Am Fam Physician. 2010;81(10):1219-1227
Author disclosure: Nothing to disclose.
Approximately 1.5 million Americans reside in nursing homes. A family physician often leads the interdisciplinary team that provides for the medical, functional, emotional, nutritional, social, and environmental needs of these patients. The treatment of nursing home residents is a dynamic process of ongoing assessment, transitions, and shifting care plans. The clinical assessment of nursing home residents focuses on cognition, mood, disability, skin integrity, and medication management. Advance care planning includes the development of realistic goals of care with the patient and family that go beyond living wills and do-not-resuscitate orders. The nursing home medical record and Minimum Data Set document the interdisciplinary findings and care plan. Transitions between different health care environments are facilitated by communication among health care professionals and detailed transfer documentation. Palliative care encompasses continuing reassessment of the goals of care; general supportive care (e.g., family, cultural, spiritual); and legal planning. Identifying and reporting resident abuse and neglect, and infection control practices are also essential in nursing home care.
Nursing home care is a complex, highly regulated, and dynamic process. The combination of chronic health conditions and increased need for assistance with activities of daily living leads to special medical, social, behavioral, and spiritual needs. The 2004 National Nursing Home Survey found that 1.5 million persons older than 65 years in the United States have spent time in a nursing home, and 51 percent of nursing home residents require assistance with all activities of daily living.1 The most common diseases in nursing home residents include mental disorders or those involving the circulatory or central nervous system. The number of Americans needing long-term care is expected to double by 2050.1
Nursing homes vary greatly in size and scope of services. They may provide short-stay care, posthospitalization rehabilitation for community-dwelling patients, and hospice care. More than 80 percent of nursing homes use community physicians to provide care, but they also may employ staff physicians or contract with physician groups.1 A 2008 survey by the American Academy of Family Physicians reported that the average family physician supervises 9.6 nursing home residents and conducts 2.3 nursing home visits per week.2
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Patients with advance directives are more likely to die in a nursing home with hospice care, require fewer resources, and are hospitalized less. | B | 9 |
| Communication among health care professionals is essential in the transitional care of nursing home residents, and policies should be developed that promote high-quality transitional care. | C | 11 |
| Annual influenza vaccination is recommended for all nursing home residents and staff. | C | 35 |
| Pneumococcal polysaccharide vaccine (Pneumovax) is recommended for all adults 65 years and older, with repeat vaccination in five years if immunocompromised. | C | 37 |
| Two-step tuberculosis testing is recommended for nursing home residents to prevent false-negative results, which often occur in older adults. | C | 38 |
Role of Attending Physician
The American Medical Directors Association provides a detailed list of the attending physician's supervisory and clinical responsibilities, which are based on regulatory requirements (Table 1).4 Conceptually, nursing home care begins with the recognition that the physician is visiting the patient's residence. The nursing home staff provides for the nutritional, medical, functional, recreational, spiritual, emotional, social, and environmental needs of the patient and implements interdisciplinary assessment and treatment plans.
