
A more recent article on acute otitis externa is available.
Am Fam Physician. 2012;86(11):1055-1061
Author disclosure: No relevant financial affiliations to disclose.
Acute otitis externa is a common condition involving inflammation of the ear canal. The acute form is caused primarily by bacterial infection, with Pseudomonas aeruginosa and Staphylococcus aureus the most common pathogens. Acute otitis externa presents with the rapid onset of ear canal inflammation, resulting in otalgia, itching, canal edema, canal erythema, and otorrhea, and often occurs following swimming or minor trauma from inappropriate cleaning. Tenderness with movement of the tragus or pinna is a classic finding. Topical antimicrobials or antibiotics such as acetic acid, aminoglycosides, polymyxin B, and quinolones are the treatment of choice in uncomplicated cases. These agents come in preparations with or without topical corticosteroids; the addition of corticosteroids may help resolve symptoms more quickly. However, there is no good evidence that any one antimicrobial or antibiotic preparation is clinically superior to another. The choice of treatment is based on a number of factors, including tympanic membrane status, adverse effect profiles, adherence issues, and cost. Neomycin/polymyxin B/hydrocortisone preparations are a reasonable first-line therapy when the tympanic membrane is intact. Oral antibiotics are reserved for cases in which the infection has spread beyond the ear canal or in patients at risk of a rapidly progressing infection. Chronic otitis externa is often caused by allergies or underlying inflammatory dermatologic conditions, and is treated by addressing the underlying causes.
Otitis externa, also called swimmer's ear, involves diffuse inflammation of the external ear canal that may extend distally to the pinna and proximally to the tympanic membrane. The acute form has an annual incidence of approximately 1 percent1 and a lifetime prevalence of 10 percent.2 On rare occasions, the infection invades the surrounding soft tissue and bone; this is known as malignant (necrotizing) otitis externa, and is a medical emergency that occurs primarily in older patients with diabetes mellitus.3 Otitis externa lasting three months or longer, known as chronic otitis externa, is often the result of allergies, chronic dermatologic conditions, or inadequately treated acute otitis externa.
| Clinical recommendation | Evidence rating | References | Comments |
|---|---|---|---|
| Acute otitis externa should be distinguished from other possible causes of ear canal inflammation. | C | 4 | Different and overlapping pathologies may require alteration in treatment |
| Topical antimicrobial otic preparations should be considered the first-line treatment foruncomplicated acute otitis externa. | A | 4, 14–16 | Choose specific preparation based on risk of adverse effects, tympanic membrane status, cost, adherence issues, etc. |
| Addition of a topical corticosteroid may result in faster resolution of symptoms such as pain, canal edema, and canal erythema. | B | 4, 14–16 | May be partly dependent on strength of corticosteroid |
| Systemic antibiotics should be used only if the infection has spread beyond the ear canal or in patients at high risk of such spread. | B | 4, 14, 16 | — |
| Use of aural toilet should be considered to remove debris from the ear canal before treatment. | C | 4, 16 | Widely performed in research studies, but no data on effectiveness |
Etiology
In North America, 98 percent of cases of acute otitis externa are caused by bacteria.4 The two most common isolates are Pseudomonas aeruginosa and Staphylococcus aureus. However, a wide variety of other aerobic and anaerobic bacteria have been isolated.5,6 Approximately one-third of cases are polymicrobial.4 Fungal pathogens, primarily those of the Aspergillus and Candida species, occur more often in tropical or subtropical environments and in patients previously treated with antibiotics.7–9 Inflammatory skin disorders and allergic reactions may cause noninfectious otitis externa, which can be chronic.
