
Am Fam Physician. 2016;94(9):723-726
Patient information: See related handout on epididymitis, written by the authors of this article.
Author disclosure: No relevant financial affiliations.
Inflammation of the epididymis, or epididymitis, is commonly seen in the outpatient setting. Etiology and treatment are based on patient age and the likely causative organisms. Epididymitis presents as the gradual onset of posterior scrotal pain that may be accompanied by urinary symptoms such as dysuria and urinary frequency. Physical findings include a swollen and tender epididymis with the testis in an anatomically normal position. Although the etiology is largely unknown, reflux of urine into the ejaculatory ducts is considered the most common cause of epididymitis in children younger than 14 years. Neisseria gonorrhoeae and Chlamydia trachomatis are the most common pathogens in sexually active males 14 to 35 years of age, and a single intramuscular dose of ceftriaxone with 10 days of oral doxycycline is the treatment of choice in this age group. In men who practice insertive anal intercourse, an enteric organism is also likely, and ceftriaxone with 10 days of oral levofloxacin or ofloxacin is the recommended treatment regimen. In men older than 35 years, epididymitis is usually caused by enteric bacteria transported by reflux of urine into the ejaculatory ducts secondary to bladder outlet obstruction; levofloxacin or ofloxacin alone is sufficient to treat these infections. Because untreated acute epididymitis can lead to infertility and chronic scrotal pain, recognition and therapy are vital to reduce patient morbidity.
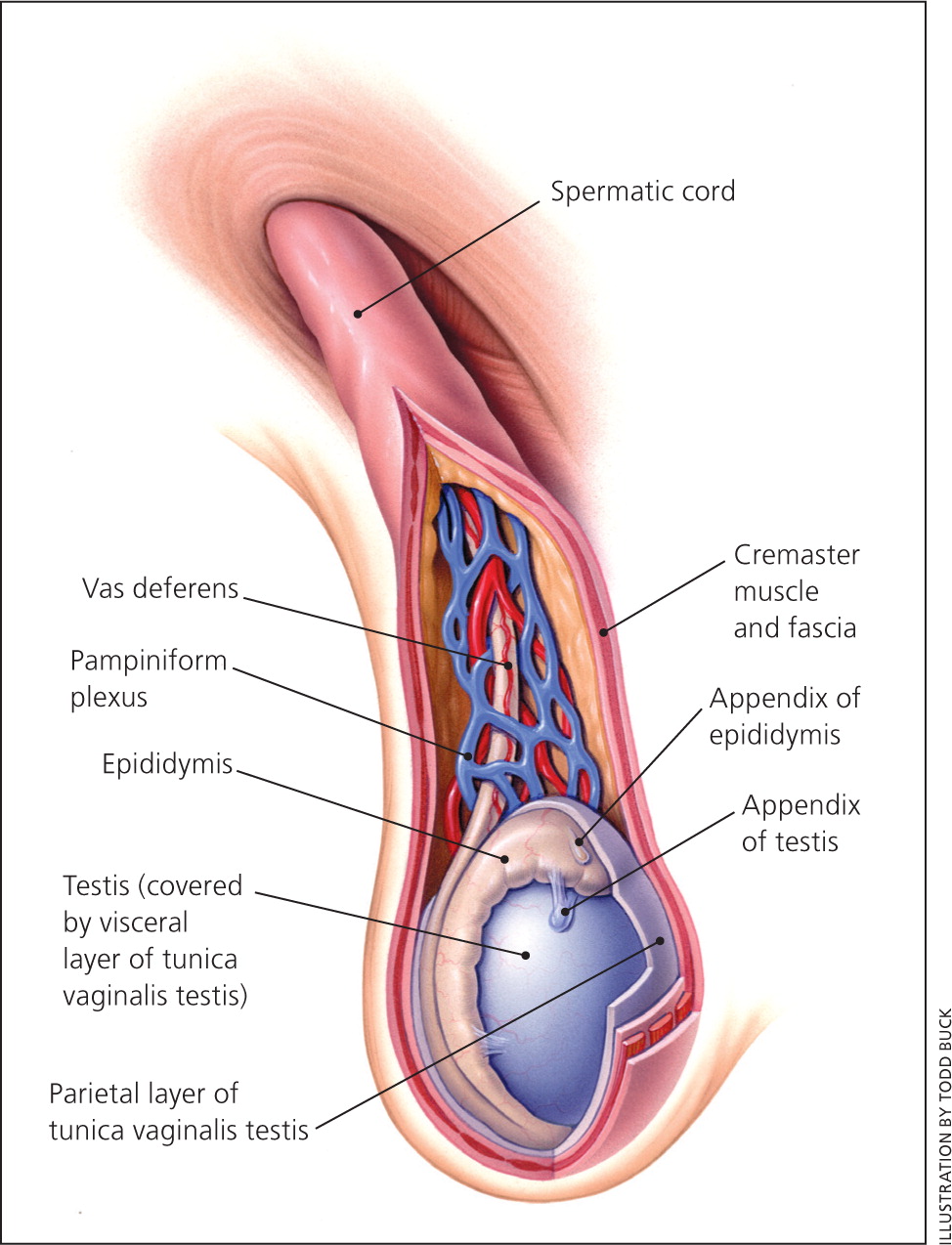
Epididymitis (inflammation of the epididymis) can affect children and adults and is commonly seen in the outpatient setting. Epididymitis often occurs with orchitis (inflammation of the testis); this is referred to as epididymo-orchitis.1 Figure 1 illustrates normal scrotal anatomy.2 In acute epididymitis, pain and scrotal swelling are present for less than six weeks. Chronic epididymitis lasts longer than three months and is usually characterized by pain in the absence of scrotal swelling.3
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| If acute epididymitis is thought to be due to gonorrhea or chlamydia, intramuscular ceftriaxone (single 250-mg dose) plus oral doxycycline (100 mg twice daily for 10 days) is the recommended treatment regimen. | C | 1 |
| In men with epididymitis who practice insertive anal intercourse, an enteric organism is likely in addition to gonorrhea or chlamydia; intramuscular ceftriaxone (single 250-mg dose) plus either oral levofloxacin (Levaquin; 500 mg once daily for 10 days) or ofloxacin (300 mg twice daily for 10 days) is the recommended treatment regimen. | C | 1 |
| In men older than 35 years with epididymitis, sexually transmitted infections are less likely, and monotherapy with levofloxacin or ofloxacin is the empiric regimen of choice. | C | 1 |
Epidemiology
The annual incidence of acute epididymitis is approximately 1.2 per 1,000 boys two to 13 years of age (mean age = 11 years)4,5; about one-fourth of this group has recurrence within five years.5 Among adult men, 43% of epididymitis cases occur between 20 and 30 years of age.4,6 In one series, epididymitis occurred with orchitis in 58% of patients.7
