
This is a corrected version of the article that appeared in print.
Am Fam Physician. 2016;94(3):219-226
Patient information: A handout on this topic is available at https://familydoctor.org/familydoctor/en/diseases-conditions/vision-loss.html.
Author disclosure: No relevant financial affiliations.
Vision loss affects 37 million Americans older than 50 years and one in four who are older than 80 years. The U.S. Preventive Services Task Force concludes that current evidence is insufficient to assess the balance of benefits and harms of screening for impaired visual acuity in adults older than 65 years. However, family physicians play a critical role in identifying persons who are at risk of vision loss, counseling patients, and referring patients for disease-specific treatment. The conditions that cause most cases of vision loss in older patients are age-related macular degeneration, glaucoma, ocular complications of diabetes mellitus, and age-related cataracts. Vitamin supplements can delay the progression of age-related macular degeneration. Intravitreal injection of a vascular endothelial growth factor inhibitor can preserve vision in the neovascular form of macular degeneration. Medicated eye drops reduce intraocular pressure and can delay the progression of vision loss in patients with glaucoma, but adherence to treatment is poor. Laser trabeculoplasty also lowers intraocular pressure and preserves vision in patients with primary open-angle glaucoma, but long-term studies are needed to identify who is most likely to benefit from surgery. Tight glycemic control in adults with diabetes slows the progression of diabetic retinopathy, but must be balanced against the risks of hypoglycemia and death in older adults. Fenofibrate also slows progression of diabetic retinopathy. Panretinal photocoagulation is the mainstay of treatment for diabetic retinopathy, whereas vascular endothelial growth factor inhibitors slow vision loss resulting from diabetic macular edema. Preoperative testing before cataract surgery does not improve outcomes and is not recommended.
Vision loss is common and consequential among older adults.1 Family physicians play a critical role in identifying persons who are at risk of vision loss, counseling patients, and referring patients for disease-specific treatment.
| Recommendation | Sponsoring organization |
|---|---|
| Do not perform preoperative medical tests for eye surgery unless there are specific medical indications. | American Academy of Ophthalmology |
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| The U.S. Preventive Services Task Force concludes that current evidence is insufficient to assess the balance of benefits and harms of screening for impaired visual acuity in older adults. | C | 12 |
| Daily AREDS or AREDS2 vitamin supplementation delays vision loss in patients with age-related macular degeneration. | A | 25, 28–31 |
| Intravitreal injection of a vascular endothelial growth factor inhibitor, such as bevacizumab (Avastin), ranibizumab (Lucentis), or aflibercept (Eylea), stabilizes vision in patients with neovascular age-related macular degeneration or diabetic macular edema. | A | 33, 36, 37, 53, 54 |
| Fenofibrate (Tricor) reduces the progression of diabetic retinopathy. | A | 48, 49 |
| Medical testing before cataract surgery does not improve outcomes and is not recommended. | A | 58, 59 |
| Older adults who smoke should be counseled to quit because of an increased risk of vision loss associated with age-related macular degeneration and cataracts. | C | 60 |
The prevalence of all-cause vision loss increases with age, affecting 37 million Americans older than 50 years and 25% of those older than 80 years (Figure 1).2 Approximately 7% of adults 65 years and older report disability related to impaired vision.3 A 2013 review estimated that the indirect and direct costs of treating adults with visual impairment is $54 billion annually.4 Vision loss in older adults is associated with increased fall risk, loss of independence, depression, and increased all-cause mortality.5–8 Most cases of vision loss in older adults are due to defined diseases for which there are effective strategies to prevent or delay vision loss and blindness.9
Definitions and Legal Issues
Low vision is defined as central visual acuity of 20/70 or worse in the better-seeing eye with best correction or a total visual field loss of 140 degrees. Legal blindness is defined as central visual acuity of 20/200 or worse in the better-seeing eye with best correction or a visual field of 20 degrees or less. Persons with legal blindness may still have adequate vision to maintain activities of daily living and function independently.
