
A more recent article on carpal tunnel syndrome is available.
Am Fam Physician. 2011;83(8):952-958
Related letter: Best Treatment Approaches for Carpal Tunnel Syndrome
Patient information: See related handout on carpal tunnel syndrome, written by the authors of this article.
Author disclosure: Nothing to disclose.
Carpal tunnel syndrome is the most common entrapment neuropathy, affecting approximately 3 to 6 percent of adults in the general population. Although the cause is not usually determined, it can include trauma, repetitive maneuvers, certain diseases, and pregnancy. Symptoms are related to compression of the median nerve, which results in pain, numbness, and tingling. Physical examination findings, such as hypalgesia, square wrist sign, and a classic or probable pattern on hand symptom diagram, are useful in making the diagnosis. Nerve conduction studies and electromyography can resolve diagnostic uncertainty and can be used to quantify and stratify disease severity. Treatment options are based on disease severity. Six weeks to three months of conservative treatment can be considered in patients with mild disease. Lifestyle modifications, including decreasing repetitive activity and using ergonomic devices, have been traditionally advocated, but have inconsistent evidence to support their effectiveness. Cock-up and neutral wrist splints and oral corticosteroids are considered first-line therapies, with local corticosteroid injections used for refractory symptoms. Nonsteroidal anti-inflammatory drugs, diuretics, and pyridoxine (vitamin B6) have been shown to be no more effective than placebo. Most conservative treatments provide short-term symptom relief, with little evidence supporting long-term benefits. Patients with moderate to severe disease should be considered for surgical evaluation. Open and endoscopic surgical approaches have similar five-year outcomes.
Carpal tunnel syndrome is the most common entrapment neuropathy, with a prevalence in the general adult population ranging from 2.7 to 5.8 percent.1,2 Although the prevalence of bilateral symptoms is uncertain, one study in the United Kingdom reported bilateral symptoms in more than 50 percent of cases.3 The mean annual crude incidence of carpal tunnel syndrome was found to be 329 cases per 100,000 person-years, and the standardized incidence was 276.4 Although the etiology is often unknown, certain conditions are commonly associated with carpal tunnel syndrome (Table 1). In addition, carpal tunnel syndrome is often associated with overuse-type injuries caused by repetitive motion, usually work-related.5 Because many other conditions produce symptoms similar to those of carpal tunnel syndrome (Table 2), an accurate history and physical examination are essential to establishing the diagnosis.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Flick sign, hypalgesia, square wrist sign, and a classic or probable pattern on hand symptom diagram are most discriminating for ruling in carpal tunnel syndrome. | C | 7, 9, 10 |
| Neutral and cock-up wrist splints produce short-term symptom relief in persons with carpal tunnel syndrome, with full-time use more effective than night-only use. | B | 19, 20 |
| Local and systemic corticosteroids yield significant resolution of symptoms in mild carpal tunnel syndrome for up to one month. | A | 21 |
| Repetitive maneuvers |
| Obesity |
| Pregnancy |
| Arthritis |
| Hypothyroidism |
| Diabetes mellitus |
| Trauma |
| Mass lesions |
| Amyloidosis |
| Sarcoidosis |
| Multiple myeloma |
| Leukemia |
| Condition | Characteristics |
|---|---|
| Carpometacarpal arthritis of thumb | Joint line pain, pain on motion, radiologic finding |
| Cervical radiculopathy (C6) | Neck pain, numbness in thumb and index finger only |
| Flexor carpi radialis tenosynovitis | Tenderness near base of thumb |
| Median nerve compression at elbow | Tenderness at the proximal forearm |
| Raynaud phenomenon | History of symptoms related to cold exposure |
| Ulnar or cubital tunnel syndrome | First dorsal interosseous weakness, fourth and fifth digit paresthesias |
| Vibration white finger | Uses vibrating hand tools at work |
| Volar radial ganglion | Mass near base of thumb, above wrist flexion crease |
| Wrist arthritis | Limited motion at wrist, radiologic finding |
Symptoms
The pain and paresthesias characterizing carpal tunnel syndrome are typically along the distribution of the median nerve (i.e., thumb, index finger, and middle finger; Figure 1). At times, these symptoms may occur in all the fingers, but should not occur in the dorsum or palm of the hand.