Etiology and Pathophysiology
Acute epididymitis generally presents as unilateral pain and inflammation in the scrotum. Etiology is highly dependent on age. In boys younger than 14 years, the cause is largely unknown but may be related to anatomic abnormalities causing reflux of infected or sterile urine into the ejaculatory ducts.5 Epididymitis in this age group may also be part of a postinfectious syndrome, mainly from Mycoplasma pneumoniae, enteroviruses, and adenoviruses.4 Henoch-Schönlein purpura may present as an acute scrotum and bilateral vasculitic epididymitis in children two to 11 years of age.6
Chlamydia trachomatis and Neisseria gonorrhoeae are the most common etiologies in sexually active males 14 to 35 years of age.1 In those older than 35 years, acute epididymitis is most commonly caused by the retrograde flow of infected urine (bacteriuria) into the ejaculatory duct in the setting of bladder outlet obstruction, usually secondary to prostatic hypertrophy.6 Enteric bacteria must be considered in men who practice insertive anal intercourse, regardless of age.1 In patients with human immunodeficiency virus infection, epididymitis may be caused by concomitant infections, such as from Cytomegalovirus, Salmonella, toxoplasmosis, Ureaplasma urealyticum, Corynebacterium, Mycoplasma, and mycobacteria.1 Noninfectious acute epididymitis may be an adverse reaction to a medication or caused by reflux of sterile urine into the vas deferens because of bladder outlet obstruction or an underlying systemic disease (e.g., sarcoidosis, Behçet syndrome).1,6,9
Diagnosis
HISTORY AND PHYSICAL EXAMINATION
Acute epididymitis generally presents as the gradual onset of posterior scrotal pain and swelling over one to two days. There may be concurrent symptoms of fever, hematuria, dysuria, and urinary frequency, and the pain may radiate into the lower abdomen. In contrast, torsion of the testis or appendix testis (vestigial tissue along the testis) presents as the sudden onset of severe unilateral pain, often associated with nausea and vomiting but without fever or other urologic symptoms. A history of intermittent scrotal pain is uncommon in epididymitis or torsion of the testicular appendages but may occur with intermittent testicular torsion.3,10
Physical examination findings in patients with epididymitis include tenderness of the epididymis that may extend to the adjacent testis and swelling or inflammation of the scrotum. Elevating the scrotum may alleviate the pain (Prehn sign).
In contrast to acute epididymitis with an anatomically normal testis, testicular torsion classically presents as a high-riding testis on one side that may lie transversely in the scrotum with an anteriorly located epididymis. An absent cremasteric reflex is suggestive of testicular torsion (odds ratio = 7.8), whereas the reflex is preserved with epididymitis.10–12 Torsion of the appendix testis is classically associated with a blue-dot sign (i.e., bluish discoloration in the scrotal area directly over the torsed appendage), indicating infarction or necrosis.3,11
It is important to consider an inguinal hernia because it may also present as a swollen, tender scrotum. With an inguinal hernia, bowel sounds may be auscultated within the scrotum. Testicular cancer and trauma may also cause scrotal pain. Table 1 includes the selected differential diagnosis of acute scrotal pain.3,13–15