Risk Factors
Several factors may predispose patients to the development of acute otitis externa (Table 1).4,10 One of the most common predisposing factors is swimming, especially in fresh water. Other factors include skin conditions such as eczema and seborrhea, trauma from cerumen removal, use of external devices such as hearing aids, and cerumen buildup.4 These factors appear to work primarily through loss of the protective cerumen barrier, disruption of the epithelium (including maceration from water retention), inoculation with bacteria, and increase in the pH of the ear canal.10–12
| Anatomic abnormalities |
| Canal stenosis |
| Exostoses |
| Hairy ear canals |
| Canal obstruction |
| Cerumen obstruction |
| Foreign body |
| Sebaceous cyst |
| Cerumen/epithelial integrity |
| Cerumen removal |
| Earplugs |
| Hearing aids |
| Instrumentation/itching |
| Dermatologic conditions |
| Eczema |
| Psoriasis |
| Seborrhea |
| Other inflammatory dermatoses |
| Water in ear canal |
| Humidity |
| Sweating |
| Swimming or other prolonged water exposure |
| Miscellaneous |
| Purulent otorrhea from otitis media |
| Soap |
| Stress |
| Type A blood |
Prevention
A number of preventive measures have been recommended, including use of earplugs while swimming, use of hair dryers on the lowest settings and head tilting to remove water from the ear canal, and avoidance of self-cleaning or scratching the ear canal. Acetic acid 2% (Vosol) otic solutions are also used, either two drops twice daily or two to five drops after water exposure. However, no randomized trials have examined the effectiveness of any of these measures.
Diagnosis
Acute otitis externa is diagnosed clinically based on signs and symptoms of canal inflammation (Table 24 ; Figures 1 and 2). Presentation can range from mild discomfort, itching, and minimal edema to severe pain, complete canal obstruction, and involvement of the pinna and surrounding skin. Pain is the symptom that best correlates with the severity of disease.13 Mild fever may be present, but a temperature greater than 101°F (38.3°C) suggests extension beyond the auditory canal.
| Onset of symptoms within 48 hours in the past three weeks | |
| and | |
| Symptoms of ear canal inflammation: | |
| Ear pain, itching, or fullness | |
| With or without hearing loss or jaw pain | |
| and | |
| Signs of ear canal inflammation: | |
| Tenderness of tragus/pinna or ear canal edema/erythema | |
| With or without otorrhea, tympanic membrane erythema, cellulitis of the pinna, or local lymphadenitis | |
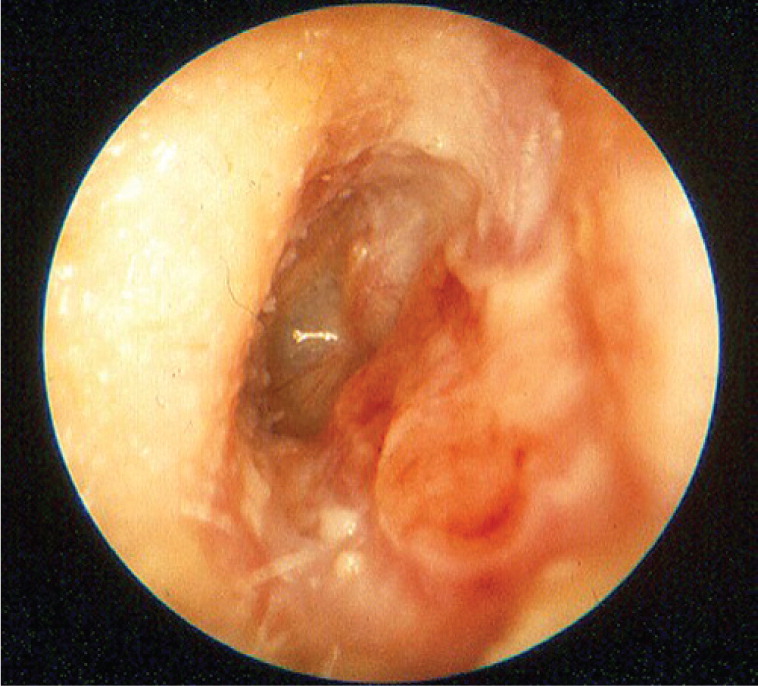
Acute otitis externa should be distinguished from other causes of ear canal inflammation4 (Table 3; see previous AFP article on ear pain [https://www.aafp.org/afp/2008/0301/p621.html]). Proper evaluation includes a history of presenting and associated symptoms, water exposure, local trauma/cerumen removal, inflammatory skin disorders, diabetes, ear surgeries, and local radiotherapy. Physical examination should include the auricle and surrounding lymph nodes, a skin examination, otoscopy of the ear canal, and verification that the tympanic membrane is intact. Tenderness with movement of the tragus or pinna is a classic finding.
