
Am Fam Physician. 2017;96(6):371-378
Patient information: See related handout on hair loss.
Author disclosure: No relevant financial affiliations.
Hair loss is often distressing and can have a significant effect on the patient's quality of life. Patients may present to their family physician first with diffuse or patchy hair loss. Scarring alopecia is best evaluated by a dermatologist. Nonscarring alopecias can be readily diagnosed and treated in the family physician's office. Androgenetic alopecia can be diagnosed clinically and treated with minoxidil. Alopecia areata is diagnosed by typical patches of hair loss and is self-limited. Tinea capitis causes patches of alopecia that may be erythematous and scaly and must be treated systemically. Telogen effluvium is a nonscarring, noninflammatory alopecia of relatively sudden onset caused by physiologic or emotional stress. Once the precipitating cause is removed, the hair typically will regrow. Trichotillomania is an impulse-control disorder; treatment is aimed at controlling the underlying psychiatric condition. Trichorrhexis nodosa occurs when hairs break secondary to trauma and is often a result of hair styling or overuse of hair products. Anagen effluvium is the abnormal diffuse loss of hair during the growth phase caused by an event that impairs the mitotic activity of the hair follicle, most commonly chemotherapy. Physician support is especially important for patients in this situation.
Patients with hair loss will often consult their family physician first. Hair loss is not life threatening, but it is distressing and significantly affects the patient's quality of life. The pattern of hair loss may be obvious, such as the bald patches that occur in alopecia areata, or more subtle, such as the diffuse hair loss that occurs in telogen effluvium. As with most conditions, the physician should begin the evaluation with a detailed history and physical examination. It is helpful to determine whether the hair loss is nonscarring (also called noncicatricial), which is reversible, or scarring (also called cicatricial), which is permanent. Scarring alopecia is rare and has various etiologies, including autoimmune diseases such as discoid lupus erythematosus. If the follicular orifices are absent, the alopecia is probably scarring; these patients should be referred to a dermatologist. This article will discuss approaches to nonscarring causes of alopecia.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Topical minoxidil is safe and effective for the treatment of androgenetic alopecia in women. | B | 5 |
| Alopecia areata can be treated with intralesional corticosteroids. | B | 11 |
| Oral terbinafine (Lamisil), itraconazole (Sporanox), fluconazole (Diflucan), or griseofulvin is recommended for treatment of children with tinea capitis caused by Trichophyton infections. | B | 2 |
| Cognitive behavior therapy is effective for the treatment of trichotillomania, and medical therapy may be more effective when combined with cognitive behavior therapy. | B | 19 |
Physiology of Hair Growth
Hair grows in three phases: anagen (active growing, about 90 % of hairs), catagen (degeneration, less than 10% of hairs) and telogen (resting, 5% to 10% of hairs). Hair is shed during the telogen phase.
Approach to the Patient with Nonscarring Alopecia
The history and physical examination are often sufficient to determine a specific etiology for hair loss. It is convenient to divide the various causes into focal (patchy) and diffuse etiologies, and proceed accordingly. Patchy hair loss is often due to alopecia areata, tinea capitis, and trichotillomania. Diffuse hair loss is commonly due to telogen or anagen effluvium. Androgenetic alopecia may be diffuse or in a specific pattern, and may progress to complete baldness.
HISTORY
Important clues to the etiology of different patterns and types of hair loss are listed in Table 1 and Table 2. Hair that comes out in clumps suggests telogen effluvium. Systemic symptoms such as fatigue and weight gain suggest hypothyroidism, whereas a febrile illness, stressful event, or recent pregnancy may account for the diffuse hair loss of telogen effluvium. The use of hair products such as straightening agents or certain shampoos suggests a diagnosis of trichorrhexis nodosa. A family history of hypothyroidism may warrant laboratory testing for this condition, whereas a family history of hair loss supports the diagnosis of androgenetic alopecia.
