
Am Fam Physician. 2012;86(5):433-440
A more recent article on syphilis is available.
Related letter: Serologic Cross-Reactivity of Syphilis, Yaws, and Pinta
Patient information: See related handout on syphilis, written by the authors of this article.
Author disclosure: No relevant financial affiliations to disclose.
Rates of primary and secondary syphilis have increased in the past decade, warranting renewed attention to the diagnosis and treatment of this disease. Men who have sex with men are particularly affected; however, increases in infection rates have also been noted in women, as well as in all age groups and ethnicities. Physicians need to vigilantly screen high-risk patients. The concurrent rise in congenital syphilis also requires special attention and reemphasizes the need for continued early prenatal care and syphilis screening for all pregnant women. Syphilis infection in patients coinfected with human immunodeficiency virus has also become more common. New experimental diagnostic approaches, including using the B cell chemoattractant chemokine (CXC motif) ligand 13 as a cerebrospinal fluid marker, may help identify suspected neurosyphilis cases. Additionally, point-of-care immunochromatographic strip testing has been suggested for screening high-risk populations in developing countries. Nontreponemal screening tests followed by treponemal confirmatory tests continue to be standard diagnostics; however, interpreting false-negative and false-positive test results, and identifying serofast reactions, can be challenging. Although doxycycline, tetracycline, ceftriaxone, and azithromycin have been used to successfully treat syphilis, penicillin remains the drug of choice in all stages of infection and is the therapy recommended by the Centers for Disease Control and Prevention. Close follow-up is necessary to ensure treatment success.
Syphilis has predictable stages and well-established diagnostic and treatment strategies; however, these warrant revisiting because the incidence of syphilis has been increasing in the past decade. Syphilis is caused by the spirochete Treponema pallidum, and is spread primarily through sexual contact. A high index of suspicion is necessary because of the many clinical manifestations of the disease. From the laboratory standpoint, syphilis can be difficult to diagnose because of a several-week delay between infection and the development of an immunologic response. In addition, a substantial percentage of patients who were treated previously present with serofast reactions, which require careful interpretation to avoid overtreatment. Careful attention to the history and physical examination, testing of high-risk populations, and appropriate monitoring can help keep this disease under control.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Patients with a negative Venereal Disease Research Laboratory or rapid plasma reagin test and strong clinical indicators of primary syphilis should have repeat nontreponemal serology in two weeks. | C | 5 |
| All patients with confirmed syphilis should be tested for human immunodeficiency virus. | C | 5 |
| All sexually active men who have sex with men should have syphilis serology at least annually. | C | 5 |
| Penicillin G benzathine is the first-line treatment for all stages of syphilis, except neurosyphilis. | C | 5 |
| Intravenous aqueous crystalline penicillin G is the first-line treatment for neurosyphilis. | C | 5 |
Epidemiology
In 2000, primary and secondary syphilis rates in the United States were at an all-time low (2.1 cases per 100,000 persons)1; however, outbreaks of the infection were reported in men who have sex with men.2 Rates of infection with primary and secondary syphilis increased 15.2 percent between 2006 and 2007, from 3.3 to 3.8 cases per 100,000 persons.3 Most primary and secondary syphilis cases (84 percent) reported in 2004 to the Centers for Disease Control and Prevention (CDC) were in men.1 Men who have sex with men are particularly affected3; however, increases in infection rates over the past decade have also been noted in women, as well as in all age groups and ethnicities including Asian, black, Hispanic, and white persons. Additionally, the CDC recently reported a 23 percent increase in congenital syphilis in the United States, from 8.2 cases per 100,000 live births in 2005 to 10.1 cases per 100,000 live births in 2008.4
Stages
| Stage | Time | Manifestations | |
|---|---|---|---|
| Common | Uncommon | ||
| Primary | 10 to 90 days | Chancre | Local lymphadenopathy |