| Condition | Distinguishing characteristics | Comment |
|---|---|---|
| Acute otitis media | Presence of middle ear effusion, no tragal/pinnal tenderness | Use pneumatic otoscopy or tympanometry, treat with systemic antibiotics |
| Chronic otitis externa | Itching is often predominant symptom, erythematous canal, lasts more than three months | Treat underlying causes/conditions |
| Chronic suppurative otitis media | Chronic otorrhea, nonintact tympanic membrane | Control otitis externa symptoms, then treat otitis media |
| Contact dermatitis | Allergic reaction to materials (e.g., metals, soaps, plastics) in contact with the skin/epithelium; itching is predominant symptom | Check for piercings, hearing aids, or earplug use; discontinue exposure when possible |
| Eczema | Itching is predominant symptom; often chronic; history of atopy, outbreaks in other locations | Consider treatment with topical corticosteroids |
| Furunculosis | Focal infection, may be pustule or nodule, often in distal canal | Consider treatment with heat, incision and drainage, or systemic antibiotics; can progress to diffuse otitis externa |
| Malignant otitis externa | High fever, granulation tissue or necrotic tissue in ear canal, may have cranial nerve involvement; patient with diabetes mellitus or immunocompromise, elevated erythrocyte sedimentation rate, findings on computed tomography | Medical emergency with high morbidity rate and possible mortality; warrants emergent consultation with otolaryngologist, hospitalization, intravenous antibiotics, debridement |
| Myringitis | Tympanic membrane inflammation, may have vesicles; pain is often severe, no canal edema | Usually results from acute otitis media or viral infection |