| Type | Significant features | Treatment and comments |
|---|---|---|
| Alopecia areata | Acute, patchy hair loss; examination shows short, vellus hairs, yellow or black dots, and broken hair shafts | Intralesional triamcinolone acetonide injected intradermally |
| High rate of spontaneous remission | ||
| Anagen effluvium | Diffuse hair loss days to weeks after exposure to a chemotherapeutic agent; incidence after chemotherapy is estimated at 65% | No pharmacologic intervention has been proven effective; scalp cooling not recommended |
| Minoxidil may help during regrowth period | ||
| Androgenetic alopecia | Family history of hair loss; gradually progressive course | Men: topical minoxidil (2% or 5% solution) |
| Men: bitemporal thinning of the frontal and vertex scalp, complete hair loss with some hair at the occiput and temporal fringes | Women: topical minoxidil (2% solution) | |
| Women: diffuse hair thinning of the vertex with sparing of the frontal hairline | Treatment should continue indefinitely because hair loss reoccurs when treatment is discontinued | |
| Adverse effects include hypertrichosis (excessive hair growth for age, sex, and race) and irritant or contact dermatitis | ||
| Telogen effluvium | Clumps of hair come out in the shower or in hairbrush; associated with physiologic or emotional stress | Treatment involves removing the underlying cause and providing reassurance |
| Condition is usually self-limited and resolves within two to six months | ||
| Tinea capitis | Dermatophyte infection of the hair shaft and follicles; patients present with patchy alopecia with or without scaling | Requires systemic treatment because topical antifungals do not penetrate hair follicles |
| Trichophyton species: oral terbinafine (Lamisil), itraconazole (Sporanox), fluconazole (Diflucan), or griseofulvin | ||
| Microsporum species: griseofulvin | ||
| Trichorrhexis nodosa | Hairs break secondary to trauma or because of fragile hair (congenital or genetic); causative traumas include excessive brushing, heat application, hairstyles that pull on hairs, and conditions that cause excessive scalp scratching | Stop offending actions |
| Trichotillomania | Patches of alopecia, typically frontoparietal, that progress backward and may include the eyelashes and eyebrows | Optimal treatment is unknown; strong evidence is lacking for selective serotonin reuptake inhibitors; cognitive behavior therapy with habit reversal and medications may be more effective than either approach alone |
| Psychiatric referral may be indicated |
| Common findings | Related diagnosis | Diagnostic workup and comments |
|---|---|---|
| Abrupt onset of hair loss | Telogen effluvium related to a specific event | Inquire about inciting event |
| Gradual onset of hair loss | Alopecia areata | History and physical examination findings are diagnostic |
| Pull test: increased telogen-to-anagen ratio (greater than the normal ratio of 1:10) | ||
| Androgenetic alopecia | Family history and specific patterns are important | |
| Scarring alopecias | Refer if scarring is suspected | |
| Diffuse hair loss | Alopecia totalis if more than scalp is involved | Consider referral |
| Systemic disease (e.g., hypothyroidism, iron deficiency, other nutritional disorder) | Laboratory testing depends on history and physical examination findings: complete blood count, thyroid-stimulating hormone level | |
| Telogen effluvium | History and physical examination findings are diagnostic | |
| Patchy hair loss | Alopecia areata, trichotillomania | History and physical examination findings are diagnostic |
| Tinea capitis | Obtain fungal cultures; itching, scaling, pustules, and lymphadenopathy may be present | |
| Male or female pattern | Androgenetic alopecia | History and physical examination findings are diagnostic; scalp appears normal |
| History of anxiety or psychiatric diseases | Trichotillomania | Obtain psychiatric history; patient may not be forthcoming about pulling hair; pattern and appearance of hair are diagnostic |
| History of extensive use of hair products or tight hairstyles | Trichorrhexis nodosa | History and physical examination findings are diagnostic; broken hairs seen on slight magnification |
| Medication use | Several types of hair loss, especially telogen effluvium | If a particular medicine is suspected, a discontinuation trial is reasonable |
| Recent physical or emotional trauma | Telogen effluvium | History and physical examination findings are diagnostic; scalp appears normal; hair loss may not be obvious |
| Skin condition | Scarring alopecia, tinea capitis; most nonscarring alopecias are associated with a relatively normal scalp | History and physical examination findings are diagnostic |
| Systemic symptoms | Related to systemic disease | Laboratory testing depends on history and physical examination findings |
PHYSICAL EXAMINATION
The physical examination should focus on the hair and scalp, but attention should be given to physical signs of any comorbid disease indicated by the review of systems. If only the scalp is involved, the physician should look for typical male or female pattern to determine the presence of androgenetic alopecia. Whole body hair loss is consistent with alopecia totalis. Dry, broken hair suggests trichorrhexis nodosa, whereas scaling, pustules, crusts, erosions, or erythema and local adenopathy suggest infection.