| Secondary | 1 to 3 months | Arthralgia, condylomata lata, fatigue, generalized lymphadenopathy, headache, maculopapular/papulosquamous exanthema, myalgia, pharyngitis | Annular syphilis, iritis, pustular syphilis, pyrexia, syphilitic alopecia, ulceronodular syphilis |
| Early latent | After primary or secondary stages, 1 year or less of no symptoms | None | None |
| Late latent | More than 1 year of no symptoms | None | None |
| Tertiary | Months to years | Late neurosyphilis* | Cardiovascular syphilis, gummatous syphilis |
PRIMARY
The classic description of primary syphilis is a solitary nontender genital chancre. This represents the first site of T. pallidum invasion and the resultant dermatologic response to infection. Patients may present to their physician with this finding if noticed; however, the infection site may easily go undetected if it is in a difficult area to visualize, such as the cervix or anus/rectum. Also, chancres are occasionally (2 to 7 percent) found extragenitally, at sites including the fingers, nipples, and oral mucosa.6,7 Patients may have multiple chancres (Figure 1); the presence of such should not dissuade the consideration of syphilis in the differential diagnosis.8

SECONDARY
Untreated primary syphilis progresses to secondary syphilis six to eight weeks after the primary infection. The characteristic exanthem of secondary syphilis involves the trunk, face, and extremities. Morphology tends to be generalized pink to red macules and papules (Figure 2). Several other mucocutaneous manifestations are possible (Figure 3). Syphilitic alopecia is well described in the literature and is characterized as having a “moth-eaten” appearance. Although the moth-eaten appearance occurs only in 4 to 12.5 percent of of patients with secondary syphilis, recognition is crucial because it may be the sole presenting symptom.9

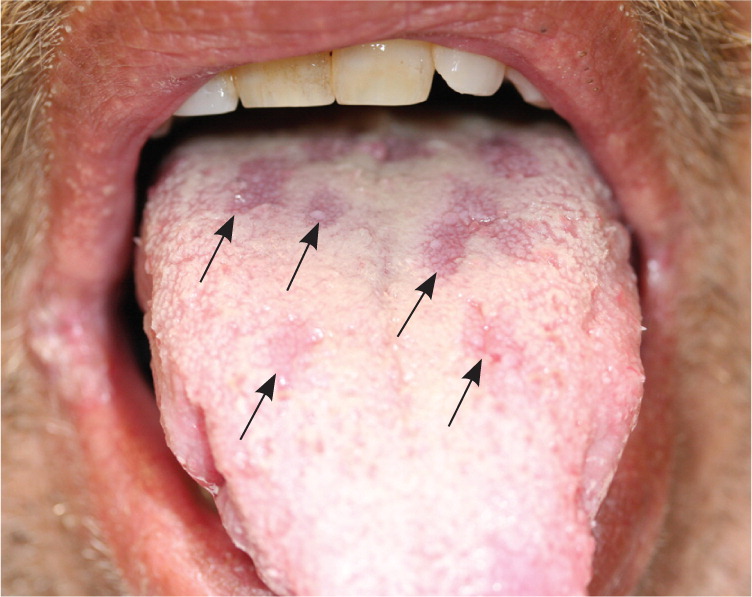
Cutaneous manifestations are caused by direct infiltration of pathogens; therefore, direct visualization of treponemes with dark-field microscopy is possible when sampling lesions. Condylomata lata are an example of these lesions. They are intertriginous mucosal papules that tend to become macerated and form flat, moist, infectious lesions.10 Lues maligna, also known as ulceronodular or malignant syphilis, is a severe form of secondary syphilis. It has been observed in immunosuppressed patients,11–15 as well as in otherwise healthy persons.14,16
LATENT
If untreated in the primary or secondary stage, syphilis can progress to the latent stage, which can be characterized by an absence of symptoms. The latent stage is further divided into early and late latency. The distinction between the two stages is important because it relates to infectivity of the patient. Regarding sexual transmission, patients with syphilis in the early latency stage remain infectious, whereas those with syphilis in the late latency stage are thought to be noninfectious. The CDC regards early latency as a one-year interval without symptoms of primary or secondary syphilis (this is the commonly accepted definition in the United States).17 Late latency is the period beyond one year in which the patient is symptom-free. Patients with unknown infection duration will typically be treated as if they have latent syphilis. Syphilis may remain in latency without treatment in two-thirds of patients, and will progress to the tertiary stage in one-third of patients.18
TERTIARY
Tertiary syphilis is characterized by a persistent low-level burden of pathogens, against which a potent and self-destructive immune response is mounted.19 Three presentations of tertiary syphilis are neurosyphilis, cardiovascular syphilis, and late benign syphilis. Neurosyphilis occurs as a consequence of treponemal penetration of the blood-brain barrier. Cardiovascular syphilis largely affects the great vessels, most commonly manifesting as ascending aortitis.19 Late benign syphilis represents one-half of tertiary syphilis cases and appears as granulomas, gummas, and psoriasiform plaques.20
Neurosyphilis
Neurosyphilis can occur at any stage of infection and has manifold presentations.19 Meningovascular syphilis may result in cerebrovascular accident and can cause widespread or focal changes, depending on the arteries involved. General paresis is characterized by emotional lability, memory deficit, and psychosis. Changes in the posterior columns lead to tabes dorsalis, characterized by sensory ataxia of the lower extremities.19 It is difficult to predict which patients will be affected by these syndromes.