| Administrative | |
| Meet documentation requirements as governed by the facility, and state and federal law | |
| Provide residents, caregivers, and facility staff contact information to respond to calls regarding care | |
| Provide on-call roster to facility staff | |
| Provide an informed and credentialed alternate physician(s) for cross-coverage | |
| General | |
| Assess residents' decision-making capacity, and develop advance directives | |
| Abide by facility policies, including infection control procedures | |
| Assist in care planning and coordination | |
| Become familiar with federal and state regulations | |
| Become involved with committees and medical staff issues | |
| Liaison with residents, families, caregivers, and facility staff | |
| Perform comprehensive assessment of the resident | |
| Practice preeminence of resident autonomy and self-determination, when possible | |
| Provide care that is based on medical necessity | |
| Resident care | |
| Care planning and coordination, transfers, discharges: | |
| Facilitate safe transfers between care environments (e.g., from nursing home to hospital) | |
| Implement interdisciplinary approach to care (e.g., cancer screening; health maintenance; immunizations; behavioral interventions; fall prevention; palliative and hospice care; polypharmacy; management of nutrition, hydration, pressure ulcers, and infections) | |
| Emergencies | |
| Develop evaluation and treatment plan for emergencies | |
| If an emergency occurs, review circumstances and possible causes, and formulate measures (if applicable) to prevent similar events | |
| Liaison with nursing home medical director* | |
| Liaison with consultant pharmacists, and review medications | |
| Supervise midlevel health care professionals | |
| Physician may delegate care to midlevel health care professionals if within their scope of practice; follow facility policy | |
| Some tasks must be performed by a physician | |
| Visitation intervals | |
| Admission visit: the physician should examine residents within 72 hours of initial nursing home admission, unless a documented physician examination occurred within the previous five days; this visit establishes the level of care | |
| Scheduled visits: the physician should visit the patient within 30 days of the initial examination, then once every 30 days for the first 90 days and at least once every 60 days thereafter | |
| Interim visits should occur for acute, emergency, or unusual medical/behavioral issues | |
Ideally, the initial medical history is obtained from the resident, and supplemented with information from family members and available medical records. The examination should include assessment of mood, cognition, hearing, vision, gait and balance, and skin integrity. A review of the resident's medical record and functional status (Minimum Data Set [MDS]) is useful at each visit to assess progress, stability, and deterioration in health. Specific review of vital signs (especially weight), functional status, and medications are also important at each visit. If a visit occurs after a hospitalization or hospital transfer, the care plan must be reevaluated.