Pain and paresthesias may radiate proximally into the forearm, and even into the arm and shoulder. Patients may say that their fingers seem swollen and useless, but do not have swelling. They may also report loss of strength when gripping or performing certain tasks. The patient may be awakened with nighttime pain, with a history of shaking the hand or flicking the wrist in an attempt to alleviate the discomfort, which is known as the flick sign. The flick sign predicts electrodiagnostic abnormalities in 93 percent of cases and has a false-positive rate of less than 5 percent.6,7
The physician can also have the patient trace his or her hand on a piece of paper, or use a hand symptom diagram to identify patterns of symptoms that are consistent with carpal tunnel syndrome (Figure 28 ). The classic and probable patterns on a hand symptom diagram have 64 percent sensitivity for carpal tunnel syndrome. Only 9 percent of patients with an unlikely pattern have carpal tunnel syndrome (Table 3).7
| Finding | Sensitivity (%) | Specificity (%) | Positive likelihood ratio | Negative likelihood ratio |
|---|---|---|---|---|
| Flick sign | 93 | 96 | 21.4 | 0.1 |
| Hypalgesia | 39 | 88 | 3.1 | 0.7 |
| Square wrist sign | 53 | 80 | 2.7 | 0.6 |
| Classic or probable pattern on hand symptom diagram | 64 | 73 | 2.4 | 0.5 |
| Abduction weakness | 65 | 65 | 1.8 | 0.5 |
| Thenar atrophy | 16 | 90 | 1.6 | 0.94 |
| Tinel sign | 36 | 75 | 1.4 | 0.8 |
| Phalen maneuver | 57 | 58 | 1.3 | 0.7 |
| Nighttime or morning symptoms | 70 | 43 | 1.2 | 0.7 |
Information from reference 7.
Physical Examination
Ecchymosis or abrasions on the wrists and hands suggest an acute injury to the tissue, including the median nerve, as the etiology. Bony abnormalities, such as boutonniere deformity, swan neck deformity, and ulnar deviation of the wrist, suggest rheumatoid arthritis whereas carpal or distal phalanx bossing suggests osteoarthritis. Thenar atrophy usually occurs only with severe, chronic carpal tunnel syndrome, and is more commonly associated with other neuropathy syndromes and carpometacarpal arthritis7,9 (Table 37 ).
Patients should be evaluated for the presence of hypalgesia (diminished ability to perceive painful stimuli) along the palmar aspect of the index finger compared with the ipsilateral little finger of the affected hand. A two-point discrimination test, in which the inability to discriminate points less than 6 mm apart is considered abnormal, can be performed with a caliper. The abductor pollicis brevis may display notable weakness on strength testing. The physician can observe this weakness by instructing the patient to raise his or her thumb perpendicular to the palm as the physician applies downward pressure on the distal phalanx, resisting thumb abduction.7
Phalen maneuver and Tinel sign have been used to observe for reproduction of the patient's symptoms when the wrist is placed in flexion or when it is percussed on the volar surface, respectively. However, Phalen maneuver, Tinel sign, presence of thenar atrophy, and history of nocturnal paresthesias have little diagnostic value compared with other history and examination findings7,10 (Table 37 ).
Adjunctive Tests
The diagnosis of carpal tunnel syndrome is primarily based on history and physical examination findings. Adjunctive tests are useful when the diagnosis is uncertain. Electrodiagnostic testing is indicated for selected patients, whereas ultrasonography, magnetic resonance imaging, and computed tomography generally are not helpful.11
Nerve conduction studies and electromyography can be used for confirmation of diagnosis in patients with an intermediate pretest probability or with an atypical presentation. Nerve conduction studies and electromyography can also be used to quantify and stratify disease severity, which may aid in treatment decisions.12 A slowed median nerve conduction velocity supports the diagnosis. Nerve conduction studies have a sensitivity of 56 to 85 percent and a specificity of at least 94 percent for carpal tunnel syndrome.12,13 Electromyography is often paired with nerve conduction studies to differentiate primary muscle conditions from muscle weakness caused by neurologic disorders. In patients with a high probability of carpal tunnel syndrome based on history and physical examination, nerve conduction studies and electromyography generally are not indicated.12
Treatment
Management of carpal tunnel syndrome should be based on severity. Patients with mild to moderate carpal tunnel syndrome have normal to mildly abnormal nerve conduction study and electromyography findings. Severe disease is suggested by worsening clinical symptoms and clearly abnormal electrodiagnostic studies (Table 4). Six weeks to three months of conservative treatment is reasonable in patients with mild disease.14 Cock-up and neutral wrist splints and oral corticosteroids are considered first-line therapies, with local corticosteroid injections used for refractory symptoms. Patients with moderate to severe disease, or those with persistent symptoms despite conservative treatment, may be referred for surgical evaluation.15
| Classification | Duration | Two-point discrimination test | Weakness | Atrophy | Electromyography* | Nerve conduction studies* |
|---|---|---|---|---|---|---|
| Mild | Shorter than one year | Normal | Absent | Absent | No denervation | No to mild velocity decrease |
| Moderate | Shorter or longer than one year | Possible abnormality | Minimal presence | Minimal presence | No to mild denervation | No to mild velocity decrease |
| Severe | Longer than one year | Marked abnormality | Marked presence | Marked presence | Marked denervation | Marked velocity decrease |
CONSERVATIVE MANAGEMENT
Lifestyle Modification. Avoiding repetitive motions, using ergonomic equipment (e.g., wrist rest, mouse pad), taking breaks, using keyboard alternatives (e.g., digital pen, voice recognition and dictation software), and alternating job functions have traditionally been advocated for management of carpal tunnel syndrome. However, there is inconsistent evidence to support or refute the effectiveness of any of these interventions.