| Diagnosis | Typical presentation | Examination findings | Ultrasound findings |
|---|---|---|---|
| Epididymitis | Gradual onset of posterior scrotal pain and swelling over one to two days | Scrotal swelling or inflammation and tenderness of the epididymis; positive Prehn sign (pain alleviated by lifting the scrotum); normal cremasteric reflex | Hyperemia, swelling, and increased blood flow of the epididymis on color Doppler |
| Testicular cancer | Up to 15% of cases are associated with pain | Firm, unilateral nodule arising from the testis that may be tender | Distinct mass involving the testis on color Doppler |
| Testicular torsion | Sudden onset of severe unilateral scrotal pain | High-riding testis, absent cremasteric reflex, increased pain with elevation of scrotum | Decreased or absent blood flow on color Doppler |
| Torsion of appendix testis | Sudden onset of scrotal pain | Blue-dot sign (bluish discoloration in the scrotal area directly over the torsed appendage), indicating infarction or necrosis | Appendage larger than 5 mm, spherical shape, or increased periappendiceal blood flow on color Doppler |
DIAGNOSTIC TESTING
Acute epididymitis is a clinical diagnosis. A midstream urinalysis should be obtained to evaluate for an infectious cause. A urine culture should be obtained for all children, and for adults with a positive urinalysis result.6,16 For sexually active patients younger than 35 years or who have a new sex partner, nucleic acid amplification testing for N. gonorrhoeae and C. trachomatis should be performed.1
If testicular torsion is suspected, color Doppler ultrasonography should be ordered immediately. Hyperemia, swelling, and increased blood flow of the epididymis are common ultrasound findings in patients with epididymitis, whereas there is decreased or absent flow in those with testicular torsion.14
If color Doppler ultrasonography is not readily available, measurement of acute phase reactants may be helpful in differentiating between epididymitis and testicular torsion. Epididymitis is often associated with an elevated C-reactive protein level.13
Treatment
In children two to 14 years of age without systemic signs (e.g., fever), antibiotics may be reserved for when urinalysis or urine culture results are positive.16 In patients 14 years and older, empiric antibiotics are recommended based on the most likely causative organism. Goals of treatment include curing microbiologic infection; preventing the spread of N. gonorrhoeae or C. trachomatis infection to sex partners; and preventing complications from untreated epididymitis, including infertility and chronic pain.1
To prevent complications and the spread of gonorrhea and chlamydia, the Centers for Disease Control and Prevention recommends beginning treatment before all laboratory test results are available, and basing therapy choice on the risk of chlamydia and gonorrhea or enteric organisms.1 In settings where gonorrhea or chlamydia is likely, intramuscular ceftriaxone (single 250-mg dose) plus oral doxycycline (100 mg twice daily for 10 days) is the recommended regimen. In men who practice insertive anal intercourse, an