Advance Care Planning
The general goal of nursing home care is to maximize resident autonomy, function, dignity, and comfort. Care discussions should be repeated and goals periodically reevaluated. Discussion topics should include end-of-life care, hospital transfers, palliative care measures, health promotion, and diagnostic testing. These preferences are then documented via advance directives, living wills, and do-not-resuscitate orders. A power of attorney for health care or surrogate can also be designated to make health care decisions if the resident loses the capacity to do so.
Some states have Physician Orders for Life-Sustaining Treatment Paradigm programs to document patients' end-of-life wishes. Residents with these orders are more likely to receive comfort measures and less likely to be transferred to acute care hospitals. However, these orders are not legally recognized in all states.5
Few residents have an advance directive at the time of admission to a nursing home6; however, the Patient Self-Determination Act requires that all residents be offered information about advance care planning.7 Several studies show that residents with advance directives are more likely to die in a nursing home with hospice care, are less likely to use a feeding tube or respirator in the last month of life,8 require fewer resources, and are hospitalized less.9 Although discussions of end-of-life preferences have increased, one study showed that 90 percent of residents had only one documented end-of-life care discussion.6
Minimum Data Set
The MDS is a comprehensive assessment of function and health of each resident.10 The assessment is performed at admission, quarterly, and at change of status. Essential domains of the MDS assessment are listed in Table 2.10 The MDS is a clinical and quality-improvement tool that can be used to develop and modify the care plan (e.g., evaluation and assessment of new-onset incontinence). MDS data from all nursing facilities are reported to the Centers for Medicare and Medicaid Services' Nursing Home Quality Initiative, which creates quality reports on a facility-to-facility basis.10
| Activity pursuit patterns |
| Cognitive patterns |
| Communication/hearing problems |
| Continence |
| Customary routines |
| Discharge potential and overall status |
| Disease/diagnoses |
| Health conditions |
| Identification, demographics, background information |
| Medications |
| Mood and behavioral patterns |
| Oral (dental and nutrition) |
| Physical functioning and structural problems |
| Psychosocial well-being |
| Skin condition |
| Special conditions |
| Vision patterns |
Health Care Transitions