Oral Medication. Oral corticosteroids produce significant short-term symptom relief, with benefits waning over a period of eight weeks after medication is discontinued. In contrast, nonsteroidal anti-inflammatory drugs, diuretics, and pyridoxine (vitamin B6) have been shown to be no more effective than placebo.15–17
Splinting. There is good evidence supporting the use of neutral (Figure 318 ) and cock-up wrist splints, with similar symptom relief outcomes with both styles. There is limited evidence supporting the utility of a splint that fixates the metacarpophalangeal joints with the wrist, thus decreasing lumbrical migration into the retinacular space.19 There is good evidence supporting the use of splints 24 hours a day (full-time) over night-only use.20

Although there is little evidence concerning recommended splinting duration, most studies have been done with six to eight weeks of trial treatment, and effectiveness has been seen out to one year. In one study, splinting led to a decrease in symptoms that delayed patients' perceived need for surgery for at least one year in up to 60 percent of a population already considered surgical candidates based on symptoms and nerve conduction studies.20 Little evidence has shown long-term benefits after splinting cessation, and progression of disease may occur during the period of splint use.14
Corticosteroid Injection. Local corticosteroid injection may be used as an initial treatment or as an adjunctive subsequent therapy. There is strong evidence that local and systemic corticosteroids yield significant resolution of symptoms in patients with mild carpal tunnel syndrome for up to one month after the injection, with many patients reporting relief for up to one year. One study showed that local corticosteroids offer greater symptom relief than oral corticosteroids for up to three months, but provide similar symptom relief compared with a combination of nonsteroidal anti-inflammatory drugs and splinting at eight weeks.21 Although effectiveness is primarily short-term, corticosteroid injection may be particularly useful for patients wanting to delay surgical treatment.
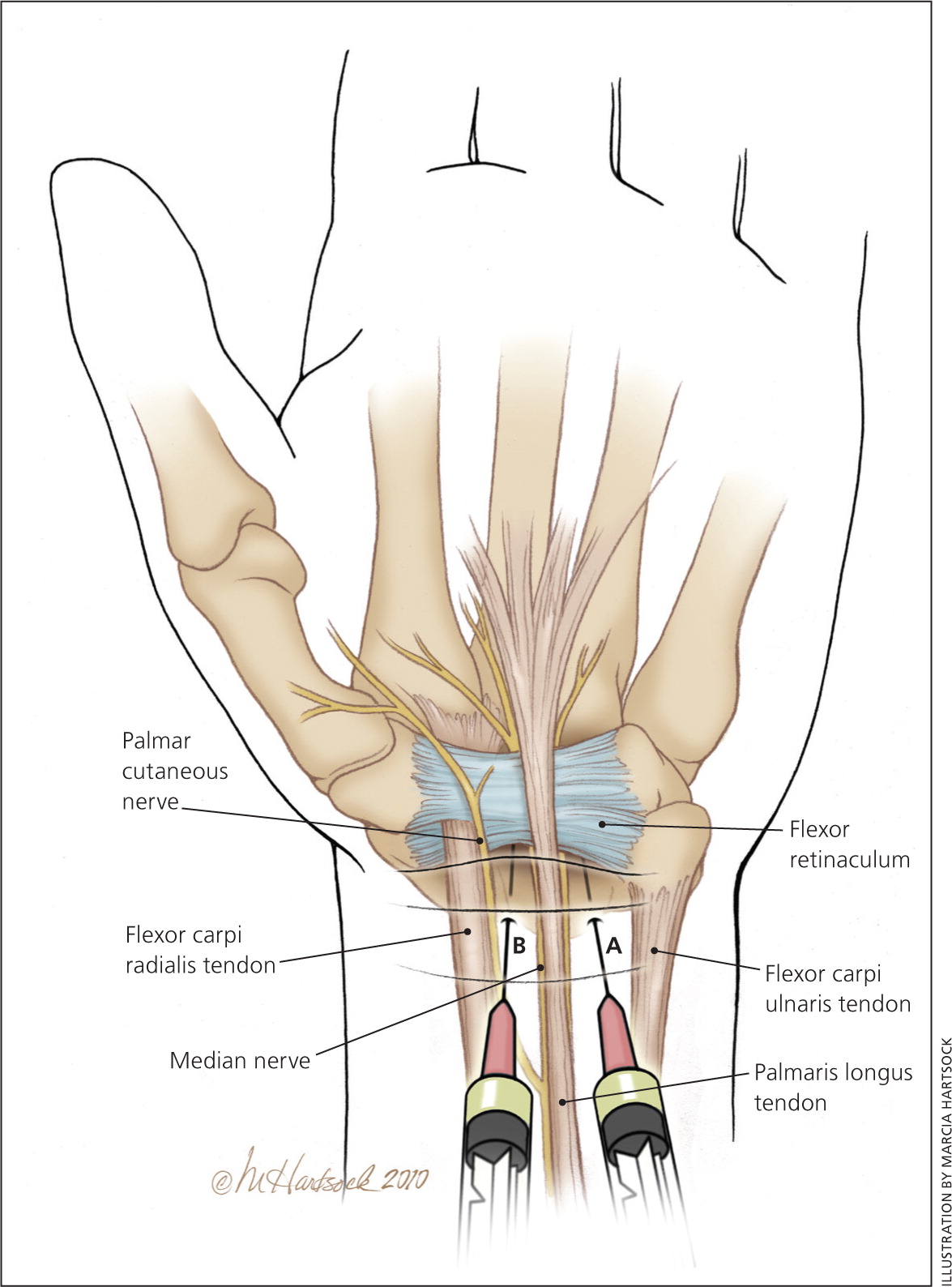