Screening
The U.S. Preventive Services Task Force (USPSTF) concludes that current evidence is insufficient to assess the balance of benefits and harms of screening for impaired visual acuity in adults older than 65 years. The USPSTF found no well-designed studies demonstrating conclusive benefits of universal eye screening in older adults.12
Based on expert consensus, the American Academy of Ophthalmology recommends comprehensive eye examinations every one to two years for all adults 65 years and older.13 A comprehensive eye examination includes a visual acuity test, pharmacologic dilation of the pupil, tonometry, and visual field testing.14
Major Causes
The four major causes of severe vision loss and blindness in older adults are age-related macular degeneration (AMD), ocular complications of diabetes mellitus, glaucoma, and age-related cataracts.15
| Disease | Epidemiology15 | Clinical presentation | Screening recommendations |
|---|---|---|---|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Age-Related Macular Degeneration
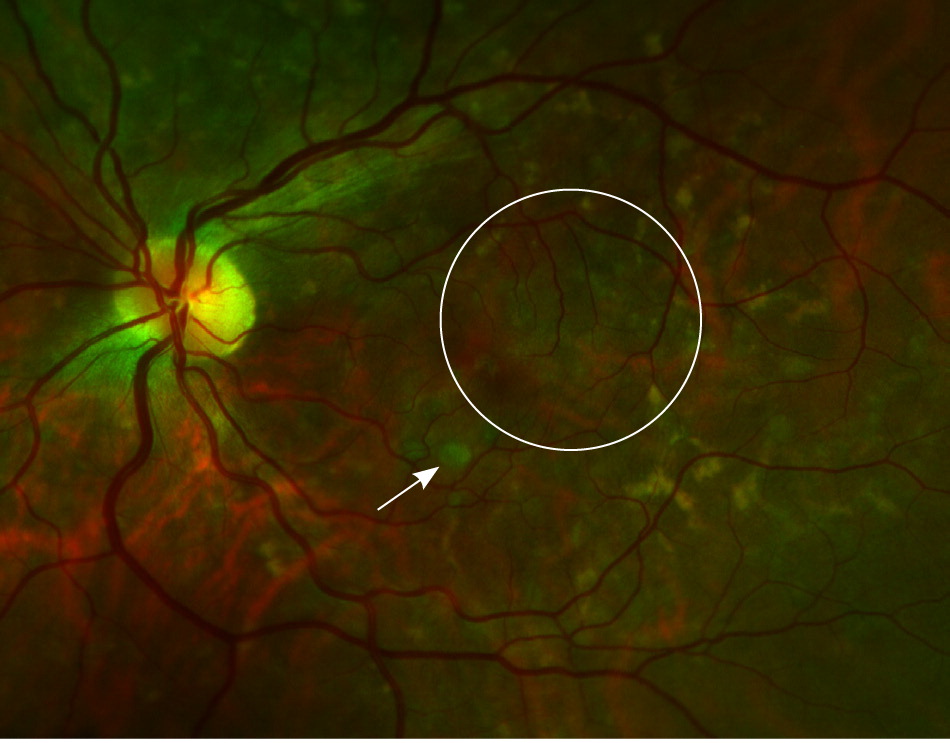
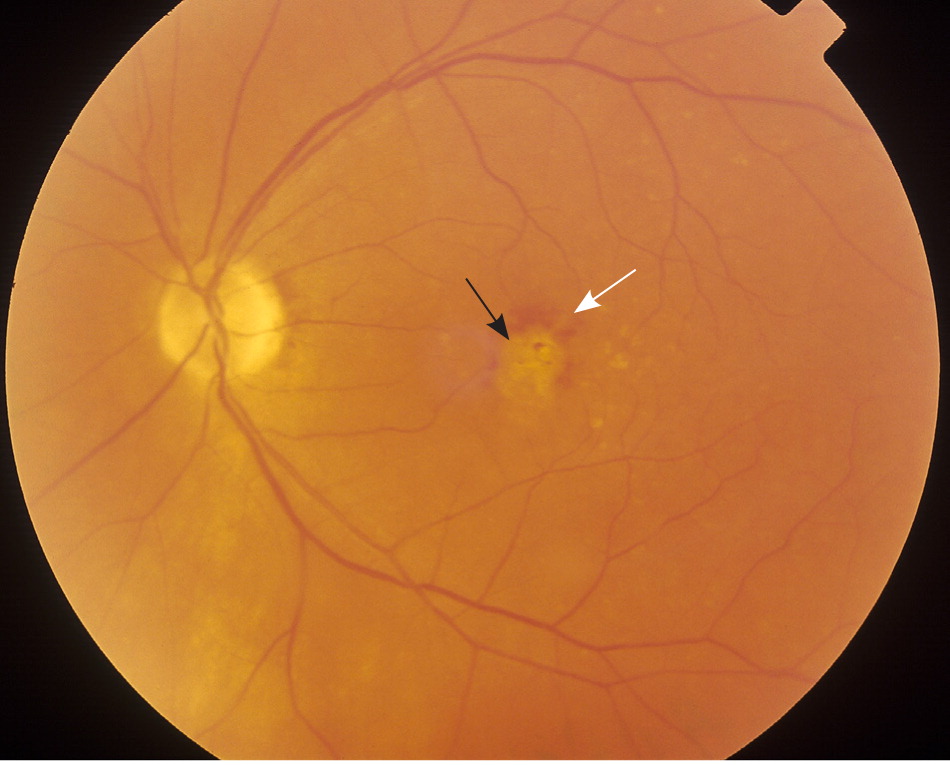
Two retinal pigment abnormalities, retinal geographic atrophy and drusen (yellow deposits under the retina made up of lipids), predominate in dry (nonexudative) AMD (Figure 2). Dry AMD can progress to the more severe wet (exudative or neovascular) type (Figure 3), which is characterized by neovascularization