Poor transitional care (i.e., to different facility locations or changing levels of care) can result in medical errors, duplication of services, inappropriate care, poor clinical outcomes, and resident dissatisfaction.11 Physicians who have been caring for a resident rarely directly and verbally communicate with the receiving physician during transfers across health care settings.11 However, communication among health care professionals is essential, and policies should be developed to ensure high-quality transitional care.11 Clearly written patient summary information is vital for a safe transfer to or from a nursing home. Figure 1A and Figure 1B is a universal patient summary form.12
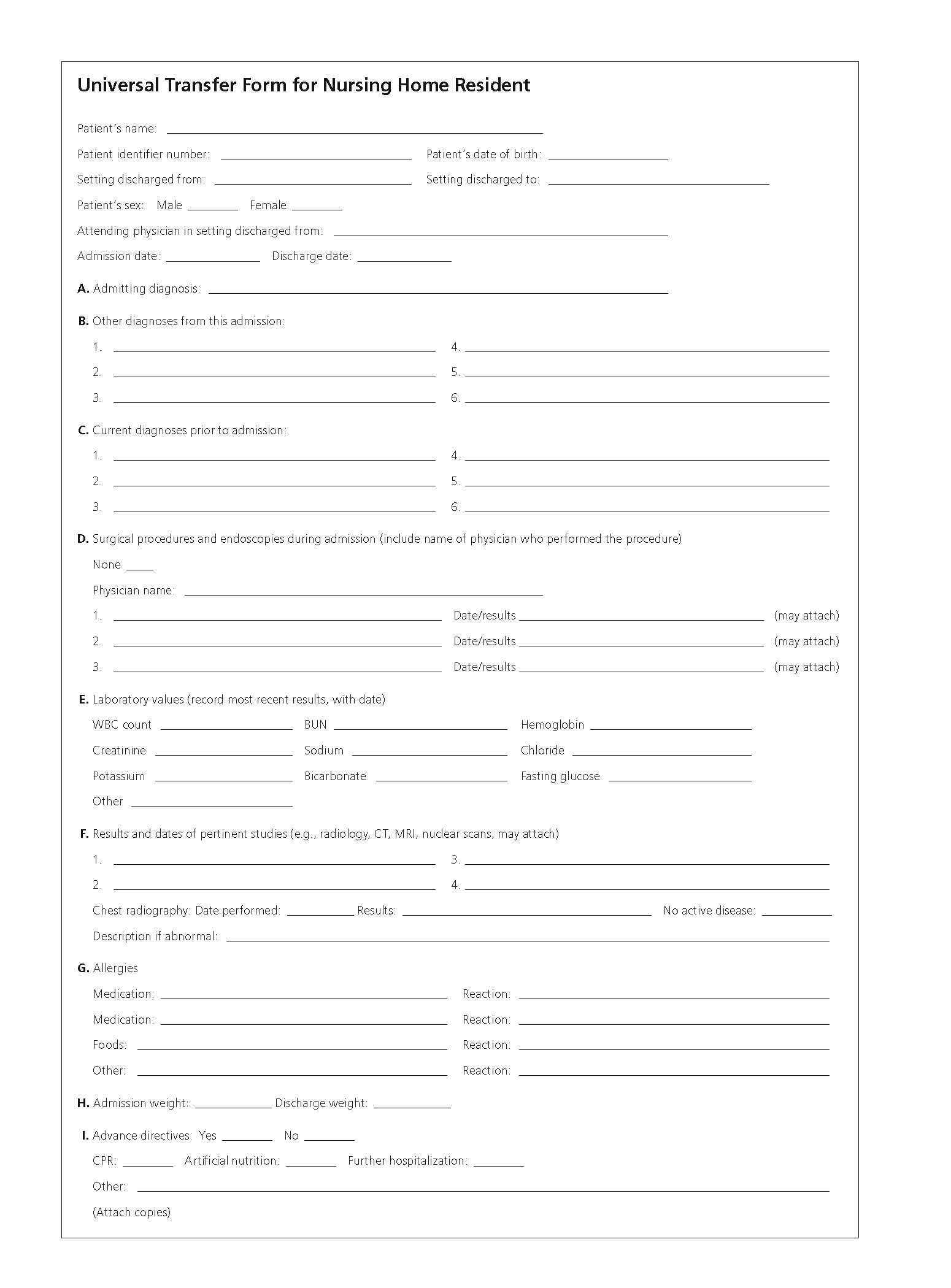
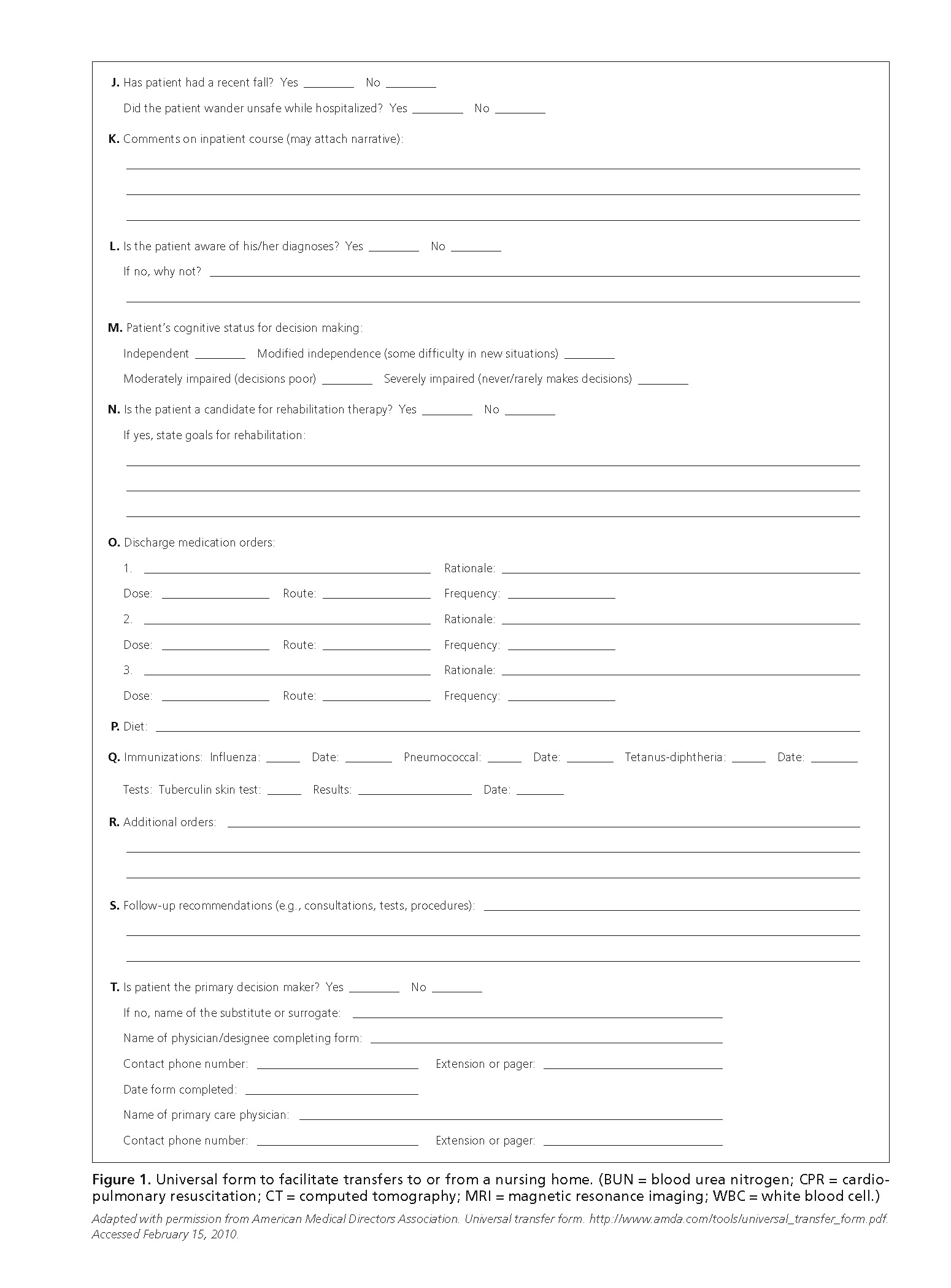
End-of-life care is particularly an issue when transferring nursing home residents to acute care hospitals for additional support and resources.13 Core components of an effective transfer include weighing the risks versus benefits of the transfer, matching the new care setting with the resident's needs, and ensuring communication between established and new physicians (e.g., common care plan; medical data and summary of previous care; resident goals, preferences, and advance directives; contact information of caregiver and primary care physician; resident preparation on what to expect; reconciliation of medication record with current regimen; pending follow-up plans).11
End-of-Life Care
Approximately one third of nursing home residents die within one year of admission; and it is estimated that by 2020, 40 percent of all deaths will occur in nursing homes.6 End-of-life care in the nursing home is similar to that in the community setting and includes prognosis, appropriate recognition of futility, pain management, hospice care, hospitalization, advance care planning, communication (among staff and between staff, the resident, and the resident's family), family perception of care, and staff education.14 A framework for palliative care involves establishing goals of care, providing progressive outside support and resources for the patient and family, and assisting with financial planning.15–17 This framework is summarized in Table 3.15–17 Nursing homes with hospice services have more residents with advance care plans, superior pain management programs, fewer hospitalizations, and improved care as perceived by staff and family members.6
| Element | Stage of disease or frailty | |||
|---|---|---|---|---|
| Early | Middle | Late | Bereavement | |
| Goals of care |
|
|
|
|
| Programmatic support |
|
|
|
|
| Financial and legal planning |
|
|
|
|
| Family support |
|
|
|
|
| Cultural support |
|
|
|
|
| Spiritual support |
|
|
|
|