The pull test may be used to diagnose hair loss conditions.1 The examiner grasps approximately 40 to 60 hairs at their base using the thumb, index, and middle fingers and applies gentle traction away from the scalp. A positive result is when more than 10% of hairs (four to six) are pulled from the scalp; this implies active hair shedding and suggests a diagnosis of telogen effluvium, anagen effluvium, or alopecia areata. However, a negative test result does not necessarily exclude those conditions. The pull test is difficult to standardize because the pulling force is not distributed uniformly and because it is difficult to approximate the number of hairs grasped, thereby leading to false interpretations.
LABORATORY STUDIES
Because many conditions can cause hair loss, there are no routine tests to evaluate hair loss. Laboratory testing is indicated when the history or physical examination findings suggest an underlying comorbidity.
Specific Disorders
ANDROGENETIC ALOPECIA
Androgenetic alopecia is the most common form of hair loss in men and women and is a normal physiologic variant. It is most prevalent in white men, with 30%, 40%, and 50% experiencing androgenetic alopecia at 30, 40, and 50 years of age, respectively 2 (Figure 1). Although this condition is less common in women, 38% of women older than 70 years may be affected3 (Figure 24 ). Many patients with androgenetic alopecia have a family history of this condition.
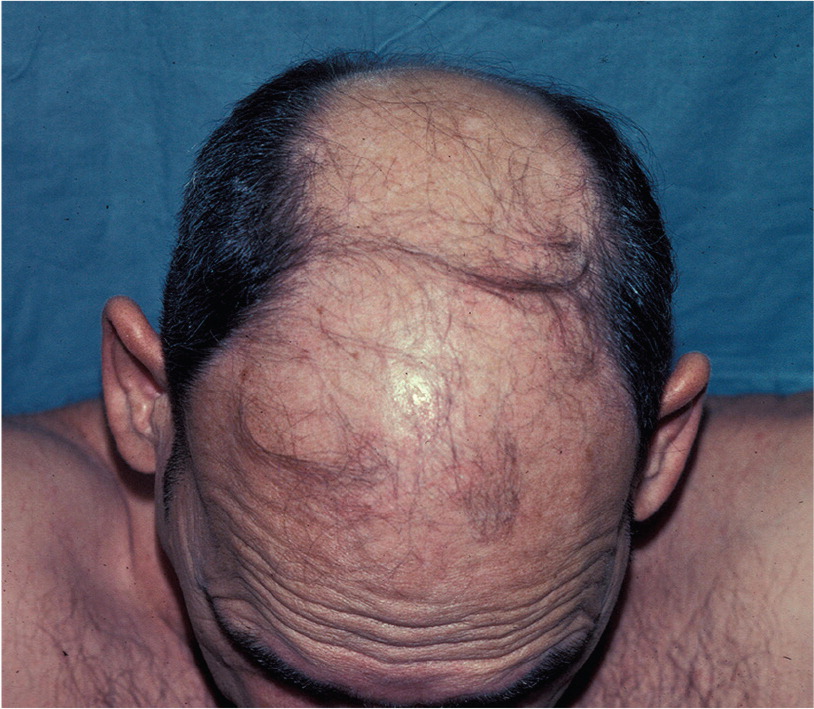

Hair thinning occurs in a sex-specific pattern. Men typically present with bitemporal thinning, thinning of the frontal and vertex scalp, or complete hair loss with residual hair at the occiput and temporal fringes.5 Women typically present with diffuse hair thinning of the vertex with sparing of the frontal hairline. Some women experience thinning over the lateral scalp. Common conditions that mimic androgenetic alopecia include thyroid disease, iron deficiency anemia, and malnutrition.
