A more recent article on diagnosis and management of hip fractures is available.
Am Fam Physician. 2014;89(12):945-951
Patient information: See related handout on hip fractures, written by the authors of this article.
Author disclosure: No relevant financial affiliations.
Hip fractures cause significant morbidity and are associated with increased mortality. Women experience 80% of hip fractures, and the average age of persons who have a hip fracture is 80 years. Most hip fractures are associated with a fall, although other risk factors include decreased bone mineral density, reduced level of activity, and chronic medication use. Patients with hip fractures have pain in the groin and are unable to bear weight on the affected extremity. During the physical examination, displaced fractures present with external rotation and abduction, and the leg will appear shortened. Plain radiography with cross-table lateral view of the hip and anteroposterior view of the pelvis usually confirms the diagnosis. If an occult hip fracture is suspected and plain radiography is normal, magnetic resonance imaging should be ordered. Most fractures are treated surgically unless the patient has significant comorbidities or reduced life expectancy. The consulting orthopedic surgeon will choose the surgical procedure. Patients should receive prophylactic antibiotics, particularly against Staphylococcus aureus, before surgery. In addition, patients should receive thromboembolic prophylaxis, preferably with low-molecular-weight heparin. Rehabilitation is critical to long-term recovery. Unless contraindicated, bisphosphonate therapy should be used to reduce the risk of another hip fracture. Some patients may benefit from a fall-prevention assessment.
Older patients commonly experience hip fractures, which cause significant morbidity and are associated with increased mortality. The family physician's role involves multiple objectives: identify patients at increased risk of a hip fracture, promptly diagnose a hip fracture, facilitate long-term rehabilitation, reduce the risk of another hip fracture, and manage comorbid conditions.1–4
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Plain radiography should be the initial diagnostic test in patients with suspected hip fracture. | C | 5 |
| Hip fracture surgery should be performed 24 to 48 hours after a fracture unless a delay is needed to stabilize comorbidities. | C | 34 |
| Patients undergoing hip fracture surgery should receive thromboembolic and antibiotic prophylaxis. | A | 46–48, 50 |
| Following a hip fracture, patients should usually be treated with a bisphosphonate, regardless of their bone mineral density, unless contraindicated. | C | 53 |
| Following a hip fracture, most patients should have a formal fall-prevention assessment. | C | 55 |
| Patients should receive post-fracture rehabilitation to help restore functional capability. | B | 56 |
Epidemiology
Women experience 80% of all hip fractures.5 The average age at the time of the fracture is 80 years, and almost all patients are older than 65 years.5 The lifetime prevalence of a hip fracture is 20% for women and 10% for men.1 The projection of annual new hip fractures by 2050 ranges from 500,000 to 1 million.6 The estimated annual cost in the United States is approximately $10.3 to $15.2 billion.7
Hip fractures are associated with increased mortality; 12% to 17% of patients with a hip fracture die within the first year, and the long-term increased risk of death is twofold.8,9 Of the patients who survive, only one-half walk independently again, and 20% must move to a long-term care facility.1 With regard to functional independence, 50% of patients recover prefracture capability of activities of daily living, and 25% recover full capability of their instrumental activities of daily living.10
Risk Factors
Sex and age are nonmodifiable risk factors that are highly associated with an increased risk of hip fracture (Table 111–23 ). Women older than 85 years are 10 times more likely to sustain a hip fracture than those 60 to 69 years of age.11 A previous hip fracture, a family history of hip fracture, and low socioeconomic status are also associated with an increased risk.12–15,24 Hip fracture clinical risk scores have been developed to identify high-risk patients in the primary care setting (see one example at https://www.aafp.org/afp/2007/0715/p273.html).3
