A more recent article on common types of supraventricular tachycardia is available.
Am Fam Physician. 2010;82(8):942-952
Patient information: See related handout on supraventricular tachycardia, written by the authors of this article.
Author disclosure: Nothing to disclose.
The most common types of supraventricular tachycardia are caused by a reentry phenomenon producing accelerated heart rates. Symptoms may include palpitations (including possible pulsations in the neck), chest pain, fatigue, lightheadedness or dizziness, and dyspnea. It is unusual for supraventricular tachycardia to be caused by structurally abnormal hearts. Diagnosis is often delayed because of the misdiagnosis of anxiety or panic disorder. Patient history is important in uncovering the diagnosis, whereas the physical examination may or may not be helpful. A Holter monitor or an event recorder is usually needed to capture the arrhythmia and confirm a diagnosis. Treatment consists of short-term or as-needed pharmacotherapy using calcium channel or beta blockers when vagal maneuvers fail to halt or slow the rhythm. In those who require long-term pharmacotherapy, atrioventricular nodal blocking agents or class Ic or III antiarrhythmics can be used; however, these agents should generally be managed by a cardiologist. Catheter ablation is an option in patients with persistent or recurrent supraventricular tachycardia who are unable to tolerate long-term pharmacologic treatment. If Wolff-Parkinson-White syndrome is present, expedient referral to a cardiologist is warranted because ablation is a potentially curative option.
Supraventricular tachycardia (SVT) is tachycardia having an electropathologic substrate arising above the bundle of His and causing heart rates exceeding 100 beats per minute. Accelerated rhythms can be frightening to the patient if recurrent or persistent, and can cause significant morbidity. This article focuses on the most common types of paroxysmal SVT: atrioventricular nodal reentrant tachycardia (AVNRT), atrioventricular reciprocating tachycardia (AVRT), and atrial tachycardia (AT). Although atrial fibrillation and flutter are classified as types of SVT, they will not be discussed in this article and are reviewed elsewhere.1,2 Table 1 lists the common types of SVT and usual characteristics.3–6 Figure 1 depicts AVNRT, AVRT, AT, and normal sinus rhythm.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Intravenous adenosine (Adenocard) or verapamil is a safe and effective treatment choice for terminating SVT, but verapamil is more effective for suppression of this rhythm over time. | B | 2, 14 |
| Vagal maneuvers are an effective first-line treatment option for SVT in younger patients who are hemodynamically stable; they can also be diagnostic for nodal-dependent SVT. | C | 2, 21 |
| Brugada criteria are sensitive and specific in helping distinguish between SVT with aberrancy and ventricular tachycardia. | C | 33 |
| Adenosine may be used as a diagnostic or therapeutic agent in patients with undifferentiated wide complex tachycardia. | C | 35 |
| Radiofrequency ablation is a safe, effective, and cost-effective method for suppressing SVT, and it improves patient quality of life compared with medical treatment of SVT. | B | 2, 41, 42 |
| Type | Epidemiology | Mechanism | Possible electrocardiography changes |
|---|---|---|---|
| AVNRT | Most common SVT (approximately 50 to60%)4 Occurs more often in younger women | Reentry caused by nodal pathways or tracts (two types): atypical (fast/slow) represents 10% and typical (slow/fast) represents 90% of all AVNRT | Rate: 118 to 264 bpm Rhythm: regular, narrow QRS complex (< 120 msec); regular, wide QRS complex (≥ 120 msec); may not see any P-wave activity in either type (atypical or typical) Atypical AVNRT: RP interval > PR interval; P waves negative in leads III and aVF Typical AVNRT: RP interval < PR interval; pseudo R wave in lead V1 with tachycardia, not with normal sinus rhythm; pseudo S wave in leads I, II, and aVF |