The procedure involves placing a small bolus of corticosteroid beneath the flexor retinaculum and within the carpal tunnel. A correlation between corticosteroid dose and symptom reduction has not been observed, and there are no good data supporting a specific type of corticosteroid formulation over another.22 Traditionally, 20 mg of triamcinolone acetonide (Kenalog) without lidocaine (Xylocaine) is injected using a 1-mL syringe with a 25-gauge, 1.25-inch needle.23 Median nerve injection injury is the major potential complication of these injections.
The median nerve lies immediately under the palmaris longus tendon, at the midpoint of the wrist and medial to the flexor carpi radialis tendon.23 If the patient does not have an identifiable palmaris longus tendon, have the patient touch the tip of his or her fifth digit to the thumb. The medial crease that is made is closely in line with the median nerve. The traditional method has been to inject just medial to the palmaris longus tendon or midway between the palmaris longus and the flexor carpi ulnaris tendons (Figure 4A; Table 5). An alternative method is to inject lateral to the palmaris longus tendon or between the palmaris longus and the flexor carpi radialis tendons (Figure 4B). A study concluded that this alternative method resulted in a greater distance between the needle and the median nerve, but had an increased risk of needle contact with the palmar cutaneous branch of the median nerve.24
| Place patient in a seated or supine position, with forearm in supination and wrist slightly extended |
| Identify point medial to the palmaris longus tendon or midway between the palmaris longus and flexor carpi ulnaris tendons |
| Insert a 25-gauge needle 1 cm proximal to the most distal wrist crease |
| Direct the needle in a 45-degree angle; slide distally until needle end lies under midpoint of the retinaculum |
| Give as a slow bolus injection; if patient has pain or paresthesias, stop the injection and redirect the needle medially |
| Advise patient to actively move his or her fingers for several minutes to allow even distribution of the solution |
SURGICAL MANAGEMENT
Five-year outcomes regarding carpal tunnel syndrome symptom relief have been shown to be equivalent using open or endoscopic surgical techniques.25 Surgical treatment of carpal tunnel syndrome relieves symptoms significantly more than splinting, but not necessarily more than corticosteroid injection.26 On average, postsurgical patients were able to return to driving in nine days, to activities of daily living in 13 days, and to work in 17 days, with a satisfaction rate of more than 90 percent.27