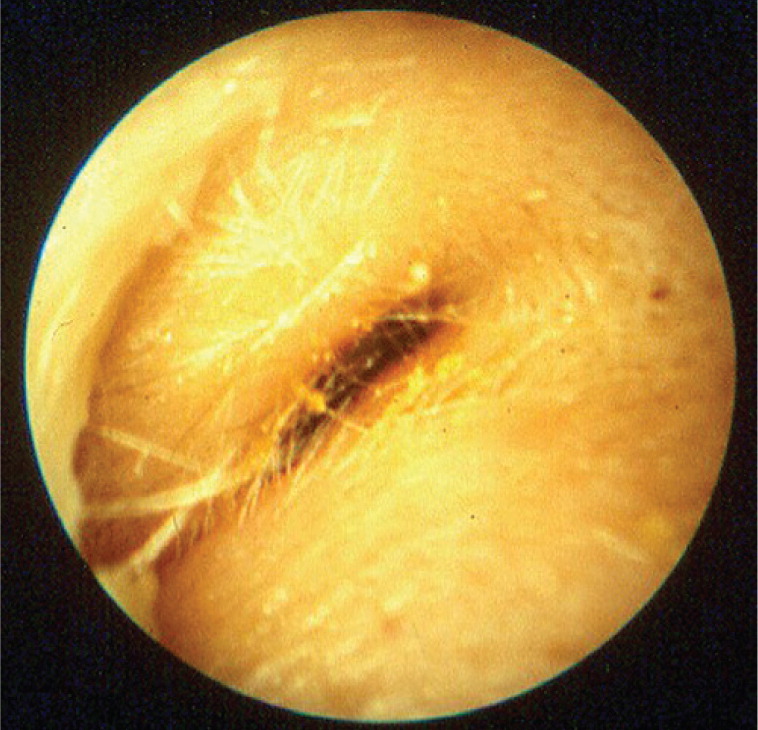
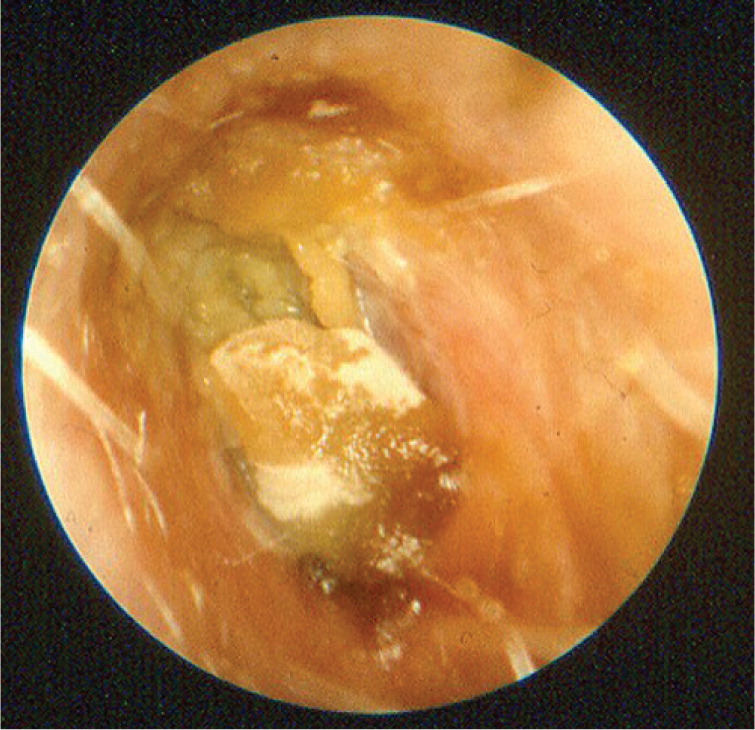
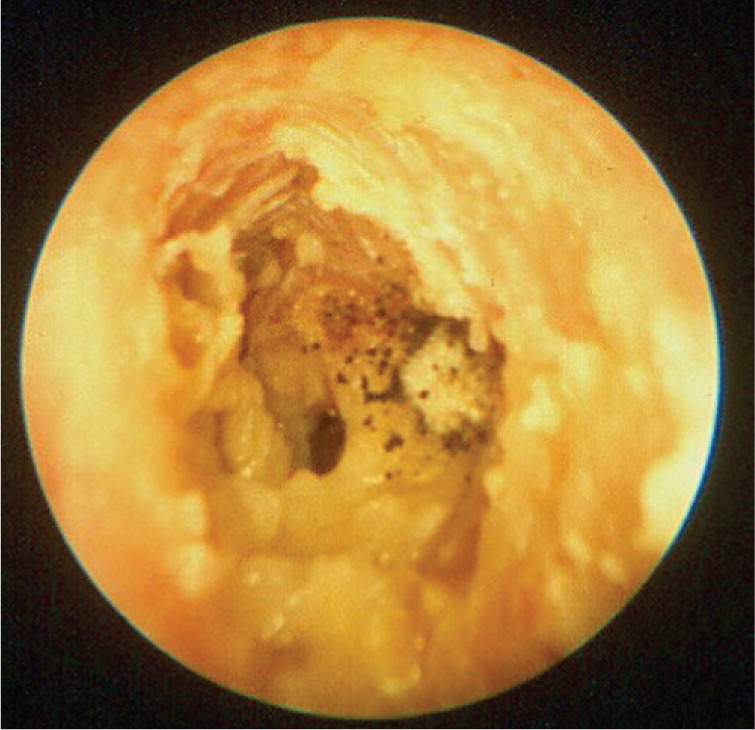
| Otomycosis | Itching is predominant symptom, thick material in canal, less edema; may see fungal elements on otoscopy (Figures 3 and 4) | Can coexist with bacterial infections; treat with acetic acid (Vosol), half acetic acid/half alcohol, or topical antifungals; meticulous cleaning of ear canal |
| Ramsay Hunt syndrome | Herpetic ulcers in canal; may have facial numbness/paralysis, severe pain, loss of taste | Treatment includes antivirals, systemic corticosteroids |
| Referred pain | Normal ear examination | Look for other causes based on patterns of referred pain |
| Seborrhea | Itching and rash on hairline, face, scalp | Treatment includes lubricating or moisturizing the external auditory canal |
| Sensitization to otics | Severe itching, maculopapular or erythematous rash in conchal bowl and canal; may have streak on pinna where preparation contacted skin; vesicles may be present | Type IV delayed hypersensitivity reaction to neomycin or other components of otic solutions; discontinue offending agent; treat with topical corticosteroids |
Because otitis externa can cause tympanic membrane erythema, pneumatic otoscopy or tympanometry should be used to differentiate it from otitis media. Otomycosis is classically associated with itching, thick material in the ear canal, and failure to improve with use of topical antibacterials. Otomycosis can sometimes be identified during otoscopy (Figures 3 and 4), although nonpathogenic saprophytic fungi may also be found.