| AVRT | Second most common SVT (approximately 30%)4,5 Orthodromic most common type (81 to 87%) Occurs more often in younger women and children May be comorbid with Wolff-Parkinson-White syndrome | Reentry caused by accessory pathways (two types): orthodromic (antegrade conduction through atrioventricular node) and antidromic (retrograde conduction through atrioventricular node) | Rate: 124 to 256 bpm Rhythm: regular, narrow QRS complex common (orthodromic); regular, wide QRS complex uncommon (orthodromic or antidromic) if bundle branch block or aberrancy present Orthodromic AVRT: RP interval < PR interval or RP interval > PR interval with a slowly conducting accessory pathway; retrograde P waves (leads I, II, III, aVF, V1); delta wave seen with normal sinus rhythm, not with tachycardia Antidromic AVRT: short RP interval (< 100 msec); regular, wide QRS complex (≥ 120 msec); delta waves seen with normal sinus rhythm and tachycardia; concealed accessory pathways do not show delta waves |
| AT | Third most common SVT (approximately 10%)6 Two types: AT and multifocal AT AT has two forms: focal and macroreentrant Multifocal AT occurs more often in middle age or in persons with heart failure or chronic obstructive pulmonary disease | Reentry (micro), automaticity, or triggered activity: focal AT (reentry, automaticity, or triggered activity); multifocal AT (automaticity activity) | Rate: 100 to 250 bpm (atrial); ventricular varies Rhythm: regular, narrow QRS complex usually; irregular (ectopic foci) may have wide QRS complex if aberrancy present Focal AT: long RP interval most common; P-wave shape/polarity variable Multifocal AT: three different P-wave morphologies exist unrelated to each other; RR interval irregularly |
Epidemiology
SVTs (excluding atrial fibrillation or flutter and multifocal AT) have an estimated incidence of 35 per 100,000 person-years, with a prevalence of 2.29 per 1,000 persons.7 Although AVNRT is the most common SVT in adults (approximately 50 to 60 percent),4 AVRT is most common in children (accounts for approximately 30 percent of all SVTs).4,5
Pathophysiology
AVNRT and AVRT are electrical aberrancies that occur mainly as a result of reentry. Less commonly, increased automaticity or triggered activity can be the mechanism and usually results in a narrow complex tachycardia. AT can result from one of the three mechanisms (Table 1).3–6 AVNRT and AVRT are atrioventricular nodal-dependent arrhythmias, whereas AT is an atrioventricular nodal-independent arrhythmia.
AVNRT
The most common type of SVT is AVNRT. Most patients with AVNRT do not have structural heart disease; the group most often affected is young, healthy women.8 However, some patients do have underlying heart disease, such as pericarditis, previous myocardial infarction, or mitral valve prolapse.9 The coexistence of slow and fast pathways in atrioventricular nodal tissue is the basis of aberrant substrate for reentrant tachyarrhythmias.10
AVRT
The second most common type of SVT is AVRT. Patients with this arrhythmia typically present at a younger age than those with AVNRT. This SVT is caused by accessory pathways (or bypass tracts) that serve as aberrant conduits for impulses that pass from the sinoatrial node and travel in an antegrade or retrograde fashion through such tracts, establishing a reentry circuit.11 AVRT, occasionally comorbid with Wolff-Parkinson-White syndrome, is a diagnosis not to be missed because this rhythm may spontaneously develop into atrial fibrillation.12 Key electrocardiography (ECG) findings, such as a delta wave, are not always apparent because of the accessory pathway being concealed; therefore, special diagnostic testing may be needed.13
AT
The third most common type of SVT is AT (approximately 10 percent); it originates from a single atrial focus.6 This SVT, if focal, usually has a definitive localized origin, such as adjacent to the crista terminalis in the right atrium or the ostia of the pulmonary veins in the left atrium.14,15 Another form, multifocal AT, often occurs in patients with heart failure or chronic obstructive pulmonary disease.16
Patient Evaluation
HISTORY AND PHYSICAL EXAMINATION
Symptoms of SVT depend on a number of factors, including patient age, presence of comorbid heart and lung disease, and duration of SVT episodes. Table 2 lists symptoms associated with SVT. Patients may also be asymptomatic or minimally symptomatic, potentially delaying diagnosis.
