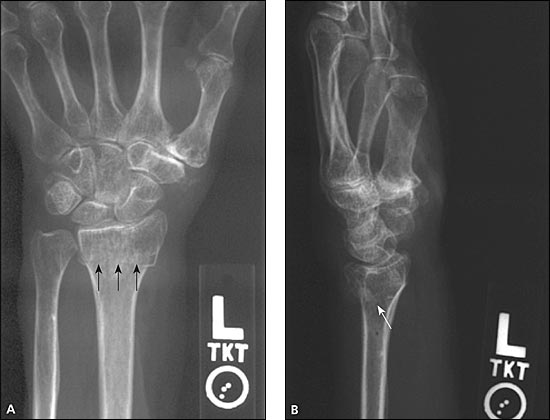
Much of the subsequent management is based on the radiologic evaluation of the fracture. Standard radiography should include posteroanterior and lateral views. Oblique views can be used to supplement the basic series if the presence of a fracture remains in doubt. Small, occult, or intra-articular fractures may not be noted on initial radiography. An anterior fat pad is normally visualized at the elbow, but an effusion will cause elevation of the fat pad (sail sign). A posterior fat pad is an abnormal finding.8 The presence of a sail sign or a visualized posterior fat pad is evidence of a fracture or other intra-articular process (Figure 1). In the presence of recent trauma, patients with a visualized posterior fat pad and no other evidence of skeletal trauma should be treated as though a fracture has occurred. When suspicion of a fracture is high, it is appropriate to perform repeat radiography in 10 to 14 days. If immediate confirmation or exclusion of fracture is required, or if there is a question about the presence of joint instability or associated ligamentous injury, magnetic resonance imaging may be performed.

Types of Fractures
DISTAL RADIUS FRACTURES
Distal radius fractures, also known as Col-les fractures, represent up to one sixth of all fractures treated. They are most common in young adults and in older persons.4 The mechanism of injury tends to be different in these two groups, with the younger population generally sustaining fractures from high-energy trauma and the older population usually experiencing a low-impact injury, such as from a simple fall.
These fractures traditionally have been treated with closed manipulation and casting. However, it is now recognized that many of these fractures are unstable, and casting may not maintain acceptable reduction.5 Additionally, advancements in surgical technique have improved fracture stability, allowing for earlier motion and rehabilitation.5
Much of the evidence to support various treatment methods is undeveloped. Cochrane reviews of randomized controlled trials of surgical and medical interventions for distal radius fractures in adults found insufficient evidence to guide treatment.9,10 Because of this, treatment decisions are often guided by physician experience and expert opinion.
For primary care physicians, initial management includes deciding whether to refer the patient to an orthopedist. A young, active patient with an occupation or hobby that requires a highly functional hand and wrist may prefer to be treated more aggressively than an older, sedentary patient who is more interested in pain relief and who can tolerate some loss of motion. Because nonsurgical treatment of persons with intra-articular fractures increases the risk of complications, such as radiocarpal arthritis,4,6,7,11 a referral should be strongly considered for any fracture that extends into the radiocarpal joint or the distal radioulnar joint. Additionally, fractures that require reduction are potentially unstable and may require surgical fixation.7,11,12 Unless the primary care physician has extensive experience with fracture management, it is best to refer patients with distal radius fractures requiring manipulation to an orthopedic surgeon.
A complete radiologic evaluation of a distal radius fracture requires at least two views (posteroanterior and lateral) of the wrist. Oblique radiography is often required to fully assess the extent of the fracture. The radiographs should be scrutinized for intra-articular fractures, carpal injuries, dislocation of the distal radioulnar joint, and other associated fractures, such as those of the ulnar styloid. The presence of any of these findings warrant consideration for orthopedic referral.