Treatment is based on patient preference. Topical minoxidil (2% or 5% solution) is approved for the treatment of androgenetic alopecia in men. Hair regrowth is more robust at the vertex than in the frontal area, and will take six to 12 months to improve.5 Treatment should continue indefinitely because hair loss reoccurs when treatment is discontinued. Minoxidil 2% solution is recommended for the treatment of androgenetic alopecia in women.6 Adverse effects include irritant and contact dermatitis.
Finasteride (Propecia), 1 mg per day orally, is approved to treat androgenetic alopecia in men for whom topical minoxidil has been ineffective. Adverse effects of finasteride include decreased libido, erectile dysfunction, and gynecomastia.7
Minoxidil and oral finasteride are the only treatments currently approved by the U.S. Food and Drug Administration for the treatment of androgenetic alopecia. Both of these drugs stimulate hair regrowth in some men, but are more effective in preventing progression of hair loss. Although there are a number of other treatments listed in various texts, there is not good evidence to support their use.8
ALOPECIA AREATA
Alopecia areata is an acute, patchy alopecia that affects up to 2% of the population with no difference between sexes 9 (Figure 3). Approximately 20% of affected patients are children.10 The etiology is unknown, but the pathogenesis is likely autoimmune. Patients may have a single episode, or they may have remission and recurrence. The diagnosis can usually be made clinically.
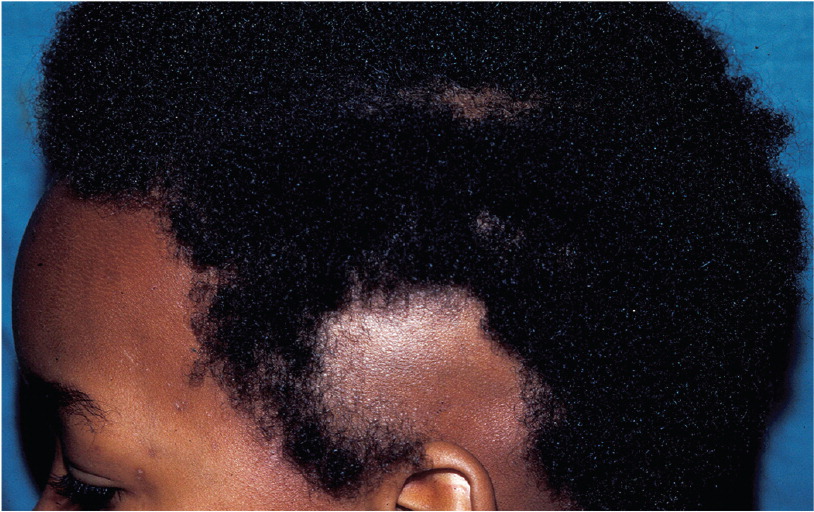
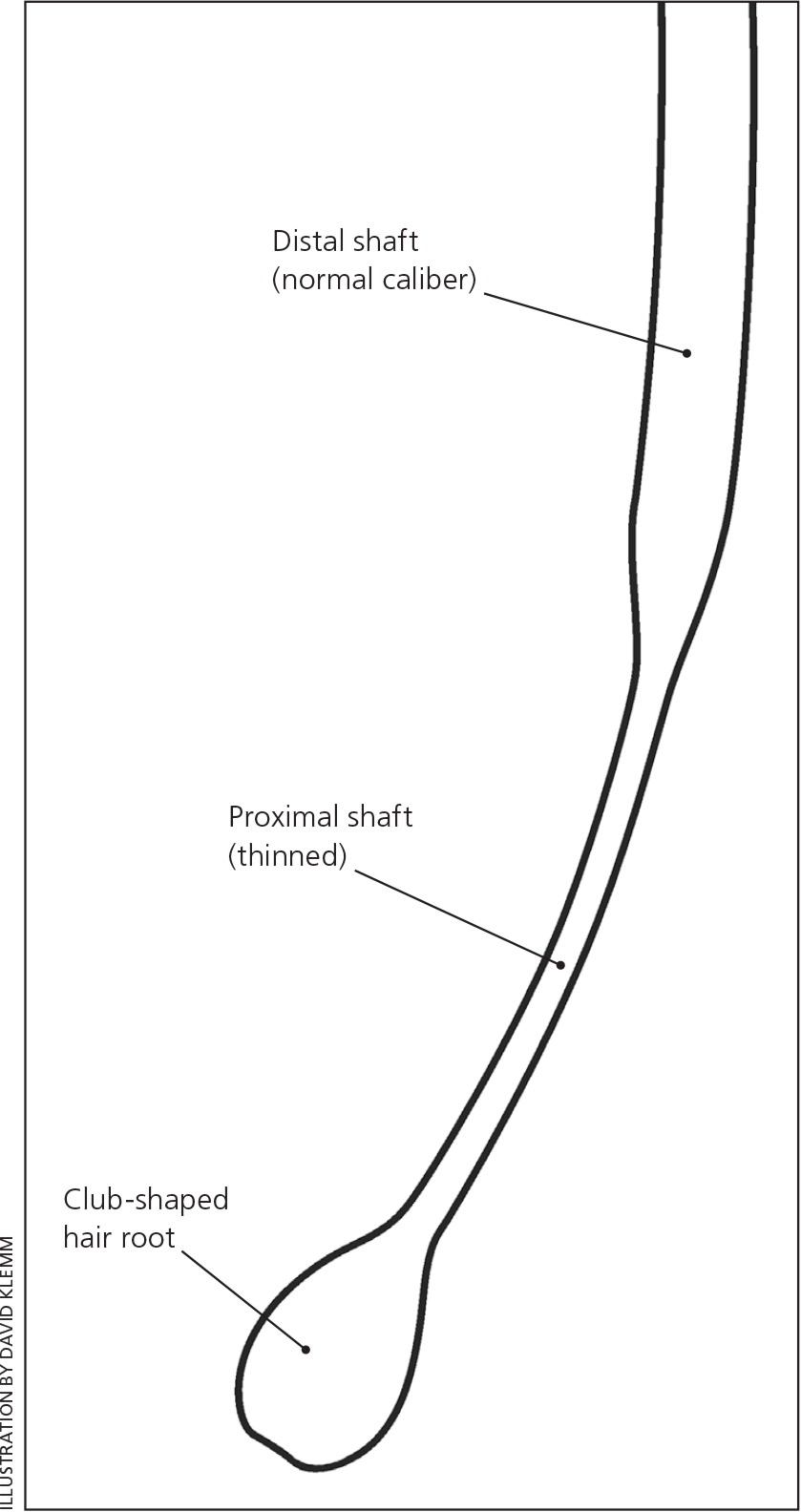
Hair loss in alopecia areata occurs in three different patterns: patchy alopecia is circumscribed, oval-shaped, flesh-colored patches on any part of the body; alopecia totalis involves the entire scalp; and alopecia universalis involves the whole body. Evaluation of the scalp may reveal short vellus hairs, yellow or black dots, and broken hair shafts (which are not specific to alopecia areata). Microscopic examination of the hair follicles demonstrates exclamation mark hair (i.e., hairs that are narrower closer to the scalp and mimic an exclamation point; Figure 44). Nail pitting is also associated with alopecia areata.
Treatment for adults with less than 50% of scalp involvement is intralesional triamcinolone acetonide injected intradermally using a 0.5-inch, 30-gauge needle. Maximal volume is 3 mL per session.11 Treatment may be repeated every four to six weeks until resolution or for a maximum of six months. Local adverse effects include transient atrophy and telangiectasia.
