
Am Fam Physician. 2012;85(3):247-252
Related editorial: Reassessing the Role of MRI in the Evaluation of Knee Pain
Author disclosure: No relevant financial affiliations to disclose.
Although historical findings have some value in diagnosing internal derangement of the knee, a thorough physical examination can often rule out fracture and ligamentous and meniscal injuries. The Ottawa Knee Rule can help physicians determine which patients require radiography. Positive physical examination tests and findings of acute effusion suggest internal derangement. An abnormal McMurray or Thessaly test strongly suggests meniscal injury, whereas a normal Thessaly test may rule out meniscal injury. Absence of evidence of joint effusion significantly decreases the probability of internal derangement. Magnetic resonance imaging should be reserved for ruling out internal derangement in patients with suggestive historical and physical examination findings.
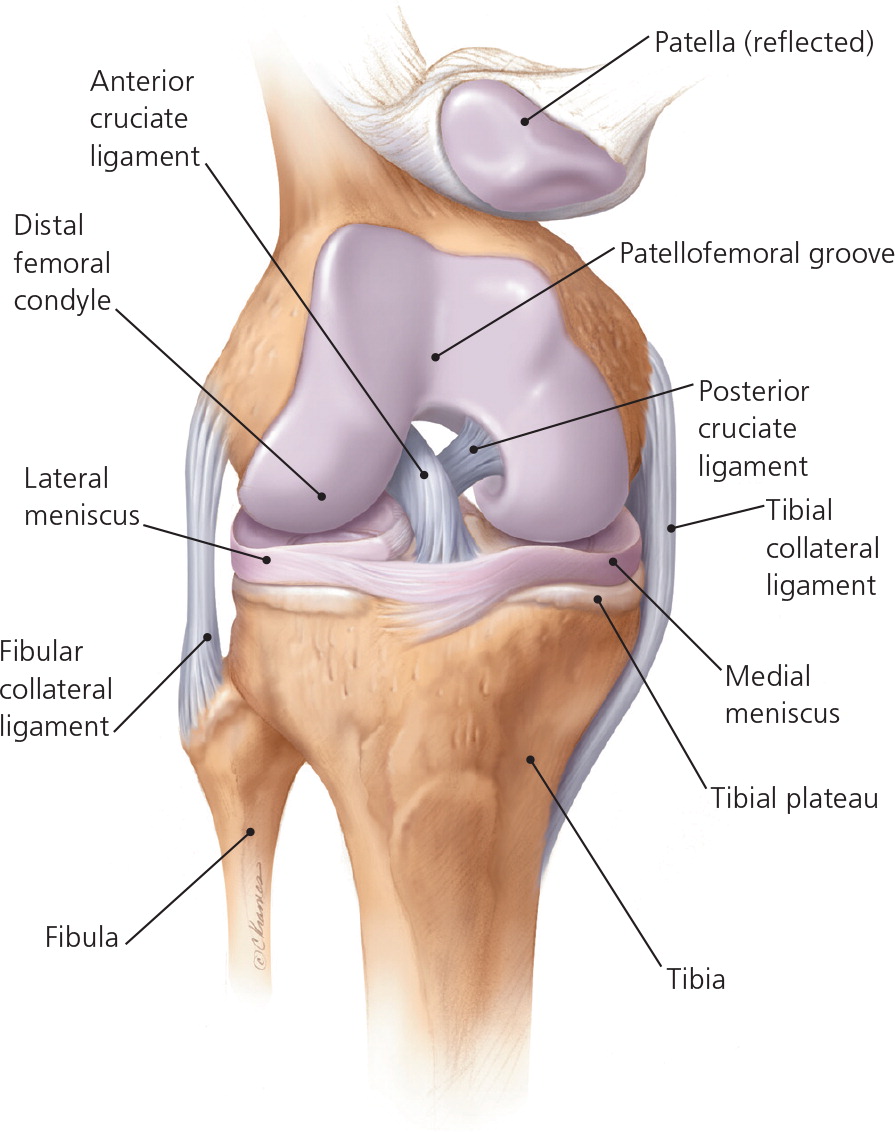
Nearly one-half of adults will experience knee pain at some point in their lives.1 Primary care physicians in the United States evaluate knee pain during approximately 4 million office visits each year, and knee symptoms are the 10th most common reason for outpatient visits.2 Although most episodes of knee pain in primary care patients are caused by osteoarthritis, many patients have acute injuries. Approximately 9 to 10 percent of patients with acute knee pain who are treated by family physicians have meniscal tears, 7 percent have collateral ligament injury, and about 4 percent have a cruciate ligament injury 2,3 (Figure 14 ).
