Am Fam Physician. 2010;82(8):917-922
Patient information: See related handout on ACL injury, written by the authors of this article.
Author disclosure: Nothing to disclose.
There are an estimated 80,000 to 100,000 anterior cruciate ligament (ACL) repairs in the United States each year. Most ACL tears occur from noncontact injuries. Women experience ACL tears up to nine times more often than men. Evaluation of the ACL should be performed immediately after an injury if possible, but is often limited by swelling and pain. When performed properly, a complete knee examination is more than 80 percent sensitive for an ACL injury. The Lachman test is the most accurate test for detecting an ACL tear. Magnetic resonance imaging is the primary study used to diagnose ACL injury in the United States. It can also identify concomitant meniscal injury, collateral ligament tear, and bone contusions. Treatment consists of conservative management or surgical intervention, with the latter being the better option for patients who want to return to a high level of activity. Patients who undergo surgery must commit to appropriate rehabilitation for the best outcome. Long-term sequelae of ACL injury include knee osteoarthritis in up to 90 percent of patients. Primary prevention of ACL injury includes specific proprioceptive and neuromuscular training exercises to improve knee stability.
The knee joint is prone to injury because of its complexity and weight-bearing function. It is made up of the tibia, femur, and patella, which are stabilized by the medial collateral ligament, lateral collateral ligament, posterior cruciate ligament, and anterior cruciate ligament (ACL; Figure 11). The medial and lateral menisci act as shock absorbers, distributing weight evenly with each step or turn.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| The Lachman test is the most accurate test for detecting ACL injury, followed by the anterior drawer test and the pivot shift test. | C | 24 |
| Patients with ACL injury should be referred to an orthopedic surgeon if they have recurrent giving-way episodes, a strong desire to resume high-intensity activity, or concomitant meniscal or collateral ligament damage. | C | 23, 27 |
| A trial of conservative management may be considered if the patient has few giving-way episodes, near normal range of motion on knee extension, minimal or no meniscal damage on magnetic resonance imaging, strong quadriceps femoris, and no difficulty performing the crossover hop test. | C | 23, 27 |
| To prevent ACL injuries, athletes should participate in neuromuscular and proprioceptive strengthening and conditioning programs. These should include plyometric exercises and coaching regarding proper positioning while landing. | B | 8, 14, 33–36 |
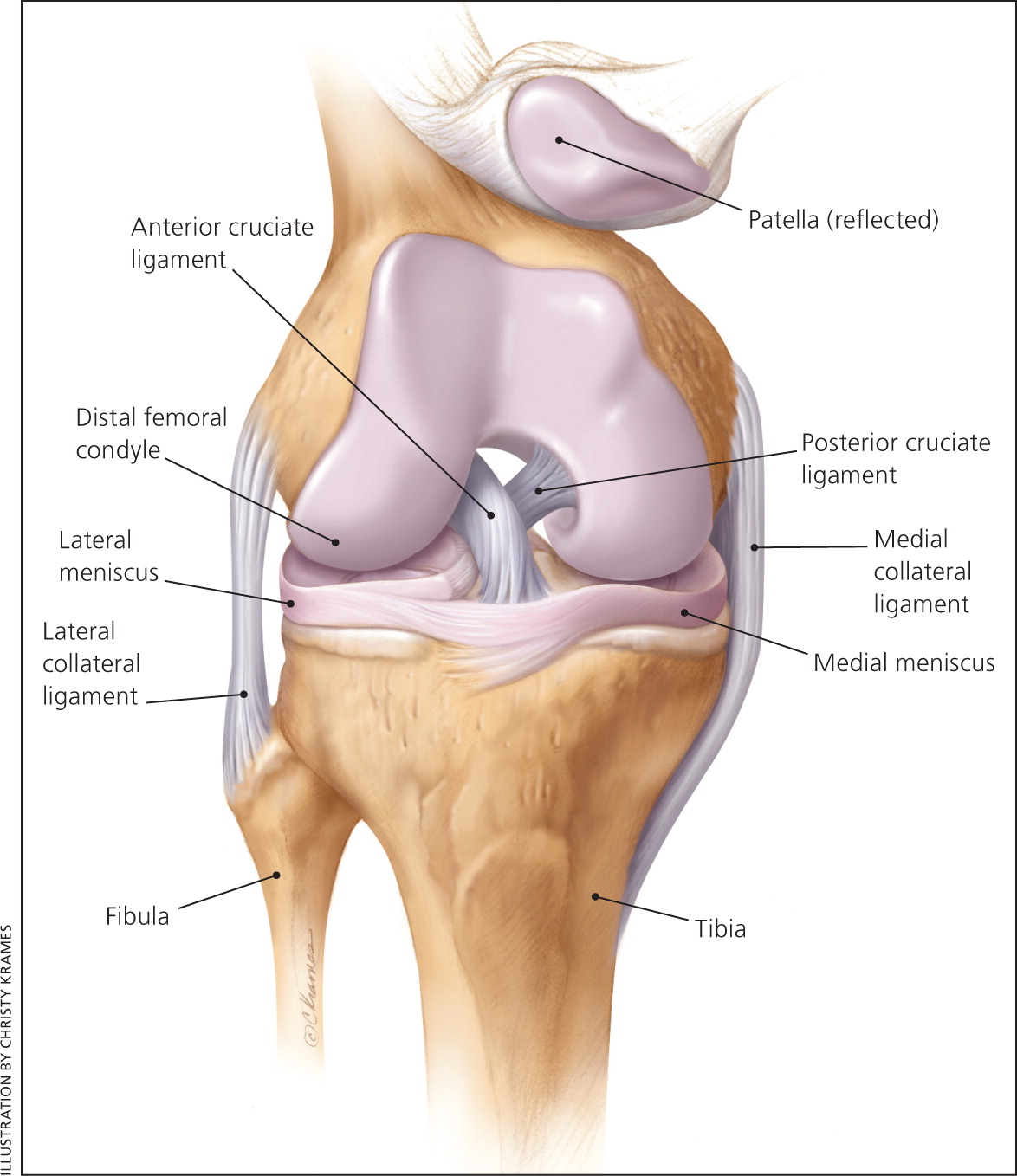