| Common |
| Chest discomfort or pressure; dyspnea; fatigue; lightheadedness or dizziness; palpitations (including possible pulsations in the neck) |
| Uncommon |
| Chest pain (more severe than discomfort); diaphoresis; nausea; presyncope or syncope |
| Rare |
| Sudden death (may occur with Wolff-Parkinson-White syndrome) |
The history may reveal the likely etiology underlying the SVT (Table 3). Sinus tachycardia must be considered in the differential diagnosis. Episodic SVT may be misdiagnosed as anxiety or panic disorder,17 especially in patients with a psychiatric history, prolonging definitive diagnosis and treatment. Prolonged and persistent elevated heart rates produced by some types of SVT have been known to cause a type of cardiomyopathy; therefore, a high index of suspicion for the diagnosis is important.18
| Inquiry | Possible implication |
|---|---|
| At what age did the symptoms begin (time of onset)? | Symptoms since early childhood suggest supraventricular tachycardia |
| Did symptoms begin when patient was sedentary or active? | Coronary ischemia with activity may lead to ventricular problems |
| How did the symptoms begin (gradually or suddenly)? | Sinus tachycardia starts and stops gradually |
| What were the symptoms (e.g., syncope, presyncope, lightheadedness with rapid heart rate, dizziness, shortness of breath, palpitations)? | Any combination of these symptoms suggests supraventricular tachycardia, especially in patients with Wolff-Parkinson-White syndrome |
| How long did the symptoms last? | Supraventricular tachycardia starts and stops quickly (within seconds) |
| What were the potential triggers (e.g., caffeine, reduced sleep, increased stress)? | Increased sympathetic discharge may induce sinus tachycardia |
| Is there a cardiac history? | Symptoms or arrhythmias after myocardial infarction or ischemia suggest ventricular origin |
| Is there a family history of cardiac disease or sudden death? | Ischemia or any sudden death suggest supraventricular tachycardia |
| Has the patient had any cardiac procedures? | History of ischemic heart disease is consistent with ventricular issues |
The physical examination may or may not be helpful in determining a possible etiology for a patient's symptoms. Younger patients who are otherwise healthy usually have a normal examination, with tachycardia (if present on examination) being the only physical finding. Table 4 lists items to include in a focused examination and diagnostic workup.
| Evaluation | System or test | Possible finding | Significance |
|---|---|---|---|
| Focused physical examination | Cardiovascular | Murmur(s) | Valvular heart disease causing heart failure or tachycardia |
| Friction rub | Pericarditis resulting in tachycardia | ||
| Third heart sound | Heart failure causing tachycardia | ||
| Cannon waves | Possible atrioventricular nodal reentrant tachycardia or ventricular tachycardia | ||
| Respiratory | Crackle | Heart failure resulting in tachycardia | |
| Endocrine | Enlarged or tender thyroid gland | Hyperthyroidism or thyroiditis resulting in tachycardia | |
| In-office testing | Vitals | Hemodynamic instability or febrile illness | Incite tachyarrhythmia |
| Orthostatic blood pressure | Autonomic or dehydration issues | Induce tachyarrhythmia | |
| Electrocardiography | Preexcitation | Wolf-Parkinson-White syndrome | |