and hemorrhage in the macula. In a long-term follow-up study of patients with AMD, 70.9% of participants with bilateral medium drusen at enrollment progressed to large drusen, and 13.8% progressed to advanced AMD over 10 years.23
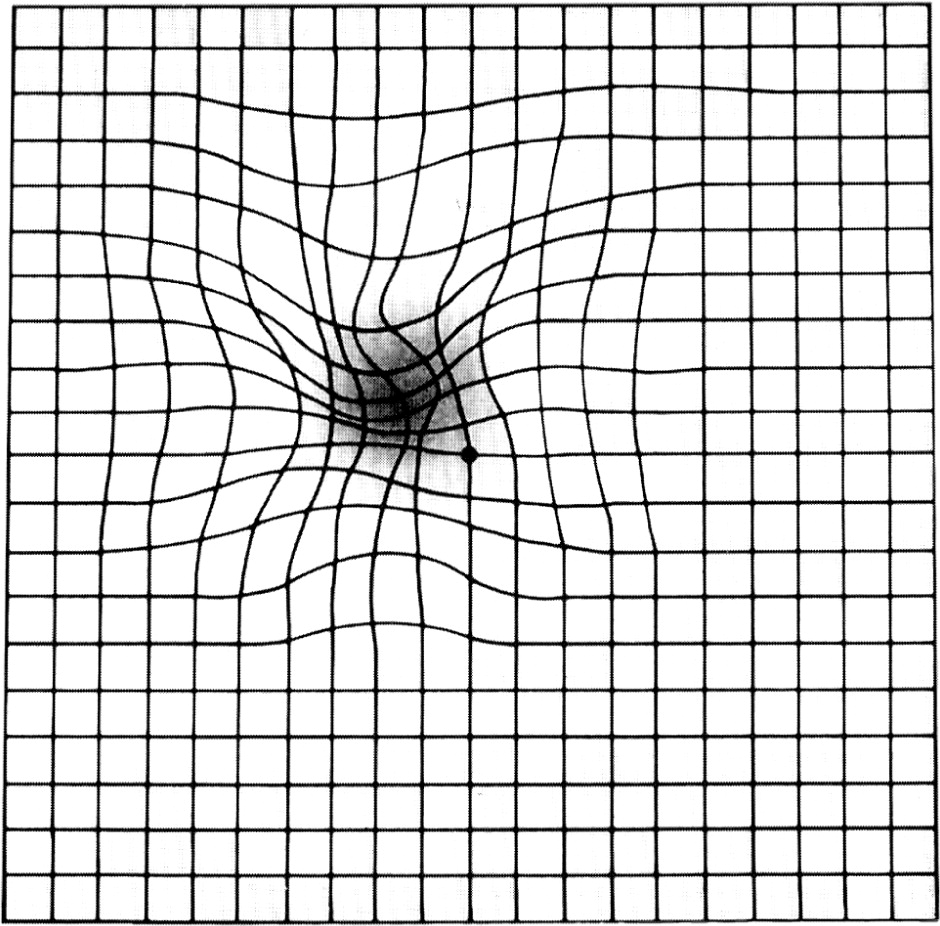
The Amsler grid can be used to identify defects in central vision and monitor visual changes in patients with established AMD. Patients are asked to fix their gaze on the black dot in the center and report whether any grid lines appear to be missing or distorted, indicating an abnormality (Figure 424 ). New or worsening abnormalities warrant referral to an ophthalmologist.
TREATMENT
Vitamin Supplements. The Age-Related Eye Disease Study (AREDS) is a randomized controlled trial that tested the effectiveness of an antioxidant vitamin supplement in 3,640 patients with AMD who were 55 to 80 years of age.25 Patients in the active treatment arm who had moderate to severe AMD at enrollment had a lower risk of disease progression compared with those receiving placebo over 6.3 years of follow-up (26.7% vs. 35.7%; number needed to treat = 11).25,26 Supplements do not prevent the development of AMD.25,27
Because beta-carotene supplements were subsequently associated with increased lung cancer rates in patients who smoke tobacco, a second trial (AREDS2) randomized participants to a revised supplement containing lutein plus zeaxanthin, omega-3 fatty acids, or