Accurate prognostication of mortality is difficult until hours before death. However, patient communication, joint decision making, and determination of hospice eligibility is facilitated by knowledge of disease-specific clinical markers that are associated with terminal illness. General clinical markers predictive of mortality are listed in Table 4. A prognosis calculator has been developed for nursing home residents with advanced dementia.18 The Functional Assessment Staging tool for patients with Alzheimer disease19 and the Eastern Cooperative Oncology Group Performance Status scale20 have limited utility in predicting mortality, but are commonly used in determining hospice eligibility. Additional clinical resources are available on the American Academy of Hospice and Palliative Medicine Web site at http://www.aahpm.org.
| Acute illness |
| Anemia |
| Cognitive decline |
| Incontinence |
| Increase in falls |
| Leukopenia (total lymphocyte count < 800 per mm3 [0.8 × 109 per L]) |
| Long stay in nursing home |
| Mood decline |
| Need for assistance with activities of daily living |
| Nutritional decline |
| Personality change |
| Social withdrawal |
Alternatives to Nursing Home Care
In 2002, approximately 1 million persons lived in the 35,000 assisted-living facilities in the United States.21 Research suggests that persons with declining functional ability and health often move from the community setting to an assisted-living setting and then on to a nursing home.21 Assisted-living facilities have limited regulatory oversight and differ from nursing homes in residential environment, operational philosophy, and scope of services.22 Residents are contractually obligated to move to a different assisted-living facility if their health care needs exceed the services and capabilities of the current facility. The average length of stay in an assisted-living facility is two and one half to three years.23
Residents in assisted-living facilities are affected by many of the same complex conditions as nursing home residents, but the physician's role in the care of these residents is not defined. More than 80 percent of residents in assisted-living facilities need help with activities of daily living, 40 percent describe their health as fair or poor, and 23 to 42 percent have some form of measurable cognitive impairment.24 Knowledge of the facility's staffing and services is key to the treatment of these patients.24
Alternative living arrangements for older adults include subsidized senior housing, board and care homes, and continuing care retirement communities. Information about community-based services for older adults, such as transportation, meals, home care services, and care-giver resources, is available at http://www.eldercare.gov. Federal alternatives to nursing home care are available in some communities for Medicare patients, including the Program of All-Inclusive Care for the Elderly and the Social Managed Care Plan.25 The core feature of these two programs is provision of comprehensive medical and social resources that allow the resident to remain in the community as long as possible.