| Wide versus narrow QRS complex | Type of SVT versus ventricular tachycardia | ||
| Q waves | Ischemia leading to ventricular tachycardia | ||
| Other findings | Type of SVT (see Table 1) | ||
| Blood work | Complete blood count | Anemia or infection | All possibly induce or incite tachyarrhythmia |
| Thyroid-stimulating hormone | Suppression or hyperthyroidism | ||
| Basic metabolic panel | Electrolyte disturbance | ||
| B-type natriuretic peptide | Congestive heart failure | ||
| Cardiac enzymes | Myocardial infarction or ischemia | ||
| Diagnostics | Chest radiography | Cardiomegaly | Congestive heart failure or cardiomyopathy |
| Holter monitor or event recorder | Capture aberrant rhythm, frequency, duration | Type of tachyarrhythmia | |
| Graded exercise test | Preexcitation or aberrant rhythm | Type of tachyarrhythmia | |
| Echocardiography | Structural or valvular disease | Possible surgical intervention |
ECG
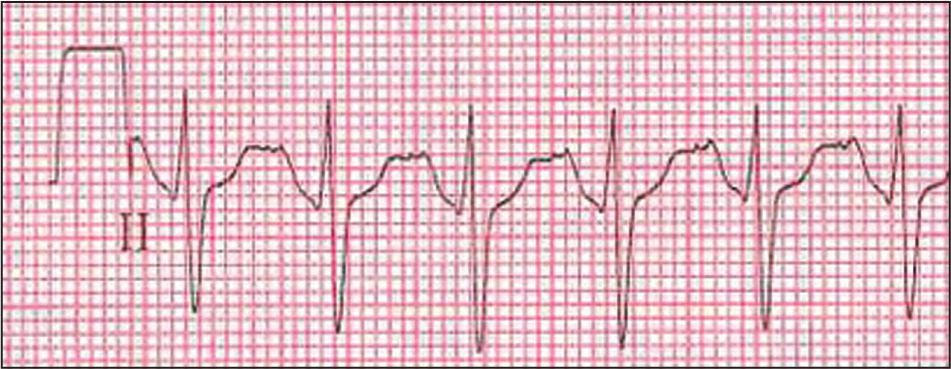
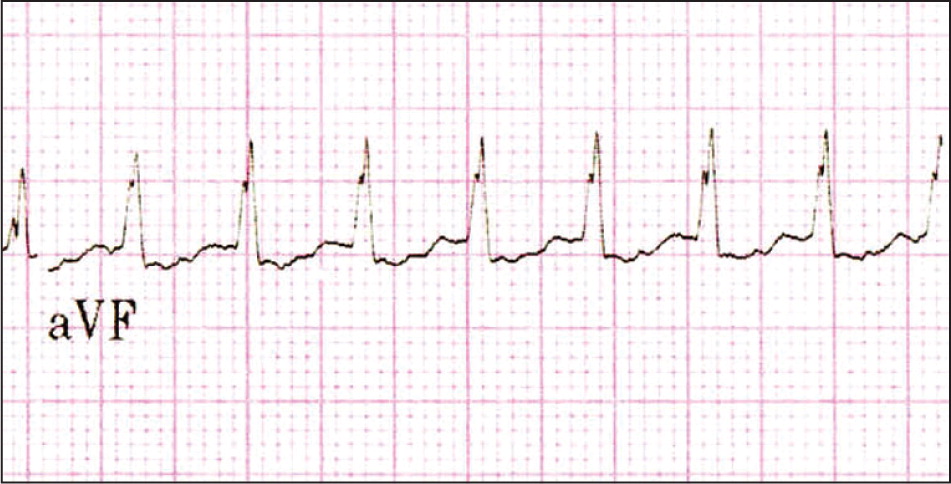
A 12-lead ECG should be performed in patients who are hemodynamically stable, with special attention to rhythm and rate, atrioventricular conduction (PR interval), RP interval, hypertrophy, pathologic Q waves, prolongation of the QT interval, and any evidence of preexcitation. Figures 2 through 5 are example ECGs for the types of SVT discussed. Most types of SVT have narrow QRS complexes. Wide complex tachyarrhythmias can also occur and can be secondary to SVT associated with bundle branch block, an accessory pathway, or ventricular tachycardia. In patients with a history of (or suspected) coronary artery disease or myocardial infarction, wide complex tachyarrhythmias must be considered to be of ventricular origin until proven otherwise and treated as such (see the treatment section). Table 1 describes ECG findings for common types of SVT.3–6


Further clinical investigations and their possible significance to SVT should be pursued (Table 4). Patients should be expediently referred to a cardiologist or electrophysiologist if they have experienced syncope or severe dyspnea, or if preexcitation is present on resting 12-lead ECG. Table 5 lists other situations in which patients should be referred to a cardiologist or electrophysiologist.
| Referral is warranted if: |
| Medications are not controlling symptoms |
| Patient cannot tolerate medications or no longer wishes to use them |
| Patient has worsening symptoms or is becoming hemodynamically unstable Patient is in a high-risk occupation (e.g., pilot, truck driver, heavy equipment operator) or participates in high-risk recreational activities (e.g., rock climbing, sky or scuba diving) |
| Physician is uncomfortable with or uncertain about management or initial diagnosis |
| Preexcitation is present on electrocardiography or if atrioventricular reciprocating tachycardia is suspected |
| Supraventricular tachycardia is accompanied by syncope |
| Wide QRS complex is present on electrocardiography |
Treatment
The primary treatment goal for any SVT is its cessation, especially in patients who are at risk hemodynamically and cannot tolerate prolonged tachyarrhythmias. SVT may be rare and fleeting in some patients, whereas in others, it is more frequent and may cause serious symptoms such as presyncope or syncope. Treatment of SVT can be divided into short-term or urgent management and long-term management.