enteric organism is likely in addition to gonorrhea or chlamydia; intramuscular ceftriaxone (single 250-mg dose) plus either oral levofloxacin (Levaquin; 500 mg once daily for 10 days) or oral ofloxacin (300 mg twice daily for 10 days) is the recommended treatment regimen for these patients. In patients older than 35 years, sexually transmitted infections are less likely, and monotherapy with levofloxacin or ofloxacin is sufficient to treat the likely enteric organisms. Because of increased chlamydia resistance, ciprofloxacin is no longer an adequate alternative fluoroquinolone for treatment of epididymitis. Table 2 summarizes antibiotic therapy for acute epididymitis.1
| Population | Most likely causative agent | Antibiotic treatment | |
|---|---|---|---|
| Children younger than 2 years | Various | Antibiotic treatment for likely underlying enteric organism and referral to a urologist | |
| Children 2 to 14 years of age | Various, likely anatomic | Treat based on urinalysis or urine culture results | |
| Sexually active adults younger than 35 years | Gonorrhea or chlamydia | Intramuscular ceftriaxone (single 250-mg dose) | |
| and | |||
| Oral doxycycline (100 mg twice daily for 10 days) | |||
| Adults who practice insertive anal intercourse | Gonorrhea or chlamydia and an enteric organism | Intramuscular ceftriaxone (single 250-mg dose) | |
| and | |||
| Oral levofloxacin (Levaquin; 500 mg once daily for 10 days) or oral ofloxacin (300 mg twice daily for 10 days) | |||
| Adults older than 35 years or who have had recent urinary tract surgery or instrumentation | Enteric organism | Oral levofloxacin (500 mg once daily for 10 days) | |
| or | |||
| Oral ofloxacin (300 mg twice daily for 10 days) | |||
Initial treatment of idiopathic chronic epididymitis includes a two-week course of nonsteroidal anti-inflammatory drugs with scrotal icing and elevation. If symptoms do not improve, adding a tricyclic antidepressant or neuroleptic such as gabapentin (Neurontin) may be helpful. As with most chronic pain syndromes, treatment of chronic epididymitis will likely require a combination of modalities individualized to the patient.6
Follow-up
Acute epididymitis can usually be treated in the outpatient setting with follow-up within one week to evaluate for clinical response to treatment. Rarely, inpatient hospitalization and intravenous antibiotics are required for systemic symptoms, abscess formation, or Fournier gangrene.8,17 Epididymitis improves within two to three days of antibiotic treatment, but residual pain may persist for several weeks.1,3 Children younger than 14 years who are treated for acute epididymitis should be referred to a urologist to evaluate for possible anatomic abnormalities.6 Men older than 50 years should be evaluated for urinary tract obstruction due to prostatic enlargement. All patients treated for a sexually transmitted infection should instruct their partners to also be treated.1,3
Data Sources: We searched the Agency for Healthcare Research and Quality evidence reports, Cochrane Database of Systematic Reviews, National Guideline Clearinghouse, Essential Evidence Plus, and PubMed clinical queries. Key words were epididymitis, orchitis, and epididymo-orchitis. Search dates: October 18, 2015; November 11, 2015; and April 2016.