both.28–31 Removal of beta-carotene had no effect on AMD progression.29 Omega-3 fatty acid supplementation offered no benefit beyond the original AREDS formulation.29 Lutein plus zeaxanthin appeared to offer no additional benefit in the general study population.29 Secondary analysis of the subgroup with large drusen at enrollment, however, suggested that lutein plus zeaxanthin may provide modest additional benefit in preventing progression to advanced AMD (hazard ratio = 0.76; 95% confidence interval, 0.61 to 0.96) and development of neovascular AMD (hazard ratio = 0.65; 95% confidence interval, 0.49 to 0.85).30,31 Lutein plus zeaxanthin also appears to be safe, with no increased risk of lung cancer.30
| AREDS supplements | AREDS2 supplements | ||
|---|---|---|---|
| 500 mg vitamin C | 500 mg vitamin C | ||
| 400 IU vitamin E | 400 IU vitamin E | ||
| 15 mg beta-carotene* | 25 mg zinc | ||
| 80 mg zinc as zinc oxide | 2 mg copper as cupric oxide | ||
| 2 mg copper as cupric oxide | 10 mg lutein plus 2 mg zeaxanthin | ||
Vascular Endothelial Growth Factor Inhibitors. The use of vascular endothelial growth factor inhibitors by intravitreal injection is a major advancement in the treatment of neovascular AMD.33 Injections are administered once monthly for four months or until vision stabilizes, then every three months thereafter. The safety and effectiveness of this intervention have not been evaluated past 24 months.