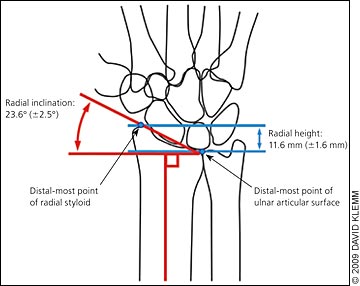
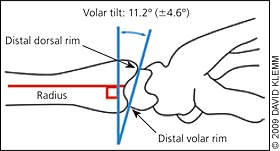
Angulation and displacement of the fracture can be assessed on radiography by measuring radial height, radial inclination, and volar tilt. The radiologist can provide these upon request. Figures 2 and 3 illustrate these measurements.13 Opinions vary as to the amount of displacement that is tolerable, but it is generally accepted that the likelihood of a poor outcome increases the further each parameter deviates from the norm. Indications for reduction and referral include loss of volar tilt with resulting dorsal angulation of the distal radial articular surface of greater than 5 to 10 degrees, change in radial inclination of greater than 5 to 10 degrees, or radial shortening of greater than 2 mm.5–7,14
Distal radius fractures that are minimally displaced or impacted (Figure 4) can be treated with immobilization for four to eight weeks.5,11,12 Initially, a volar or sugar-tong splint may be necessary if there is significant swelling. Definitive treatment should be based on fracture characteristics and patient preferences. Younger patients with good bone health and nondisplaced fractures often can be treated with a volar splint, whereas patients with minimal displacement or osteoporotic bone should have the extra protection of a short arm cast.5,11,12 The University of Ottawa, Ontario, Canada, offers video demonstrations of proper casting and splinting techniques at http://intermed.med.uottawa.ca/procedures/cast. It is imperative to perform weekly radiography for the first three weeks because even fractures that appear stable may displace during early treatment, particularly in older patients.6 Any cast or splint should not obstruct motion of the elbow, metacarpophalangeal joint, or fingers.
MIDFOREARM FRACTURES
Fractures of the radius and ulna (both-bone fractures) are complex and difficult to treat successfully.11,15 Nondisplaced fractures may displace despite external immobilization.11 Isolated radial shaft fractures are also difficult to manage. Patients with these fractures should be referred to an orthopedist unless the primary care physician has significant experience in this treatment.
Although they are uncommon, isolated ulnar shaft fractures can be successfully treated with conservative methods. Commonly referred to as nightstick fractures, many ulnar shaft fractures are caused by a direct blow to a raised forearm.16 Full evaluation requires posteroanterior and lateral radiography of the entire forearm, including the wrist and elbow. The physician must ensure that there is no associated dislocation of the radial head in fractures of the proximal one third of the ulna (i.e., Monteggia fracture), because these require orthopedic consultation. Isolated ulnar shaft fractures that are not displaced by more than 50 percent of the bone diameter and that are angulated less than 10 degrees can be treated with a short arm cast or a functional forearm brace for four to eight weeks.11,15–17 A functional brace allows unrestricted motion of the wrist and elbow, reducing the risk of postimmobilization stiffness. If a short arm cast is used initially, it should be replaced with a functional brace after approximately two weeks. Radiography should be repeated weekly for the first three weeks to detect fracture displacement.
RADIAL HEAD FRACTURES
Radial head fractures account for up to 5.4 percent of all fractures and about 33 percent of elbow fractures.18 They are usually caused by a fall on an outstretched hand with a pronated forearm or with the elbow in slight flexion, or a direct blow to the lateral elbow. Forearm movements are painful and limited with radial head fractures. Tenderness can be elicited over the radial head distal to the lateral epicondyle. Standard radiography is generally adequate, although an oblique or radiocapitellar view may be necessary.