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| The Ottawa Knee Rule should be used to determine which patients with acute knee injury require radiography. | A | 5, 6, 8–11 |
| Further testing is not immediately needed in patients with knee injury who have negative physical examination findings, although close clinical follow-up is required. | C | 3, 20, 23 |
| In patients with suspected meniscal injury, the Thessaly test is preferred over the McMurray test and evaluation for joint line tenderness. | C | 15, 27 |
| Internal derangement should be suspected in patients with knee trauma and effusion. | C | 16, 28 |
Because approximately one-third of patients with knee pain seek care from their primary care physician,1 it is important to be aware of the signs and symptoms associated with internal derangement of the knee (i.e., fracture, ligamentous injury, or meniscal tear). The primary role of the family physician in early evaluation of knee injury is to identify patients in need of referral for possible surgical intervention. If internal derangement and other acute external knee injuries (e.g., patellar subluxation, patellar tendon rupture) can be ruled out, the patient can be reassured that symptoms will likely resolve with conservative treatment (i.e., rest, ice, compression, elevation, and pain control).
Fracture
ILLUSTRATIVE CASE
A 52-year-old woman presents to the emergency department for evaluation of knee pain that began after a car crash. Her right knee struck the dashboard during a head-on collision. She was not able to walk immediately after the crash. Examination reveals a large effusion. The patient is not able flex the knee to 90 degrees, and she cannot bear weight on the leg. Radiography reveals a depressed tibial plateau fracture.
It is essential to accurately diagnose knee fractures while simultaneously using resources judiciously. Knee radiography is the most common imaging modality performed for trauma in the emergency department setting, but it has the lowest yield for diagnosing clinically significant fractures.5
The Ottawa Knee Rule can guide appropriate use of radiography at the point of care based on easily obtainable clinical information6 (Table 15–7 ). It has been repeatedly validated8–11 and decreases radiography utilization by 28 to 35 percent.9,10 The rule is 98.5 to 100 percent sensitive (i.e., it will detect almost all patients with fracture), and it has a specificity of 49 percent.9 If the prevalence (pretest probability) of fracture is 11 percent in the emergency department setting, the likelihood of fracture in a patient with any of the Ottawa Knee Rule criteria is approximately 20 percent, whereas in those with none of the Ottawa criteria, fracture can be ruled out based on clinical findings alone (approximately 1 percent chance of fracture).9 In the outpatient primary care setting, where the prevalence of fracture is only 2 percent, the probability of fracture in patients with a negative Ottawa Knee Rule evaluation is extremely low.
| Indication | American College of Radiology criteria5 | Ottawa Knee Rule6 | Pittsburgh Knee Rule7 |
|---|---|---|---|
| Age < 12 years or > 50 years | X | ||
| Age ≥ 55 years | X | ||
| Altered mental status | X | ||
| Fall or blunt trauma | X | ||
| Inability to bear weight for four steps (unable to transfer weight twice) immediately after injury or in the emergency setting | X | X | X |
| Inability to flex knee to 90 degrees | X | X | |
| Joint effusion within 24 hours of a direct blow or fall | X | ||
| Tenderness over head of fibula or isolated to patella without other bony tenderness | X | X |
The American College of Radiology has published recommendations for use of knee radiography in patients who have acute knee trauma.5 Although the recommendations have not been prospectively validated, they are similar to the Ottawa Knee Rule criteria. They recommend against radiography in patients (excluding infants) who can walk without a limp or who have a twisting injury and no effusion. The Pittsburgh Knee Rule criteria include blunt trauma or fall as the mechanism of injury, age younger than 12 years or older than 50 years, and inability to walk as independent predictors of fracture.7 A prospective validation trial comparing the Ottawa and Pittsburgh criteria showed that each rule is sensitive (97 to 100 percent of fractures found), but that the Pittsburgh rule is more specific (60 versus 27 percent for the Ottawa rule).12
Ligamentous Injury
ILLUSTRATIVE CASE
An 18-year-old high school basketball player presents the morning after sustaining a left knee injury during a game. An opposing player fell while rebounding the ball, striking the anterior aspect of the patient's tibia and forcing the femur to slide posteriorly on the tibia. The patient reports that he heard a pop, and that the knee immediately became swollen. He was unable to bear weight after the injury and is not able to take four steps in your office. Knee radiography is negative for fracture. Anterior drawer and Lachman tests are positive; the patient cannot tolerate a pivot shift test. Arthrocentesis reveals a large hemarthrosis.