Ranibizumab (Lucentis) and bevacizumab (Avastin) appear to be slightly more effective than pegaptanib (Macugen), with similar adverse effect and safety profiles.33 Pegaptanib, ranibizumab, and aflibercept (Eylea) are approved by the U.S. Food and Drug Administration (FDA) for the treatment of neovascular AMD. Bevacizumab has to be compounded for intravitreal injection and is not FDA approved for AMD treatment. The cost of bevacizumab is significantly lower per dose than other, FDA-approved agents (approximately $150 vs. $1,500 to $2,000). Many ophthalmologists favor using the less-expensive bevacizumab instead of ranibizumab, citing comparable safety and effectiveness; however, the manufacturer, which produces both drugs, has not sought FDA approval for bevacizumab.34
Glaucoma
CLASSIFICATION AND DIAGNOSIS
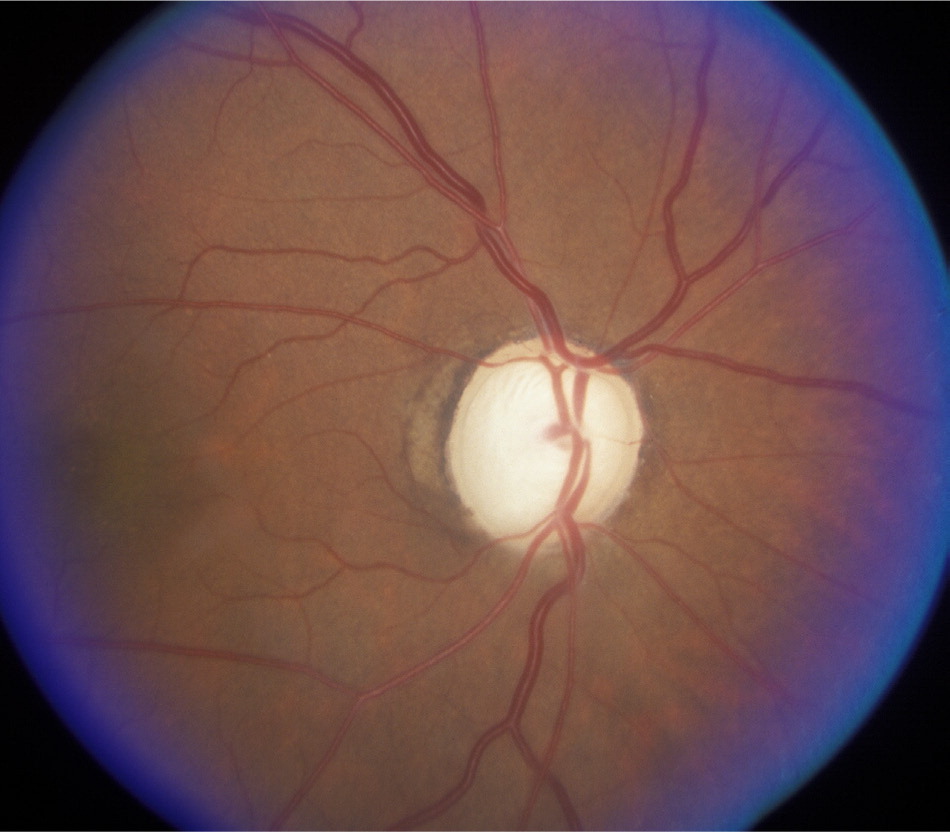
Glaucoma is a heterogeneous group of ophthalmic conditions that cause progressive damage to the optic nerve, leading to visual field loss and irreversible blindness (Figure 5). Primary open-angle glaucoma and primary angle-closure glaucoma are the most common forms. Most patients with glaucoma have ocular hypertension (elevated intraocular pressure), but optic nerve damage can also occur with normal intraocular pressure.38 Diagnosis requires measurement of intraocular pressure in conjunction with evaluation of the optic disc and an automated visual field test.18,38
SCREENING AND PREVENTION
The USPSTF found insufficient evidence to assess the balance of benefits and harms of screening for primary open-angle glaucoma, but recognizes that certain subpopulations (e.g., persons with a family history of glaucoma, blacks, Hispanics) are at higher risk of the disease and may be more likely to benefit from referral for periodic intraocular pressure measurement and automated visual field testing.18
TREATMENT
A number of medicated eye drops lower intraocular pressure and can delay the progression of vision loss.1,39 Long-term adherence to therapy remains a major problem; continuation rates are typically less than 50% at one year.40 Simplifying eye drop regimens, providing patient education, coaching on proper eye drop technique, and offering ongoing support to patients may improve adherence.41
Because adherence to medical therapy for glaucoma is poor, there is interest in surgical approaches to stop progression of glaucoma before vision loss becomes irreversible. Laser trabeculoplasty for primary open-angle glaucoma appears to be safe and effective in lowering intraocular pressure and preserving vision.42 Long-term studies are needed to identify which patients are most likely to benefit from surgery, the optimal technique, and the effectiveness of repeat procedures.