Radial head fractures are classified using the Mason system (Table 2).19 Mason type I fractures are generally treated conservatively and can be managed in the primary care setting. For these fractures, the elbow is placed in a posterior splint for five to seven days, followed by early mobilization and a sling for comfort. Aspiration of the effusion can be considered to provide pain relief and allow for earlier mobility. There is some evidence supporting the immediate initiation of elbow motion in patients with a Mason type I fracture. In one study, 60 patients with minimally displaced radial head fractures were randomized to immediate mobilization or a five-day delay before mobilization.20 There was no change in outcomes at four weeks or three months; however, patients with earlier mobilization had less pain and better function seven days after the injury. A randomized study of immediate mobilization with a sling for comfort compared with two weeks of casting revealed no benefit with casting.21
| Fracture type | Description |
|---|---|
| I | Nondisplaced fracture, no mechanical obstruction |
| II | Presence of significant displacement (greater than 2 mm) or angulation (greater than 30 degrees) |
| III | Comminuted fracture |
| IV | Fracture with associated elbow dislocation |
Imaging of Mason type I fractures should be repeated after one to two weeks to ensure appropriate alignment. Physical therapy may be added to encourage range of motion.22 More than 85 percent of patients with a Mason type I fracture have good results, with resolution of pain and a return to normal function in two to three months.23 Loss of motion, specifically the inability to fully extend the elbow, is the most common complication. Persistent pain or a delay in regaining elbow function indicates that repeat imaging or consultation with an orthopedist is necessary.
Mason type II fractures with only slight displacement may be managed without surgery. Significant displacement (greater than 2 mm) or angulation (greater than 30 degrees) requires surgery via excision or open reduction with internal fixation. Mason type III injuries may require fixation, excision, or replacement of the comminuted portion of the radial head.24 Orthopedic consultation is generally warranted for treatment of Mason type II through IV fractures.
OLECRANON FRACTURES
The subcutaneous position of the olecranon makes it vulnerable to fracture, especially when the elbow is flexed. The usual mechanism of injury is direct trauma. Injury may also occur as an avulsion at the site of the triceps tendon insertion. Associated swelling may be significant as the adjacent bursa sac fills with fluid. In the absence of an effusion, palpation of the fracture may be possible because of the absence of soft tissue structures. Therefore, a thorough inspection for open wounds is important. During the initial evaluation, the physician must ensure that the patient is able to extend the elbow. Any deficits of the extensor mechanism warrant orthopedic consultation. Because the fracture is generally well visualized on the lateral elbow radiograph, advanced imaging is rarely required.23
Olecranon fractures can be classified as intra-articular or extra-articular, depending on their radiographic appearance. Extra-articular fractures are less common (Figure 5) and are generally caused by a triceps avulsion injury. These can be managed nonsurgically if the extensor mechanism is intact.25 Many olecranon fractures have an intra-articular pattern of injury and are classified according to displacement, elbow stability, comminution, and the integrity of the extensor mechanism. The treatment of intra-articular olecranon fractures is somewhat controversial and generally requires orthopedic consultation. Surgical fixation may be necessary in more active patients. Patients with minimal displacement (less than 2 mm), normal elbow stability, lack of comminution, and an intact extensor mechanism can be considered for nonsurgical treatment.19,24

CORONOID PROCESS FRACTURES
Fractures of the coronoid process of the proximal ulna are rare. The coronoid process is a triangular projection on the anterior surface of the olecranon that acts as a buttress to prevent posterior displacement of the elbow. These fractures are best seen on lateral elbow radiographs (Figure 6), and are present in 10 to 15 percent of elbow dislocations.26 They are generally part of a spectrum of injuries associated with an elbow dislocation. Acute care should focus on reduction of the dislocation with attention to the upper extremity neurovascular status. The radial artery pulse should be examined with the arm at 90 degrees flexion. Orthopedic consultation is appropriate for any elbow dislocation or coronoid process fracture with significant displacement or instability. As an isolated injury, fractures with less than 5 mm of displacement and a stable elbow can be treated conservatively with a long arm splint with the elbow at 90 degrees flexion for one to three weeks. If repeat imaging shows no evidence of further displacement, range of motion activities can be initiated.