No systematic review has addressed the diagnostic accuracy of physical examination findings in patients with collateral ligament injuries.3,13 Tenderness along the course of the ligament with reproduction of pain with valgus or varus force may be helpful. Visual inspection for differences in appearance between symptomatic and asymptomatic knees may also be revealing.
Historically, patients with ligamentous injury often have forceful stresses applied to the joint while bearing weight. They may hear or feel a popping sensation, and often note immediate swelling. Anterior cruciate ligament (ACL) injury accounts for more than 70 percent of acute hemarthroses in young athletes.14
The Lachman, anterior drawer, and pivot shift tests are common maneuvers used to examine the knee for internal derangement from ligamentous injury (Table 23,15,16 and Table 33,15–17 ). The acute swelling that can accompany injuries may make the initial physical examination difficult, so repeated examination may be necessary. The pivot shift test has a greater positive predictive value (i.e., a positive test is helpful for ruling in injury), whereas the Lachman test has a better negative predictive value (i.e., a negative test is helpful for ruling out injury).3
| Test | Description | Video link |
|---|---|---|
| Anterior cruciate ligament tear | ||
| Anterior drawer test3 | With the patient supine on the examining table, flex the hip to 45 degrees and the knee to 90 degrees. Sit on the dorsum of the foot, wrap hands around the hamstrings (ensuring that these muscles are relaxed), then pull and push the proximal part of the leg, testing the movement of the tibia on the femur. Do these maneuvers in three positions of tibial rotation: neutral, 30 degrees externally rotated, and 30 degrees internally rotated. A normal test result is no more than 6 to 8 mm of laxity. | https://www.aafp.org/online/en/home/publications/journals/afp/afp-oct-15-videos.html |
| Lachman test3 | With the patient supine on the examining table and the leg at the examiner's side, slightly externally rotated and flexed (20 to 30 degrees), stabilize the femur with one hand and apply pressure to the back of the knee with the other hand, with the thumb on the joint line. A positive test result is movement of the knee with a soft or mushy end point. | https://www.aafp.org/online/en/home/publications/journals/afp/afp-oct-15-videos.html |
| Pivot shift test3 | Fully extend the knee and rotate the foot internally. Apply a valgus (abduction) force while progressively flexing the knee, watching and feeling for translation of the tibia on the femur. | https://www.aafp.org/online/en/home/publications/journals/afp/afp-oct-15-videos.html |
| Meniscal tear | ||
| Joint line tenderness3 | Palpate medially or laterally along the knee to the joint line between the femur and tibial condyles. Pain on palpation is a positive finding. | — |