Malignant otitis externa may be suspected in older patients with diabetes mellitus or immunocompromise who have refractory purulent otorrhea and severe otalgia that may worsen at night. Clinical findings include granulation tissue in the external auditory canal, especially at the bone-cartilage junction. Extension of the infection beyond the auditory canal can cause lymphadenopathy, trismus, and facial nerve and other cranial nerve palsies.
Treatment
TOPICAL MEDICATIONS
Topical antimicrobials, with or without topical corticosteroids, are the mainstay of treatment for uncomplicated acute otitis externa. Topical antimicrobials are highly effective compared with placebo, demonstrating an absolute increase in clinical cure rate of 46 percent or a number needed to treat of slightly more than two.4,14–16 Topical agents come in a variety of preparations and combinations; a recent systematic review included 26 different topical interventions.15 In some studies, ophthalmic preparations have been used off-label to treat otitis externa.14,15 Ophthalmic preparations may be better tolerated than otic preparations, possibly due to differences in pH between the preparations, and may help facilitate compliance with treatment recommendations. Commonly studied antimicrobial agents include aminoglycosides, polymyxin B, quinolones, and acetic acid. No consistent evidence has shown that any one agent or preparation is more effective than another.4,14–16 There is limited evidence that use of acetic acid alone may require two additional days for resolution of symptoms compared with other agents, and that it is less effective if treatment is required for more than seven days.15
Current guidelines recommend factoring in the risk of adverse effects, adherence issues, cost, patient preference, and physician experience. Some components found in otic preparations may cause contact dermatitis.17 Hypersensitivity to aminoglycosides, particularly neomycin, may develop in up to 15 percent of the population, and has been identified in approximately 30 percent of patients who also have chronic or eczematous otitis externa.17,18 Adherence to topical therapy increases with ease of administration, such as less frequent dosing.19 The addition of a topical corticosteroid yields more rapid improvement in symptoms such as pain, canal edema, and erythema.4,14–16 Cost varies considerably for the different preparations20,21 (Table 44,14–16,20,21 ).
| Component | Cost of generic (brand) | Dosage | Use if tympanic membrane perforation? | Comments |
|---|---|---|---|---|
| Acetic acid 2% (Vosol) | $39 for 15 mL* ($36 for 15 mL)* | Four to six times daily | No | May cause pain and irritation; may be less effective than other treatments if use is required beyond one week; often used as prophylactic agent |
| Ciprofloxacin 0.3%/dexamethasone 0.1% (Ciprodex) | Not available ($160 for 7.5 mL)* | Twice daily | Yes | Low risk of sensitization |
| Hydrocortisone 2%/acetic acid 1% (Vosol HC) | $220 for 10 mL† ($215 for 10 mL)* | Four to six times daily | No | May cause pain and irritation |
| Neomycin/polymyxin B/hydrocortisone, solution or suspension | $28 for 10-mL solution; $30 for 10-mL suspension† ($85 for 10-mL solution; $78 for 10-mL suspension)† | Three to four times daily | No | Ototoxic; higher risk of contact hypersensitivity; avoid in chronic/eczematous otitis externa4 |
| Ofloxacin 0.3% | $60 for 5 mL; $93 for 10 mL† ($80 for 5 mL; $143 for10 mL)† | Once to twice daily | Yes | Low risk of sensitization |
ORAL ANTIBIOTICS
Systemic antibiotics increase the risks of adverse effects, generation of resistant organisms, and recurrence. They also increase time to clinical cure and do not improve outcomes compared with a topical agent alone in uncomplicated otitis externa.1,6,16,22 Systemic antibiotics should be used only when the infection has spread beyond the ear canal, or when there is uncontrolled diabetes, immunocompromise, a history of local radiotherapy, or an inability to deliver topical antibiotics.4,14,16
TREATMENT METHODS
Use of a topical otic preparation without culture is a reasonable treatment approach for patients who have mild symptoms of otitis externa. If the tympanic membrane is intact and there is no concern of hypersensitivity to aminoglycosides, a neomycin/polymyxin B/hydrocortisone otic preparation would be a first-line therapy because of its effectiveness and low cost. Ofloxacin and ciprofloxacin/dexamethasone (Ciprodex) are approved for middle ear use and should be used if the tympanic membrane is not intact or its status cannot be determined visually 4; these also may be useful if patients are hypersensitive to neomycin, or if nonadherence to treatment because of dosing frequency is an issue. Use of a corticosteroid-containing preparation is recommended to provide more rapid relief when symptoms warrant.