SHORT-TERM OR URGENT MANAGEMENT
Short-term or urgent management of SVT can be separated into pharmacologic and nonpharmacologic strategies. Nonpharmacologic management typically uses maneuvers that increase vagal tone to decrease heart rate. Pharmacologic management typically includes intravenous adenosine (Adenocard) or verapamil, which are safe and effective treatment choices for terminating SVT, but verapamil is more effective for suppression of this rhythm over time.2,14 Figure 6 is an algorithm for the short-term management of SVT.19 Patients who are hemodynamically unstable need to be resuscitated with electrocardioversion to avoid further deterioration of cardiovascular status.
If the patient is hemodynamically stable, the QRS complex can provide information in decision making. A narrow QRS complex (less than 120 msec) usually indicates SVT, and the Valsalva maneuver is the most widely used and feasible treatment option in an alert patient. Although the use of this technique has been accepted in hospitalized settings, it has not been studied in the prehospital setting to determine its effectiveness.20 Vagal maneuvers are an effective first-line treatment option for SVT in younger patients who are hemodynamically stable; they can also be diagnostic for nodal-dependent SVT.2,21 Carotid massage can be used as a diagnostic and therapeutic tool; however, it should not be used in persons who may have atherosclerotic plaque that could be dislodged as a result of such a technique (i.e., history of carotid artery disease or carotid bruit).21
If these methods fail to terminate the SVT, or if the SVT soon returns, pharmacologic therapy is used. Table 6 shows recommended agents for short-term management of SVT.22 Which agent is selected after use of vagal maneuvers and adenosine depends on patient factors, such as contraindications (any comorbid conditions or allergies), hemodynamic stability, or presence of a wide QRS complex.
| Agent name | Class | Indication | Dosage | Comments |
|---|---|---|---|---|
| Short-term | ||||
| Adenosine (Adenocard) | V: endogenous purine nucleotide | Terminates SVT | 6 mg rapid intravenous push, repeat with 12 mg if needed | Can be diagnostic and therapeutic |
| Extremely short half-life | ||||
| Adverse effects include chest pain and dyspnea during administration | ||||
| Contraindicated in patients with Wolff-Parkinson-White syndrome | ||||
| Diltiazem | IV: calcium channel blocker | Decreases rate | 0.25 mg per kg intravenous bolus | Adverse effects include dizziness, heart failure exacerbation |
| Avoid in patients with Wolff-Parkinson-White syndrome or wide complex tachycardia | ||||
| Esmolol (Brevibloc) | II: beta blocker | Decreases rate | 500 mcg per kg intravenous loading dose | Can be proarrhythmic; has short half-life |
| Avoid in patients with renal disease; use with care in patients with asthma | ||||
| Verapamil | IV: calcium channel blocker | Decreases rate | 5 mg intravenously, up to 15 mg | Avoid in patients with congestive heart failure, Wolff-Parkinson-White syndrome, wide complex tachycardia, or atrioventricular block (second or third degree) |
| Long-term | ||||
| Amiodarone(Cordarone) | III: potassium channel blocker* | Prevents SVT | 200 to 400 mg orally once daily | Can result in optic neuritis, thyroid dysfunction, pulmonary fibrosis |
| Disopyramide (Norpace) | Ia: sodium channel blocker*† | Prevents SVT | 200 to 400 mg orally twice daily | Adverse effects include urinary retention |
| Metoprolol | II: beta blocker | Decreases rate | 25 to 100 mg orally twice daily | Atrioventricular node suppression possible |
| Procainamide | Ia: sodium channel blocker | Prevents SVT(long-term use) | 250 to 500 mg orally every six hours | Adverse effects include lupus, hypotension, His-Purkinje block |
| Quinidine | Ia: sodium channel blocker*† | Prevents SVT(long-term use) | 324 to 648 mg orally every eight to 12 hours | Avoid in patients with atrial fibrillation because of increased mortality |
| Closely monitor QTc interval when initiating therapy | ||||
| Verapamil | IV: calcium channel blocker | Prevents SVT | 80 to 240 mg orally three times daily | Adverse effects include constipation, dizziness |
| Avoid in patients with Wolff-Parkinson-White syndrome or wide complex tachycardia | ||||