| McMurray test3 | Flex the hip and knee maximally. Apply a valgus (abduction) force to the knee while externally rotating the foot and passively extending the knee. An audible or palpable snap during extension suggests a tear of the medial meniscus. For the lateral meniscus, apply a varus (adduction) stress during internal rotation of the foot and passive extension of the knee. | http://www.youtube.com/watch?v=ohSzjNj-KCA&NR=1 |
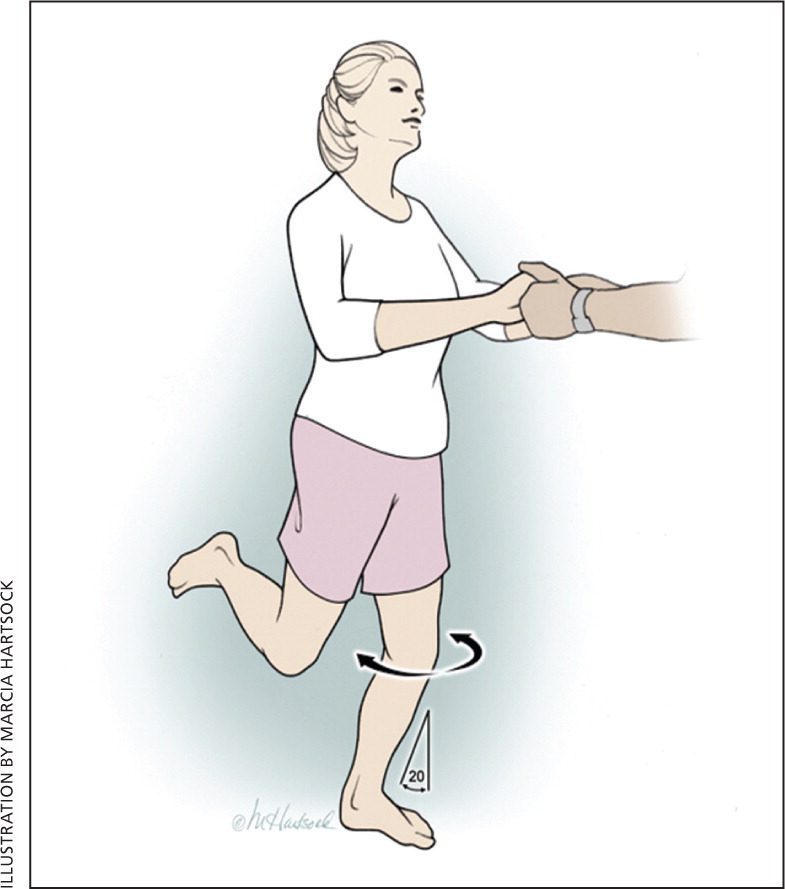
| Thessaly test15 | Hold patient's outstretched hands while he or she stands flat-footed on the floor, internally and externally rotating three times with the knee flexed 20 degrees. | http://www.youtube.com/watch?v=R3oXDvagnic |
| Effusion | ||
| Ballottement test16 | Push the patella posteriorly with two or three fingers using a quick, sharp motion. In the presence of a large effusion, the patella descends to the trochlea, strikes it with a distinct impact, and flows back to its former position. | http://www.youtube.com/watch?NR=1&v=oULBAyfwkaE |
| Maneuver or clinical findings | Positive likelihood ratio* | Negative likelihood ratio* | Probability of injury if maneuver is† | |
|---|---|---|---|---|
| Positive (%) | Negative (%) | |||
| Anterior cruciate ligament tear | ||||
| Pivot shift test3 | 20.3 | 0.4 | 69 | 4 |
| Lachman test3 | 12.4 | 0.14 | 58 | 2 |
| Anterior drawer test3 | 3.7 | 0.6 | 29 | 6 |
| Effusion | ||||
| Ballottement test; noticeable swelling16 | 3.6 | 0.4 | NA | NA |
| Meniscal tear | ||||
| Thessaly test15 | 39.3 | 0.09 | 81 | 1 |
| McMurray test3 | 17.3 | 0.5 | 66 | 5 |
| Age > 40 years, continuation of activity not possible, weight bearing during trauma, and pain with passive flexion17 | 5.8 | 0.9 | 39 | 9 |
| Joint line tenderness3 | 1.1 | 0.8 | 11 | 8 |
Magnetic resonance imaging (MRI) is highly accurate in diagnosing injury to the ACL and posterior cruciate ligament.18 It can be used when historical and physical examination findings are equivocal. Although the use of MRI has been advocated to confirm clinical suspicions before proceeding to arthroscopy,13 the American Academy of Orthopaedic Surgeons states that it is usually not required to diagnose an ACL tear.19 It has been suggested that MRI is better used to rule out internal derangement than to rule it in, because clinical findings are often sufficient for diagnosis.20 Internal derangement is unlikely (less than 2 percent) and MRI typically unnecessary if physical examination maneuvers are negative.3
Meniscal Tear
ILLUSTRATIVE CASE
A 42-year-old man presents two days after injuring his right knee while playing tennis. He twisted his body with the right leg planted on the court surface. He felt a sharp pain and could not continue playing. He reports mild swelling and a sense of clicking in the medial knee with episodes of locking, which prevent full range of motion. Examination reveals medial joint line tenderness, a positive ballottement test, pain with full flexion of the knee, and positive McMurray and Thessaly tests.