Diabetic Eye Disease
SCREENING AND MONITORING
Older adults with type 2 diabetes should be referred to an ophthalmologist at diagnosis for dilated eye examination, and reexamined at least annually.17 It is reasonable to discontinue these examinations in older adults with no or mild diabetic eye disease and life-limiting conditions (e.g., end-stage renal disease).
SLOWING DISEASE PROGRESSION
Glycemic Control. Several large clinical trials have demonstrated that tight glycemic control decreases the risk of progression of diabetic retinopathy.43–45 It is unclear how these results apply to the care of older adults with diabetes, who often have multiple comorbidities that complicate diabetes management and are at risk of hypoglycemia and increased all-cause mortality with tight glycemic control.46,47 The American Diabetes Association revised consensus guidelines recommend individualized adjustment of A1C goals (target range of 8.5%) in older adults.43
TREATMENT OF PROGRESSIVE DIABETIC RETINOPATHY
Photocoagulation. Nonproliferative diabetic retinopathy with preserved visual acuity can be monitored without active treatment. Widespread neovascularization and hemorrhage indicate progression to proliferative diabetic retinopathy (Figure 6), which requires treatment, typically with panretinal photocoagulation.50 [corrected]

Vascular endothelial growth factor inhibitors. Based on low-quality evidence, a Cochrane review concluded that vascular endothelial growth factor inhibitors have limited effectiveness for proliferative diabetic retinopathy.51 However, they may have a role if standard therapy is ineffective or vitreous hemorrhage occurs.52
TREATMENT OF DIABETIC MACULAR EDEMA
Diabetic macular edema causes rapid vision deterioration and can quickly lead to blindness. Aflibercept, bevacizumab, and ranibizumab have been studied for diabetic macular edema with comparable effectiveness, adverse effects, and safety profiles.53,54 Aflibercept and ranibizumab were approved by the FDA for the treatment of diabetic macular edema in 2015. Bevacizumab is not approved for use in diabetic macular edema. Patients who are treated with any of these agents demonstrate significantly better vision (a gain of three or more lines of vision on the Snellen chart) than individuals treated with laser photocoagulation. Aflibercept may offer a slight advantage in more advanced cases of diabetic macular edema.53