Adenosine is an atrioventricular nodal blocking agent with a very short half-life (nine to 12 seconds). It is highly effective for the termination of nodal-dependent SVT and is the first-line drug for acute conversion of narrow complex SVT.23 Adenosine has the advantage of temporarily slowing the rate enough to determine the underlying focus of the rhythm (i.e., ventricular or supraventricular). Adenosine should not be used in persons with Wolff-Parkinson-White syndrome and atrial fibrillation because this rhythm can degenerate into ventricular fibrillation.24 There is poor evidence that medical therapy reduces sudden death in patients with Wolff-Parkinson-White syndrome; therefore, expedient referral for ablation is recommended in those patients who are symptomatic.2,25 Because AT is an atrioventricular nodal-independent SVT, atrioventricular nodal blocking agents, such as verapamil or adenosine, are mostly ineffective in its termination.26
Verapamil is a calcium channel blocker that may be used in patients with SVT that recurs after adenosine therapy. Verapamil, a negative inotrope, can result in relative bradycardia and vasodilation; care must be used if patients have a significant decrease in cardiac output.27 Neither digoxin nor a calcium channel blocker should be used in patients with Wolff-Parkinson-White syndrome or wide complex tachycardia, because these agents may enhance conduction down the accessory pathway, predisposing the patient to ventricular fibrillation.28 If the SVT persists, addition of a beta blocker will often result in its termination.29
In a review of eight trials involving 577 patients, there was no difference in the effectiveness of adenosine versus verapamil in successfully treating SVT. The overall termination rate was about 90 percent for both agents.30 If SVT is not terminated and the patient is hemodynamically stable, flecainide (Tambocor) or propafenone (Rythmol) may be used to terminate the SVT.31,32 These agents are almost always administered by a cardiologist.
Compared with narrow complex tachycardia, wide complex tachycardia presents infrequently, but does occur under certain conditions. Wide complex tachycardia is often difficult to distinguish from ventricular tachycardia, and all types should be treated as ventricular tachycardia when SVT cannot be discerned, particularly in patients who are hemodynamically unstable. If the patient is hemodynamically stable, use of the wellknown Brugada criteria (Table 7) can help distinguish between SVT with aberrancy and ventricular tachycardia, with a reported sensitivity as high as 98.7 percent and specificity as high as 96.5 percent.33 More recently, a newer simplified algorithm based on the Brugada criteria has been proposed. It may be more accurate in determining true ventricular tachycardia, with a reported overall test accuracy of 90.3 percent compared with 84.8 percent when all four Brugada criteria are used.34
| Electrocardiographic change | Criterion present | Criterion not present |
|---|---|---|
| 1. RS complex absent from all precordial leads | VT present; stop and treat | Proceed to 2 |
| 2. R S complex is present, and the longest precordial RS interval is > 100 msec in one or more precordial leads | VT present; stop and treat | Proceed to 3 |
| 3. Atrioventricular dissociation is present | VT present; stop and treat | Proceed to 4 |
| 4. Morphologic criteria for VT* present in precordial leads V1 to V2 and V6 | VT present; stop and treat | Supraventricular tachycardia with aberrant conduction is diagnosis made by exclusion |
A recent retrospective study showed that intravenous adenosine used in 197 patients with undifferentiated wide complex tachycardia was safe and effective for diagnostic and therapeutic purposes. No adverse effects occurred, and the likelihood of making a correct diagnosis of SVT or ventricular tachycardia increased.35
LONG-TERM MANAGEMENT
The long-term management of SVT is based on the SVT type; frequency and intensity of the episodes; overall impact on the quality of life of the patient; and risks of the therapy chosen.19 Discussion of these issues with the patient will help determine the optimal treatment strategy. The primary options include catheter ablation (radiofrequency versus cryotherapy) or pharmacologic treatment (Table 6).22 Figure 7 is an algorithm for the long-term management of SVT.19