Patients should be taught to properly administer otic medications. The patient should lie down with his or her affected side facing upward, running the preparation along the side of the ear canal until it is full and gently moving the pinna to relieve air pockets. The patient should remain in this position for three to five minutes, after which the canal should not be occluded, but rather left open to dry.4 It may benefit the patient to have another person administer the ear drops, because only 40 percent of patients self-medicate appropriately.23 Patients should be instructed to minimize trauma to (and manipulation of) the ear, and to avoid water exposure, including abstinence from water sports for a week or, at minimum, avoidance of submersion.
When there is marked canal edema, a wick of compressed cellulose or ribbon gauze may be placed in the canal to facilitate antimicrobial or antibiotic administration. Wick placement permits antibiotic drops to reach portions of the external auditory canal that are inaccessible because of canal swelling. As the canal responds to treatment and patency returns to the ear canal, the wick often falls out.
ANALGESIA
Pain is a common symptom of acute otitis externa, and can be debilitating.12 Oral analgesics are the preferred treatment. First-line analgesics include nonsteroidal anti-inflammatory drugs and acetaminophen. When ongoing frequent dosing is required to control pain, medications should be administered on a scheduled rather than as-needed basis. Opioid combination pills may be used when symptom severity warrants. Benzocaine otic preparations may compromise the effectiveness of otic antibiotic drops by limiting contact between the drop and the ear canal. The lack of published data supporting the effectiveness of topical benzocaine preparations in otitis externa limits the role of such treatments.
CLEANING THE CANAL
Acute otitis externa can be associated with copious material in the ear canal. Consensus guidelines published by the American Academy of Otolaryngology recommend that such material be removed to achieve optimal effectiveness of the topical antibiotics.4,16 However, no randomized controlled trials have examined the effectiveness of aural toilet, and this is not typically done in most primary care settings.4,15 Topical medications rely on direct contact with the infected skin of the ear canal; hence, aural toilet takes on greater importance when the volume or thickness of the debris in the ear canal is great. Guidelines recommend aural toilet by gentle lavage suctioning or dry mopping under otoscopic or microscopic visualization to remove obstructing material and to verify tympanic membrane integrity.4 Lavage should be used only if the tympanic membrane is known to be intact, and should not be performed on patients with diabetes because of the potential risk of causing malignant otitis externa.4 Pain medications may be required during the procedure.
CHRONIC OTITIS EXTERNA
The treatment of chronic otitis externa depends on the underlying causes. Because most cases are caused by allergies or inflammatory dermatologic conditions, treatment includes the removal of offending agents and the use of topical or systemic corticosteroids. Chronic or intermittent otorrhea over weeks to months, particularly with an open tympanic membrane, suggests the presence of chronic suppurative otitis media. Initial treatment efforts are similar to those for acute otitis media. With control of the symptoms of otitis externa, attention can shift to the management of chronic suppurative otitis media.
Follow-up and Referral
Most patients will experience considerable improvement in symptoms after one day of treatment. If there is no improvement within 48 to 72 hours, physicians should reevaluate for treatment adherence, misdiagnosis (Table 3), sensitivity to ear drops, or continued canal patency. The physician should consider culturing material from the canal to identify fungal and antibiotic-resistant pathogens if the patient does not improve after initial treatment efforts or has one or more predisposing risk factors, or if there is suspicion that the infection has extended beyond the external auditory canal. There is a lack of data regarding optimal length of treatment; as a general rule, antimicrobial otics should be administered for seven to 10 days, although in some cases complete resolution of symptoms may take up to four weeks.4,15
Consultation with an otolaryngologist or infectious disease subspecialist may be warranted if malignant otitis externa is suspected; in cases of severe disease, lack of improvement or worsening of symptoms despite treatment, and unsuccessful lavage; or if the primary care physician determines that aural toilet or ear wick insertion is warranted, but is unfamiliar with or concerned about performing the procedure.
Data Sources: We performed multiple searches of PubMed Clinical Queries using the search term otitis externa. We also searched Essential Evidence Plus, the Cochrane Database of Systematic Reviews, the National Guideline Clearinghouse, Clinical Evidence, Dynamed, and UpToDate. Search dates: January 1, 2011, through April 6, 2011.