The ACL is the primary stabilizing structure of the knee. It originates from the posterior aspect of the femur coursing medially, inserting on the anterior aspect of the tibia. The ligament is intracapsular but is located outside the synovial fluid. The ACL is the primary restraint to anterior translation of the tibia, as well as tibial internal rotation.
Epidemiology
The overall incidence of ACL injury in the general U.S. population is not known, although one large New Zealand study found an incidence of 36.9 injuries per 100,000 person-years.2 Many estimates suggest there are 80,000 to 100,000 ACL repairs performed each year in the United States.3,4 ACL injuries generally occur beginning in late adolescence. Younger athletes usually sustain growth plate injuries (avulsion fractures) rather than ligamentous injuries because of the relative weakness of the cartilage at the epiphyseal plate compared with the ACL.5
Studies have shown a 1.4 to 9.5 times increased risk of ACL tear in women.6,7 Different theories for this predominance in women have been suggested, as well as other factors that could increase the likelihood of an ACL injury (Table 18–18). Studies also show that the intensity of play is a factor, with a three to five times greater risk of ACL injuries occuring during games compared with practices.19,20
| Extrinsic factors |
| Access to training facilities* |
| Ground/playing field (uneven field, wet or muddy conditions) |
| Level of competition (higher level) |
| Playing style (more aggressive) |
| Shoe surface (long cleats may provide too much traction) |
| Weather (rain, extreme cold) |
| Intrinsic factors |
| Body size and limb girth |
| Flexibility, strength, reaction time8 |
| Foot morphology |
| Hamstring strength*9 |
| Hormonal fluctuation* (suspicion of increased laxity at ovulatory and postovulatory phase)10 |
| Increased Q angle*† (greater than 14 degrees in men and greater than 17 degrees in women)11,12 |
| Leg dominance (differences in strength, flexibility, and coordination between right and left leg)11,13 |
| Ligament dominance (decreased medial-lateral neuromuscular control of the joint)14 |
| Ligamentous laxity15 |
| Narrow intercondylar notch on the distal femur (controversial whether this is more common in women)16 |
| Pelvic width* |
| Quadriceps dominance* (more quadriceps strength and decreased hamstring strength)17 |
| Small ACL size16,18 |
Mechanism of Injury
Patients who sustain ACL injuries classically describe a popping sound, followed by immediate pain and swelling of the knee. The feeling of instability or giving-way episodes typically limit the ability to participate in activities. Patients might describe the feeling of instability with the “double fist sign” (i.e., fists facing each other, rotating in a grinding motion).