Patients with infrequent SVT episodes may only need pharmacotherapy on an intermittent basis, or what has been described as the “pill-in-the-pocket” approach.36 Those experiencing SVT not more than a few times per year, but with episodes lasting one hour or longer, may be treated using this approach. This is typically done with verapamil (40 to 160 mg) in patients without preexcitation or a beta blocker in patients without chronic obstructive pulmonary disease or asthma. Agents used for long-term pharmacotherapy are similar to those used to terminate the SVT during short-term management. Atrioventricular nodal blocking agents (e.g., verapamil, diltiazem, beta blockers, digoxin) in AVNRT and AVRT with retrograde conduction are only about 30 to 60 percent effective.37 This relative lack of effectiveness can necessitate use of two such agents or the addition of class Ic or III antiarrhythmics. Larger trials comparing outcomes between these drug classes are not yet available (Table 822 ). Generally, these agents should be managed by a cardiologist.
| Class | Description |
|---|---|
| Ia | Reduce maximum velocity (rate of rise of action potential upstroke [phase 0]) |
| Prolong action potential duration | |
| Kinetics of onset and offset in blocking the sodium channel are of intermediate rapidity (less than five seconds) | |
| Examples include quinidine, procainamide, disopyramide (Norpace) | |
| Ib | Do not reduce maximum velocity |
| Shorten action potential duration | |
| Kinetics of onset and offset in blocking the sodium channel are rapid (less than 500 msec) | |
| Examples include mexiletine, phenytoin (Dilantin), lidocaine (Xylocaine) | |
| Ic | Can reduce maximum velocity |
| Primarily slow conduction | |
| Prolong refractoriness minimally | |
| Kinetics of onset and offset in blocking the sodium channel are slow (10 to 20 seconds) | |
| Examples include flecainide (Tambocor), propafenone (Rythmol) | |
| II | Block beta-adrenergic receptors |
| Examples include propranolol (Inderal), timolol, metoprolol | |
| III | Predominantly block potassium channels (e.g., inward rectifier potassium channels) |
| Prolong repolarization | |
| Examples include sotalol (Betapace), amiodarone (Cordarone) | |
| IV | Predominantly block the slow calcium channel (e.g., L-type calcium channel) |
| Examples include verapamil, diltiazem, nifedipine (Procardia), felodipine (blocks T-type calcium channel) | |
| V | Have various mechanisms of action |
| Examples include adenosine (Adenocard), digoxin, magnesium sulfate |
Ablative therapy of SVT is based on the observation that most arrhythmias arise from a focal origin critically dependent on conduction through a defined anatomic structure. If those critical regions are destroyed, the arrhythmia no longer occurs spontaneously or with provocation. Because of shorter procedure duration, lessened fluoroscopic exposure, and increased knowledge in this area of cardiology, catheter ablation is becoming the first-line treatment option for all patients with SVT, not just those with symptomatic arrhythmias refractory to suppressive drug therapy or those who prefer a drug-free lifestyle.
Clinical series of radiofrequency catheter ablation of accessory pathways have been published with excellent overall results.38 Experienced electrophysiology laboratories routinely achieve success rates of 95 percent in the ablation of accessory pathways, with recurrence rates of less than 5 percent.39 With improved knowledge of atrioventricular nodal anatomy and the advent of cryotherapy ablation, the current rate of symptomatic heart block is 0.5 to 1 percent.40
Because of its curative results and low percentages of severe adverse effects, and because the field is evolving so rapidly, there are few studies directly comparing catheter ablation with drug therapy in patients with SVT (with the exception of atrial fibrillation). However, observational studies have reported that patients undergoing radiofrequency ablation for SVT have better overall quality-of-life outcomes and lower costs attributed to therapy compared with medical treatment.41,42