Congenital
Rates of congenital syphilis are increasing, reemphasizing the need for continued early prenatal care and syphilis screening for all pregnant women. Congenital syphilis may result from transplacental transmission or contact with infectious lesions during birth. Two-thirds of neonates with congenital syphilis are asymptomatic at birth.21 In symptomatic infants, signs typically manifest early (birth through 48 months) or late (49 months through the first two decades of life).21 Table 2 lists presentations of congenital syphilis.21 The most common early signs include hepatosplenomegaly, rash, fever, and signs of neurosyphilis, especially bulging fontanelle, seizures, and cranial nerve palsies.21 Late signs may occur in untreated infants and include frontal bossing, nasal cartilage destruction, and dental abnormalities. The high case fatality ratio and significant morbidity associated with congenital syphilis dictates the need for targeted outreach to at-risk mothers, particularly crack cocaine users living in urban areas who have sex with multiple partners in exchange for drugs.
| Presentation | Descriptive findings | Time | Frequency |
|---|---|---|---|
| Rash | Morbilliform eruption resembling acquired secondary syphilis | Early | Common |
| Parrot pseudoparalysis | Painful epiphysitis causing reluctance to move | Early | Uncommon |
| Snuffles | Rhinitis with blood-stained mucus | Early | Uncommon |
| Syphilitic pemphigus | Bullae favoring distal extremities | Early | Uncommon |
| Higouménakis sign | Unilateral enlargement of the sternoclavicular portion of the clavicle | Late | Common |
| Hutchinson teeth | Peg-shaped permanent upper central incisors | Late | Common |
| Mulberry molars | Extra cusps on first molars | Late | Common |
| Olympian brow | Frontal bossing of forehead | Late | Common |
| Saddle nose | Degradation of nasal cartilage | Late | Common |
| Clutton joints | Sterile symmetric effusions of major joints | Late | Uncommon |
| Saber shins | Bowing of tibia | Late | Uncommon |
HIV Coinfection
Syphilis coinfection with human immunodeficiency virus (HIV) has become more common and presents unique challenges. Persons who are HIV positive are at increased risk of developing neurosyphilis,22,23 and tend to have higher cerebrospinal fluid HIV viral loads.24 It is unclear how long it takes to develop clinical neurosyphilis after central nervous system infection. The CDC makes the same recommendations for cerebrospinal fluid examination in persons who are HIV negative and HIV positive: it should be performed in all patients with syphilis and neurologic symptoms, and in all patients with serologic or clinical evidence of treatment failure.5 A recent study found greater success in detecting asymptomatic neurosyphilis in persons who are HIV positive by applying serologic criteria (CD4 cell count less than 350 cells per mm3 and/or rapid plasma reagin [RPR] titer greater than 1:32) instead of stage-based criteria.25 Another new development in the detection of neurosyphilis in patients who are HIV positive is the experimental use of the B cell chemoattractant chemokine (CXC motif) ligand 13 as a cerebrospinal fluid marker.26
Diagnosis
Patients suspected of having syphilis are usually screened with nontreponemal tests, including the Venereal Disease Research Laboratory (VDRL) and RPR tests (Table 3).19 These tests become positive within three weeks of development of the primary chancre, so patients may have negative nontreponemal tests very early in infection.27 In general, only 30 to 40 percent of patients are diagnosed at the primary stage.10 This may be because of small, difficult to visualize, or otherwise unnoticed primary infection sites. Although the chancre may develop within one week of exposure, immunoglobulin M antibodies take two to three weeks to be detectable.28 During this gap, dark-field microscopy is an invaluable tool for directly visualizing pathogens from chancre fluid; however, this method requires special equipment and experienced technicians.
| Test | Explanation | Advantages | Limitations |
|---|---|---|---|
| Dark-field microscopy | Direct visualization of spirochetes in ulcer exudate fluid |
|
|
| Nontreponemal serology (Venereal Disease Research Laboratory test, rapid plasma reagin test) | Detects antibodies to cardiolipin in blood |
|
|
| Treponemal serology (fluorescent treponemal antibody absorption assay, Treponema pallidum particle agglutination test) | Detects antibodies to T. pallidum in blood |
|
|
Patients with a positive RPR or VDRL test should undergo specific treponemal testing, such as the fluorescent treponemal antibody absorption assay or the T. pallidum particle agglutination test to confirm infection with T. pallidum. Patients with a negative VDRL or RPR test and strong clinical indicators of primary syphilis should have repeat nontreponemal serology in two weeks.5 Persons with confirmed syphilis should be tested for HIV.5 Syphilis is a reportable disease in every state and must be reported in accordance with state and local health departments.