ACL injuries caused by contact require a fixed lower leg (i.e., when planted) and torque with enough force to cause a tear. Contact injuries account for only about 30 percent of ACL injuries.11 The remaining 70 percent of ACL tears are noncontact injuries occurring primarily during deceleration of the lower extremity, with the quadriceps maximally contracted and the knee at or near full extension.21 In noncontact scenarios, the stress on the ACL resembles that of a collision of the knee. When the knee is at or near full extension, quadriceps contraction increases ACL tensile force. The hamstrings, which stabilize the ACL posteriorly, are often minimally contracted during these injuries, particularly if the hip is extended and the body weight is on the heel, allowing for excessive forward shifting of the femur on the tibia.12,21 Examples of this type of noncontact injury include skiers or snowboarders whose ankles are locked when they fall backward onto the snow; soccer players who execute sudden cutting maneuvers; or basketball players who land on an internally rotated knee without full flexion.3
Evaluation
Evaluation of the ACL should be performed immediately after an injury, if possible, but is often limited by swelling and pain. The evaluation should begin by observing the patient's gait, as well as the position of comfort he or she assumes on the examination table. The physician should note any asymmetry, including loss of the peripatellar groove indicating an effusion, hemarthrosis, or both. In a study of 132 athletes with acute knee injury and hemarthrosis, 77 percent had a partial or complete tear of the ACL.22
A more subtle effusion can be detected by compressing the medial and superior aspects of the knee, then tapping the lateral aspect to create a fluid wave. The physician can also attempt to palpate the patella with suprapatellar compression, which will feel spongy if effusion is present.
When hemarthrosis is present, the increased intraarticular volume produces considerable pain on range of motion. This pain results in extensive guarding and spasm of the hamstring muscle group, further limiting the knee's range of motion and making an accurate examination difficult. The patient may not be able to fully flex the knee, but the loss of hyperextension is more indicative of an ACL disruption. The torn ACL stump compressed between the tibia and femur, as well as the joint effusion, prevents full extension.23 Inability to achieve full extension also raises the possibility of a locked displaced meniscal tear.
If performed properly, a complete knee examination for ACL injury can be highly accurate, with a sensitivity and specificity of 82 and 94 percent, respectively.24 The likelihood ratio is 25.0 for a positive examination and 0.04 for a negative examination.24 The three most accurate tests for detecting an ACL tear are the Lachman test (sensitivity of 60 to 100 percent; mean 84 percent), the anterior drawer test (sensitivity of 9 to 93 percent; mean 62 percent), and the pivot shift test (sensitivity of 27 to 95 percent; mean 62 percent).24 See instructional videos of the Lachman test, the anterior drawer test, and the pivot shift test.
Lachman Test
Anterior Drawer Test
Pivot Shift Test
A radiographic knee series, including anterior-posterior, lateral, tunnel, and sunrise views, should be the initial imaging study to assess for fractures, evaluate knee alignment, determine skeletal maturity, and identify degenerative changes in middleaged patients. Magnetic resonance imaging (MRI) is the primary study used to diagnose ACL injury in the United States. It has the added benefit of identifying meniscal injury, collateral ligament tear, and bone contusions. Approximately 60 to 75 percent of ACL injuries are associated with meniscal tears, up to 46 percent have collateral ligament injuries, and 5 to 24 percent are associated with complete tear of a collateral ligament.25 The sensitivity and specificity of MRI for detecting an ACL tear is 86 and 95 percent, respectively, as confirmed on arthroscopy.26
When to Refer
If ACL injury is suspected on initial evaluation, it is reasonable to refer to physical therapy immediately to maintain range of motion and develop quadriceps strength. Knee immobilizers are unnecessary and crutches should be offered only for a limited time if the patient has considerable discomfort on ambulation.
The decision to refer to an orthopedic surgeon is largely dependent on the preferences and activity level of the patient. Younger, more active patients often choose surgical repair over conservative management. Any patient who plans to continue activities involving rapid acceleration and deceleration, cutting, and pivoting should be evaluated for surgery. Referral is also recommended in patients who have recurrent giving-way episodes or concomitant meniscal or collateral ligament damage.23,27
Patients who decide to have surgery must commit to undergo an extensive rehabilitation. Crutches are generally needed postoperatively, and most rehabilitation programs have a 10- to 12-week intensive schedule of strength-building activities.