| Nonmodifiable | |
| Age > 65 years11 | |
| Family history of hip fracture12 | |
| Female sex13 | |
| Low socioeconomic status14,15 | |
| Prior hip fracture12 | |
| Modifiable | |
| Chronic medications16–19 | |
| Levothyroxine (decreases bone density) | |
| Loop diuretics (impair calcium absorption in kidneys) | |
| Proton pump inhibitors (reduce calcium absorption) | |
| Selective serotonin reuptake inhibitors/sedatives (increase risk of falls caused by sedation, postural hypotension) | |
| Decreased bone mineral density (osteoporosis)20 | |
| Falls21 | |
| Reduced level of activity 22 | |
| Vitamin D deficiency 23 | |
The modifiable risk factors for hip fracture include falls, decreased bone mineral density, reduced level of activity, and chronic medication use. A fall is the most significant risk factor for hip fracture, with 90% of fractures associated with a fall.21 Falls usually occur from a standing position and are associated with reduced protective reactions, slower reaction times, and reduced overall strength.25 A fall may create a fear of future falls, which leads to decreased activity and mobility, and increased tension and tightening of the muscles.26,27 Many older persons become less active as they age, which increases their risk of a fracture.22
A bone mineral density T-score less than –2.5, as measured by dual energy x-ray absorptiometry, is associated with an increased risk of fractures.20 Low bone mineral density scores are associated with inadequate calcium intake, vitamin D deficiency, and a family history of osteoporosis. Vitamin D levels less than 20 ng per mL (50 nmol per L) are associated with an increased risk of falls.23
Several medications are associated with an increased risk of falls or fractures.16 Psychoactive medications, including selective serotonin reuptake inhibitors and benzodiazepines, are most consistently associated with an increased risk of falls.16,17 Long-term use of proton pump inhibitors18 and higher dosages of levothyroxine are associated with an increased risk of fractures.19
History
Patients with hip fracture have pain in the groin and are unable to bear weight on the affected extremity. Pain may be referred to the distal femur or upper knee. Rarely, a patient may be able to walk with a cane, crutches, or a walker. If the patient is able to walk, there is typically worsening pain in the buttock or groin with weight bearing and ambulation. When an older person presents with hip pain after a fall, he or she should be treated as if a hip fracture has occurred, until proven otherwise.
Physical Examination
A stress fracture or a nondisplaced fracture may have no obvious deformity. However, most patients have some fracture displacement. As a result, when the patient lies in the supine position, the leg is held in external rotation and abduction, and appears shortened. Pain is elicited with rotation, such as with the log roll maneuver, which involves gentle internal and external rotation of the lower leg and thigh in the supine position. In addition, a fracture may be suspected if groin pain is elicited when applying an axial load to the affected extremity. Because of the pain and instability, patients are unable to perform an active straight leg raise. Ecchymosis is rarely present initially. Distal pulses and sensation should be assessed and documented. Patients should be examined for any additional associated injuries.
Diagnostic Testing
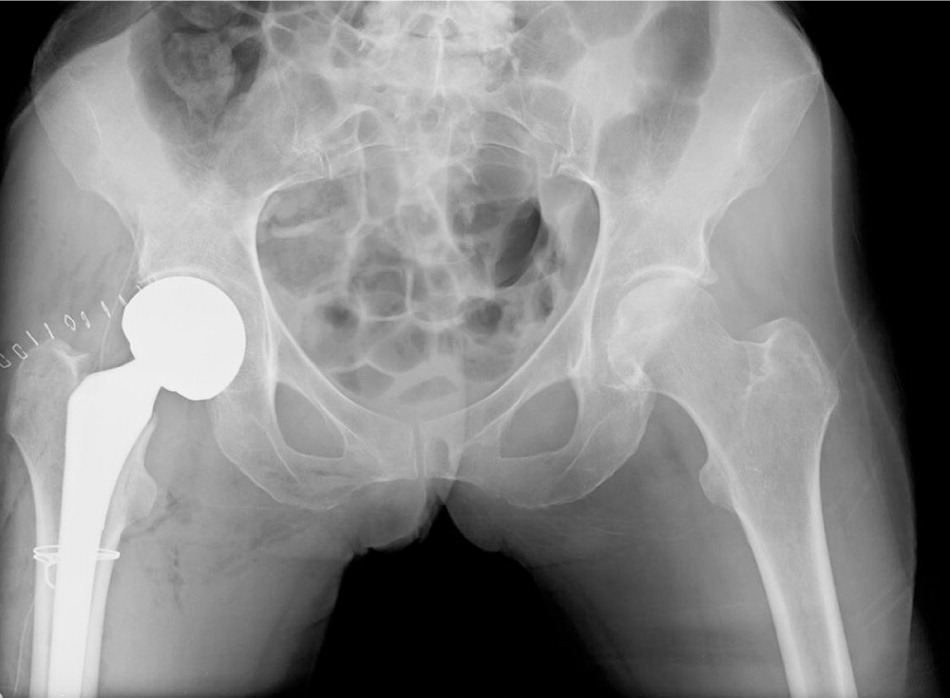
Plain radiography is the initial diagnostic test for hip fracture5 (Figures 1 through 5). A cross-table lateral view of the hip and an anteroposterior view of the pelvis are appropriate. The frog-leg view should be avoided; positioning the limb for this view results in severe pain and can cause displacement of a nondisplaced fracture or worsen a displaced fracture.28 If radiography is negative and a hip fracture is still suspected, magnetic resonance imaging or a bone scan should be performed.29 The imaging study should be evaluated for other possibilities, such as pelvic, stress, or pathologic fractures. Computed tomography may be used, although it may not detect trabecular bone injuries in osteoporotic fractures or reveal bone marrow edema surrounding the fracture line.28




Management