Abuse and Neglect in Nursing Homes
No reliable prevalence data exist for abuse and neglect of older persons in nursing homes. However, surveys of nursing home residents by facility staff and ombudsmen suggest that abuse and neglect are common. Alleged abuse complaints have been filed against one third of Medicare and Medicaid facilities.26 Staffing shortages and burnout are thought to be the primary causes of abuse in nursing homes, but programs and policies directed at improving staffing and training appear to be beneficial.26
The attending physician's role in identifying and preventing abuse and neglect in nursing homes begins with knowledge of facility and state regulatory procedures for reporting concerns (e.g., Adult Protective Services). Physicians are required to report abuse in most states, with the reporting physician immune to liability.27 Liaison with the nursing home administrators can identify problems and potential solutions. Multiple easy-to-use abuse screening tools are available, including the Elder Assessment Instrument, Brief Abuse Screen for the Elderly, and the Conflict Tactics Scale.28
Infection Control
The prevalence of methicillin-resistant Staphylococcus aureus (MRSA) in nursing homes ranges from 10 to 30 percent.30 Risk factors for MRSA colonization in nursing home residents include prior hospitalization, recent use of broad-spectrum antibiotics, impaired functional status, chronic diseases leading to skin breakdown, and use of medical devices such as urinary catheters and feeding tubes.31
MRSA infection is mainly transmitted from the health care worker to the patient. Other factors, such as environmental contamination and resident-to-resident contact, play little role in transmission.31 Routine infection control measures (Table 531–38 ) are necessary to prevent the introduction and spread of MRSA and other infections. Handwashing is the most important measure for controlling MRSA infection. Surveillance cultures and isolation are not usually necessary, because resident-to-resident contact is not a major mode of transmission. However, isolation is indicated for residents with MRSA infection who have wounds or need medical devices, such as tracheostomy tubes, that cannot be contained or covered.31
| Herpes zoster virus |
| No clinical practice guideline exists for herpes zoster immunization in nursing home residents. Immunization decisions should include an assessment of life expectancy, immune competency, burden of illness, and nutritional status.32 |
| The CDC recommends herpes zoster virus vaccine (Zostavax) for all adults 60 years and older without contraindications; booster is not necessary.33 |
| Influenza |
| Influenza vaccine should be administered to all staff and residents annually.34,35 |
| A meta-analysis demonstrated fewer influenza complications in nursing home residents, compared with community-dwelling older adults.36 |
| If an influenza outbreak occurs, treatment and chemoprophylaxis with antivirals should be initiated, and droplet precautions established. Cohorts of residents should be identified, and contact restricted among ill staff, residents, and visitors.35 |
| MRSA |
| All staff, visitors, and residents should use strict handwashing practices, and barrier precautions for wounds and medical devices should be initiated. |
| Surveillance cultures are not warranted. |
| Aggressive housekeeping practices play little, if any, role in prevention. |
| Cohorting and isolating residents are not practical or cost-effective.31 |
| Pneumococcal virus |
| Nursing homes are permitted to have standing orders to administer the pneumococcal polysaccharide vaccine (Pneumovax). |
| The CDC recommends the pneumococcal polysaccharide vaccine for all adults 65 years and older, with repeat vaccination in five years if immunocompromised.37 |
| Tuberculosis |
| Frail older adults residing in nursing homes have a greater risk of tuberculosis than those in the community setting. Two-step testing is recommended for nursing home residents to prevent false-negative results, which often occur in older adults.38 |
| All new residents and staff should receive a TST, unless a prior positive result is documented. Chest radiography and clinical diagnostic evaluation should be performed for those with a positive TST result. |
| Residents with known prior positive TST results who have normal findings on chest radiography or stable prior findings should be reevaluated periodically for change in symptoms. Repeat chest radiography is needed only if clinically indicated. |
| Residents with symptoms suggestive of tuberculosis, sputum smears positive for acid-fast bacilli, or radiography changes should be placed in airborne infection isolation. |
| When caring for residents with confirmed or suspected infectious pulmonary tuberculosis, staff must use respiratory protection devices approved by the National Institute for Occupational Safety and Health.38 |