A subset of ACL-deficient athletes are able to return to pre-injury activity levels without surgery.27 History and examination findings that suggest a possible trial of conservative management include few givingway episodes, near normal range of motion on knee extension, minimal or no meniscal damage on MRI, strong quadriceps femoris, and no difficulty performing the crossover hop test (see a video of the crossover hop test).23,27
Crossover Hop Test
The rates of success of conservative management of a known ACL tear vary widely. In one study, 72 patients treated with conservative management were followed for an average of 38 months.28 Only 31 percent had excellent or good results, and only 5.5 percent said they were performing equally as well in their sport as before the injury. In a second study, 30 percent of patients needed surgery after treatment with conservative management was unsuccessful; 86 percent continued to have giving-way episodes, but most did not report problems with chronic pain or swelling.29
A Cochrane review examining conservative versus surgical treatment of ACL tears found only two studies that met inclusion criteria.30 Both studies were from Sweden in the 1980s before the common use of MRI, and used now-outdated rehabilitation (plaster casts for conservative treatment) and surgical techniques. Neither study showed significant differences in return to sports activity.
A more recent randomized trial compared structured rehabilitation plus early ACL reconstruction to structured rehabilitation plus optional delayed ACL reconstruction in 121 adults between 18 and 35 years of age.31 At two years, the results showed no differences in pain, symptoms, sports function, or knee-related quality of life. Fewer than one half of participants in the optional delayed group chose to have ACL reconstruction after completing rehabilitation.
Primary Prevention
As the incidence of ACL injuries has increased, research on prevention has also increased. ACL injuries have been linked with chronic pain and osteoarthritis in 10 to 90 percent of patients 10 to 20 years after the injury.32
One study examined the use of a structured warm-up program in more than 1,800 athletes 15 to 17 years of age.33 The program included techniques to improve cutting and jumping movements, balance board exercises to focus on knee position during unstable movement, and strength exercises. The number needed to treat to prevent any acute knee injury over eight months was 43 patients.
Another study evaluated more than 5,000 female soccer players 14 to 18 years of age during two athletic seasons.8 The prospective nonrandomized trial used the Prevent Injury, Enhance Performance program, which is a well-known protocol for reducing ACL injuries (Table 2).8 Athletes in the intervention group experienced two ACL injuries compared with 32 ACL injuries in the control group, an 88 percent reduction. The results were reproduced the following year with a 75 percent reduction.
| Component | Details |
|---|---|
| Warm-up (50 yards each) | Jog line to line |
| Shuttle run (side to side) | |
| Backward running | |
| Stretching (30 seconds per stretch, two repetitions per stretch) | Calf stretch |
| Quadriceps stretch | |
| “Figure four” hamstring stretch | |
| Inner thigh stretch | |
| Hip flexor stretch | |
| Strengthening | Walking lunges (20 yards for two sets) |
| Russian hamstring (10 repetitions for three sets) | |
| Single toe raises (30 repetitions on each side) | |
| Plyometrics* (20 repetitions each) | Lateral hops over 2- to 6-inch cones |
| Forward/backward hops over 2- to 6-inch cones | |
| Single leg hops over 2- to 6-inch cones | |
| Vertical jumps with headers | |
| Scissors jump | |
| Agility | Shuttle run with forward/backward running (40 yards) |
| Diagonal runs (40 yards) | |
| Bounding run (50 yards) |
One aim of programs such as the Prevent Injury, Enhance Performance protocol is to diminish the effect of fatigue on neuromuscular control, which can lead to poor knee and hip positioning. Neuromuscular and proprioceptive training attempts to improve the reflexive response of the joint itself, because the voluntary muscle response is not usually quick enough to counteract the forces acting on the knee.
Sports-specific proprioceptive training has been implemented for a variety of sports, including basketball, skiing, and handball, with positive results in terms of ACL injury prevention.34–36 A meta-analysis of ACL-specific prevention protocols revealed that among successful programs, plyometrics (i.e., repetitive rapid loading and contraction of a targeted muscle group), strength training, and balance exercises combined with regular feedback about proper body positioning while landing make the greatest difference in ACL injury prevention.14