Hip fractures are classified by location for prognostic implications. The two categories are extracapsular (intertrochanteric and subtrochanteric) and intracapsular (femoral head and neck); these are summarized in Table 2.30 The intertrochanteric region contains a large amount of cancellous bone and an adequate blood supply.30 As a result, fractures in this region typically heal well with open reduction and internal fixation, which involves surgery to reduce the displaced bone, followed by internal fixation of the fracture with plates or screws. Subtrochanteric fractures, however, have an increased need for intramedullary rods or nails (impact devices) and have a higher rate of impact failure, mainly because of the high stresses on this part of the femur. The femoral neck region has a thin periosteum, little cancellous bone, and a relatively poor blood supply.30 Consequently, fractures in the intracapsular region have a higher incidence of avascular necrosis, nonunion or malunion, and degenerative changes.
| Category | Characteristic | Significance | |
|---|---|---|---|
| Extracapsular | Large amount of cancellous bone and good blood supply | Typically heals well, although subtrochanteric has higher rate of impact device failure | |
| |||
| Intracapsular | Little cancellous bone and relatively poor blood supply | Higher incidence of avascular necrosis, nonunion, malunion, and degenerative changes | |
| |||
Initially, care should focus on adequate analgesia and consultation with an orthopedic surgeon. Surgery is the most viable option for most patients. Nonsurgical interventions are reserved for patients with severe debilitation, unstable patients with major uncorrectable diseases, nonambulatory patients, or patients at the end stages of a terminal illness.31 However, some patients with impacted stable fractures may be considered for nonsurgical management.32
At initial presentation, the physician should address comorbidities and search for other injuries. When planning for surgery, patients should be assessed for bleeding risk. The presence of two of the following indicates a higher risk of bleeding: peritrochanteric fracture, initial hemoglobin level less than 12 g per dL (120 g per L), and age older than 75 years.33
The timing of surgery may affect the eventual outcome. Early surgery (within 24 to 48 hours) is prudent. This allows earlier mobilization and rehabilitation, which speeds functional recovery and decreases the risk of pneumonia, skin breakdown, deep venous thrombosis, and urinary tract infections.34 Earlier surgery is associated with reduced pain and shorter length of stay in the hospital.34 Patients with comorbidities have an increased risk of mortality; therefore, surgery may need to be delayed until 48 to 72 hours after the fracture to stabilize these conditions.35,36
Some physicians consider the use of traction, either skin or skeletal, before surgery. However, no data suggest a benefit.37 General anesthesia is most common for surgery, although spinal anesthesia may be chosen for some patients. Regional anesthesia may reduce postoperative confusion, yet no evidence suggests a clinically important difference between the two types of anesthesia.38
The consulting orthopedic surgeon determines the most appropriate surgical procedure. For femoral neck fractures, there is debate as to whether open reduction and internal fixation or arthroplasty is the better treatment. Arthroplasty replaces the acetabulum and the head of the femur, whereas hemiarthroplasty replaces only the femoral head. Internal fixation results in lower morbidity, including decreased blood loss and deep wound infection. However, lower reoperation rates have been noted with arthroplasty. Additionally, arthroplasty has a reduced risk of avascular necrosis and nonunion, and allows for earlier recovery.39,40 Intertrochanteric fractures may be treated with open reduction and internal fixation or with arthroplasty. There is insufficient evidence to determine which method is best.40,41
Trochanteric fractures (greater or lesser) are usually isolated avulsion fractures that typically occur in younger, active patients.42 These often heal with conservative, nonoperative management, unless significant displacement (greater than 1 cm) is noted, in which case an orthopedic surgeon should be consulted.43 Patients with nondisplaced fractures should not bear weight for three to four weeks, and are usually able to return to full activity within three to four months.