Several systematic reviews have examined the diagnostic accuracy of physical examination maneuvers in patients with meniscal tears.3,13,21–26 Although the individual studies have been of varying quality and have had inconsistent results, there is agreement that composite findings from the history and physical examination are more clinically helpful than any examination maneuver alone, and that a thorough examination can be nearly as accurate as magnetic resonance imaging3,20 (Table 413 ).
| History | Physical examination | Diagnosis to consider |
|---|---|---|
| Direct injury to anterior tibia; forced hyperflexion or hyperextension injury; posterior pain; pain with kneeling | Positive sag or posterior drawer test; mild swelling or slow onset; posterior swelling; painful limitation (10 to 20 degrees flexion) | Posterior cruciate ligament tear |
| Pivoting or leaping injury; sense of disruption; audible pop; instability; early swelling (one to two hours) | Positive Lachman, anterior drawer, or pivot shift test; loss of hyperextension | Anterior cruciate ligament tear |
| Squatting, cutting, or twisting injury; trivial twisting injury in older persons; giving way; locking and catching | Joint line tenderness; positive McMurray test; joint effusion; loss of extension (locked knee) | Meniscal tear |
Family physicians must have proficient physical examination skills and must be able to assess how much each finding increases or decreases clinical suspicion of meniscal injury. Some patients will be unable to fully extend the knee, indicating a possible “bucket-handle” meniscal tear.13 Tenderness on the joint line is fairly sensitive (76 percent) for meniscal tear, but is not specific (29 percent).3 The positive and negative likelihood ratios for joint line tenderness are approximately 1.0, so this finding does not provide useful information. A positive McMurray test substantially increases the probability of a meniscal tear; this test has high specificity (97 percent) but low sensitivity (52 percent).3 The Thessaly test is a validated method to assess for meniscal injury and is a valuable tool in the physical examination of patients with an acutely injured knee15,27 (Figure 2). It has been proven more accurate than the McMurray test or the finding of joint line tenderness.15
A combination of historical features and examination findings will help alert physicians to the possibility of meniscal tear more than the results of any one test.17 Features found to be most predictive of meniscal tear include age older than 40 years (odds ratio [OR] = 4.1), weight bearing during trauma (OR = 3.4), pain with passive flexion during examination (OR = 2.7), and inability to continue activity (OR = 2.2).17 The presence of all four of these features significantly increases the likelihood of meniscal tear; if the pretest probability of meniscal tear was 10 percent, the presence of all four factors increases that probability to 39 percent. The absence of all of these factors would decrease the probability to 1 percent.17
Effect of Effusion on Decision Making
The presence of effusion is a predictor of internal derangement; 74 to 91 percent of patients with traumatic injury and effusion have internal derangement of the knee.16,28 The combination of patients reporting swelling and having a positive ballottement test is helpful for detecting effusion (positive likelihood ratio = 3.6 when both are present; negative likelihood ratio = 0.4 when both are absent).16 Although ultrasonography is not routinely necessary for determining the presence of effusion, it can be diagnostic. Compared with MRI, ultrasonography may provide a more convenient, accessible, and cost-effective method of diagnosing effusion.28
Data Sources: A PubMed search was performed using the key terms knee injury and physical examination. Additional sources were obtained from Essential Evidence, the Cochrane Database of Systematic Reviews, and a Google Scholars search. Search dates: January 25, 2011, and September 22, 2011.