Intravitreal administration of corticosteroids, either by injection or implant, is another treatment option. A Cochrane review found that this therapy had a beneficial effect in stopping the progression of diabetic macular edema, but led to greater risk of increased intraocular pressure and cataract formation.55
Age-Related Cataracts
DIAGNOSIS
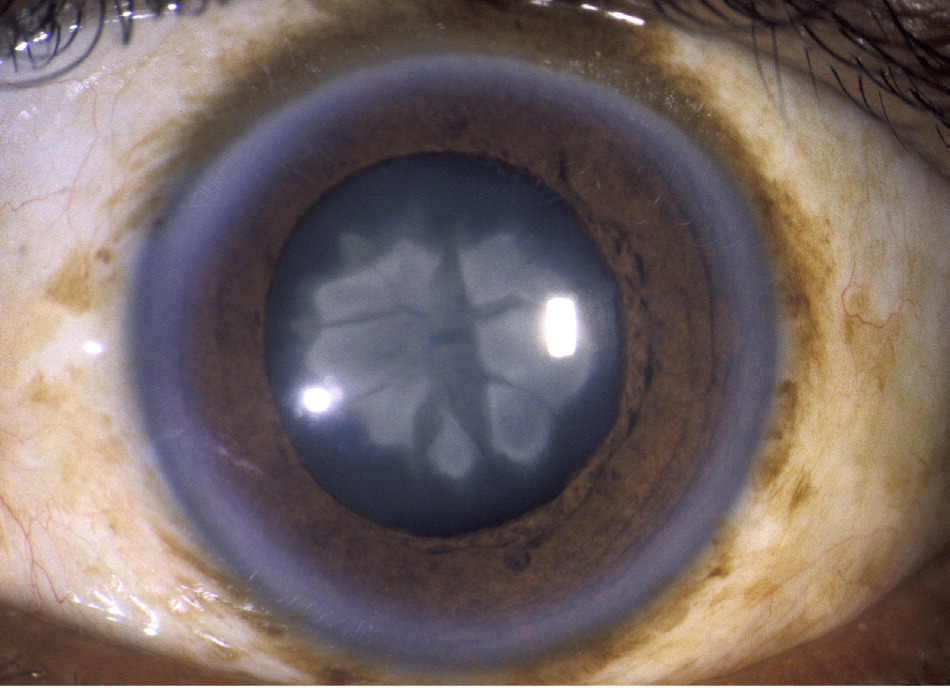
Cataracts can be readily detected with a handheld ophthalmoscope. The red reflex appears dull, extinct, or shady in a patient with cataracts (Figure 7). Treatment is not needed for cataracts that do not cause significant visual impairment. Impaired vision, glare sensitivity, or difficulty with nighttime vision (especially when driving) warrants referral to an ophthalmologist.
TREATMENT
Surgery is the only effective treatment for a cataract that compromises vision. Phacoemulsification with intraocular lens replacement is the standard surgical approach in the United States.56
Immediate sequential cataract surgery (surgery on both eyes during the same visit) has been researched for its cost-saving potential vs. the more common delayed sequential cataract surgery. A study of Medicare beneficiaries in west Tennessee projected that Medicare would save $522 million per year nationally if immediate sequential cataract surgery were widely adopted.57
PREVENTION
Ultraviolet light exposure and smoking are associated with accelerated cataract formation.60,61 It is reasonable to counsel older patients to reduce their exposure to ultraviolet light when feasible and to stop smoking. Smoking is also linked to an increased risk of vision loss associated with age-related macular degeneration.61 Supplements such as those used in the AREDS do not prevent or slow the progression of cataracts.62
Data Sources: Searches were performed in Pub Med, Healthy People 2020 Structured Evidence Queries (Vision), Essential Evidence Plus, National Guideline Clearinghouse, U.S. Preventive Services Task Force recommendations, Cochrane Database of Systematic Reviews, and the website of the National Eye Institute of the National Institutes of Health. Search terms included eye disease, eye disease in older adults, vision loss, low vision, blindness, and disease-specific terms, including age-related macular degeneration, diabetic eye disease, diabetic retinopathy, glaucoma, ocular hypertension, and age-related cataracts. Search dates: October 2015, December 2015, and May 2016.
Figures 2,3,5,6, and 7 courtesy of Mike Stanley, Department of Ophthalmology, Augusta University.