There is concern about the safety of metal-on-metal implants because of a higher failure rate compared with other bearings. Implants typically last the remainder of patients' lives; however, they have a failure rate of 12% (twice the industry average), resulting in corrective procedures (revision surgery) within five years.44 Recent data suggest that metal-on-metal bearing surfaces were not associated with an increased risk of cancer diagnoses in patients who were followed for seven years postoperatively, but the biologic effects of these metals is not fully known.44,45
Prophylaxis
Patients should receive prophylactic antibiotics within one to two hours before surgery, particularly against Staphylococcus aureus, the major pathogen of concern. Cefazolin, 1 to 2 g intravenously every eight hours, is typically used and recommended within one hour of surgery.46,47 If the patient is allergic, then 1 g of intravenous vancomycin should be administered every 12 hours and started within two hours of surgery. Antibiotics should be provided for 24 hours.48
Patients should receive thromboembolic prophylaxis, preferably with low-molecular-weight heparin, although studies comparing it with unfractionated heparin found no difference in bleeding rates.49 A guideline from the American College of Chest Physicians recommends starting low-molecular-weight heparin 12 hours or more preoperatively or postoperatively, rather than within four hours of surgery, to reduce the risk of bleeding.50 The guideline also recommends extending prophylaxis up to 35 days, rather than 10 to 14 days, to prevent nine additional venous thromboembolic events per 1,000 persons. Aspirin may be used, but is suboptimal and not preferred for protection against thromboembolic events.50
Long-Term Care
Because a previous hip fracture is a risk factor for another hip fracture and because bisphosphonates reduce that risk,22 patients should receive bisphosphonate therapy, regardless of bone mineral density results, unless contraindicated.53 Calcium (1,000 mg per day) and vitamin D (at least 800 IU per day) supplements are usually combined with bisphosphonate therapy. Risks associated with bisphosphonate therapy may increase after five years of use.54 Most patients benefit from a fall-prevention assessment, which includes removing home environmental hazards, reviewing medications, and assessing muscle strength, balance, and gait.55
All patients require rehabilitation therapy after hospital discharge, but the best strategies to improve mobility are not fully known.4,56 The location of the therapy (home, outpatient, or skilled nursing facility) depends on the patient's capabilities and motivation. Outpatient therapy may lead to improved functional status.57 The optimal duration of therapy is unclear. Early ambulation improves patient outcomes and may commence with unrestricted weight bearing. Any nutritional concerns should be addressed. In malnourished patients, protein supplements reduced medical complications.58
Displaced fractures have an increased risk of avascular necrosis.59 Therefore, periodic radiography should be performed following surgery. Depending on the health of the patient, the frequency of imaging should be individualized and discussed with the orthopedic surgeon. If avascular necrosis is suspected, magnetic resonance imaging may be necessary because plain radiography may not show changes for six months after avascular necrosis develops. Long-term care is essential to return the patient to the most functional state as soon as possible, ideally to prefracture level of activity.60
| Recommendation | Sponsoring organization |
|---|---|
| Do not use DEXA to screen for osteoporosis in women younger than 65 years or men younger than 70 years with no risk factors. | American Academy of Family Physicians |
| Do not routinely repeat DEXA scans more often than once every two years. | American College of Rheumatology |
Data Sources: A search of Essential Evidence Plus and the U.S. Preventive Services Task Force was completed for the following keywords: femoral diaphysis fracture, femoral neck fractures, and hip fractures. A literature search of PubMed was completed using the keyword hip fractures (classification, drug therapy, epidemiology, history, mortality, prevention and control, radiography). The search included meta-analyses, randomized controlled trials, clinical trials, and reviews. Search dates: February 19 and 20, 2012, and March 6, 2014.