Successful treatment of primary and secondary syphilis should be followed by a fourfold decline in RPR/VDRL titer over the next three to six months.29 Nontreponemal test titers may decline slower than fourfold over three to six months in patients who were reinfected with syphilis. Nontreponemal tests may revert to negative following treatment (seroreversion); this is more likely to occur with low initial titers and with treatment in the primary or secondary stage.29 Some patients' nontreponemal titers do not serorevert following successful treatment; this is called a serofast reaction.5 All patients should have repeat clinical and serologic evaluation (with the same nontreponemal test used at diagnosis) six and 12 months after treatment.5 Patients with continued clinical signs and symptoms, or a fourfold increase in titer (compared with the nontreponemal titer at diagnosis), should be treated again and retested for HIV.5 Even following successful treatment, specific treponemal tests may remain positive for years and should not be used to assess treatment response.5 All sexually active men who have sex with men should have syphilis serology at least annually.5
Cerebrospinal fluid examination should be performed in patients with syphilis and neurologic symptoms, and in patients with clinical or serologic evidence of treatment failure.5 Recent advances in strain-typing have identified T. pallidum isolates that have an increased association with neurosyphilis.30 Studying these particular isolates may help to better understand the pathogenesis of neurosyphilis and lead to improved diagnosis and treatment.
Recently, point-of-care immunochromatographic strip testing has been suggested for screening high-risk populations in developing countries with low diagnostic capacity.31 Immunochromatographic strip tests use a strip containing treponemal antigens that react with antibodies to syphilis in the whole blood or serum of infected persons to produce a visualized change on the test strip. Although not approved by the U.S. Food and Drug Administration for use in the United States, these inexpensive, rapid tests have been reported in a recent review to have a sensitivity of 78 to 100 percent and specificity of 97 to 99 percent.31
Management
The treatment plan for syphilis, as detailed by the CDC, remains relatively unchanged in recent years and continues to vary with stage of infection (Table 4).5 Primary, secondary, and early latent syphilis can be treated with a single intramuscular dose of 2.4 million units of penicillin G benzathine.5 A longer treatment course of 2.4 million units of intramuscular penicillin G benzathine every week for three weeks is recommended for late latent syphilis, for tertiary syphilis, or if infection duration is unknown. Neurosyphilis requires 3 to 4 million units of intravenous aqueous crystalline penicillin G every four hours for 10 to 14 days.5
| Stage | Treatment | |
|---|---|---|
| Primary | Penicillin G benzathine, 2.4 million units intramuscularly once | |
| In persons allergic to penicillin: | ||
| Doxycycline,* 100 mg orally twice daily for 14 days | ||
| Tetracycline,† 500 mg orally four times daily for 14 days | ||
| Ceftriaxone (Rocephin),‡ 1 g intravenously or intramuscularly once daily for 10 to 14 days | ||
| Azithromycin (Zithromax),‡ 2 g orally once | ||
| Secondary | Penicillin G benzathine, 2.4 million units intramuscularly once | |
| In persons allergic to penicillin: | ||
| Doxycycline,* 100 mg orally twice daily for 14 days | ||
| Tetracycline,† 500 mg orally four times daily for 14 days | ||
| Ceftriaxone,‡ 1 g intravenously or intramuscularly once daily for 10 to 14 days | ||
| Azithromycin,‡ 2 g orally once | ||
| Early latent | Penicillin G benzathine, 2.4 million units intramuscularly once | |
| Late latent | Penicillin G benzathine, 2.4 million units intramuscularly weekly for three weeks | |
| Tertiary | Penicillin G benzathine, 2.4 million units intramuscularly weekly for three weeks | |
| Neurosyphilis | Aqueous crystalline penicillin G, 18 to 24 million units daily administered as 3 to 4 million units intravenously every 4 hours for 10 to 14 days | |
| or | ||
| Penicillin G procaine, 2.4 million units intramuscularly once daily for 10 to 14 days | ||
| plus | ||
| Probenecid, 500 mg orally four times daily for 10 to 14 days | ||
| Congenital | Complex treatment | |
| Reference the Centers for Disease Control and Prevention treatment plan at http://www.cdc.gov/std/treatment/2010/STD-Treatment-2010-RR5912.pdf | ||
Patients may develop an acute febrile illness known as the Jarisch-Herxheimer reaction during the first 24 hours following initial treatment. This is largely the result of massive lysis of the pathogen, spilling large quantities of inflammatory cytokines into the bloodstream.32 Patients with primary and secondary syphilis who are allergic to penicillin may be treated (with caution and close follow-up) with doxycycline, tetracycline, ceftriaxone (Rocephin), or azithromycin (Zithromax); however, azithromycin is not recommended for pregnant patients or men who have sex with men.5 Penicillin desensitization is recommended for pregnant patients who are allergic to penicillin.5 Sex partners of patients who have syphilis at any stage should be evaluated clinically and serologically, and treated appropriately.5
Data Sources: A PubMed search was completed in Clinical Queries using the key term syphilis. The search included meta-analyses, systematic reviews, randomized controlled trials, prospective studies, case studies, and reviews. Also searched were the Cochrane database, the U.S. Preventive Services Task Force, UpToDate, and Dynamed. Search date: March 29, 2010.