Other therapies for the treatment of alopecia areata include topical mid- to high-potency corticosteroids, minoxidil, anthralin, immunotherapy (diphenylcyclopropenone, squaric acid dibutylester), and systemic corticosteroids.12 Currently available therapies often yield unsatisfactory results, and some clinicians rely on the high rate of spontaneous remission or recommend a hairpiece or wig if remission does not occur.13
TINEA CAPITIS
Tinea capitis is a dermatophyte infection of the hair shaft and follicles that primarily affects children (Figure 5). Risk factors include household exposure and exposure to contaminated hats, brushes, and barber instruments. Trichophyton tonsurans is the most common etiology in North America.14 Transmission occurs person-to-person or from asymptomatic carriers. Infectious fungal particles may remain viable for many months; other vectors include fallen infected hairs, animals, and fomites. Microsporum audouinii is commonly spread by dogs and cats.

Patients with tinea capitis typically present with patchy alopecia with or without scaling, although the entire scalp may be involved. Other findings include adenopathy and pruritus. Children may have an associated kerion, a painful erythematous boggy plaque, often with purulent drainage and regional lymphadenopathy. Posterior auricular lymphadenopathy may help differentiate tinea capitis from other inflammatory causes of alopecia. If the diagnosis is not clear from the history and physical examination, a skin scraping taken from the active border of the inflamed patch in a potassium hydroxide preparation can be examined microscopically for the presence of hyphae. Skin scrapings can also be sent for fungal culture, but this is less helpful because the fungi can take up to six weeks to grow.
Tinea capitis requires systemic treatment; topical antifungal agents do not penetrate hair follicles. If the causative agent is a Trichophyton species, treatment options include oral terbinafine (Lamisil), itraconazole (Sporanox), fluconazole (Diflucan), and griseofulvin.15 These agents have similar efficacy rates and potential adverse effects, but griseofulvin requires a longer treatment course. Griseofulvin is the preferred treatment for infections caused by Microsporum species, but definitive studies are lacking.15,16 There are limited data about empiric treatment before culture results are available. Because griseofulvin may have lower cure rates in the treatment of T. tonsurans infections, it may not be as effective when used empirically.15 All close contacts of patients with tinea capitis should be examined for signs of infection and treated, if necessary.
TELOGEN EFFLUVIUM
Telogen effluvium is a nonscarring, noninflammatory alopecia of relatively sudden onset, with similar incidences between sexes and age groups. It occurs when large numbers of hairs enter the telogen phase and fall out three to five months after a physiologic or emotional stressor. The list of inciting factors is extensive and includes severe chronic illnesses, pregnancy, surgery, high fever, malnutrition, severe infections, and endocrine disorders. Causative medications include retinoids, anticoagulants, anticonvulsants, beta blockers, and antithyroid medications; discontinuation of oral contraceptive agents is another possible cause.17
Patients with telogen effluvium may have symptoms of an underlying condition, but are often asymptomatic. They often notice clumps of hair coming out in the shower or in their hairbrush. They should be asked to recall any potential trigger two to five months before the onset of the condition.
Examination of the scalp in patients with telogen effluvium typically shows uniform hair thinning. The presence of erythema, scaling, or inflammation; altered or uneven hair distribution; or changes in shaft caliber, length, shape, or fragility may suggest other diagnoses. Laboratory investigations are indicated if the history and physical examination findings suggest underlying systemic disorders (e.g., iron deficiency anemia, zinc deficiency, renal or liver disease, thyroid disease).
Telogen effluvium is usually self-limited and resolves within two to six months. Treatment involves eliminating the underlying cause and providing reassurance. Potentially causative medications should be discontinued, if possible. Telogen effluvium may last for years if the underlying stress continues.
TRICHOTILLOMANIA
Trichotillomania is an impulse-control disorder with a mean age of onset of approximately 13 years (Figure 6). Patients with this condition consciously or unconsciously pull, twist, or twirl their hair. Trichotillomania is reported to affect as much as 4% of the population, with the highest incidence in childhood and adolescence.18
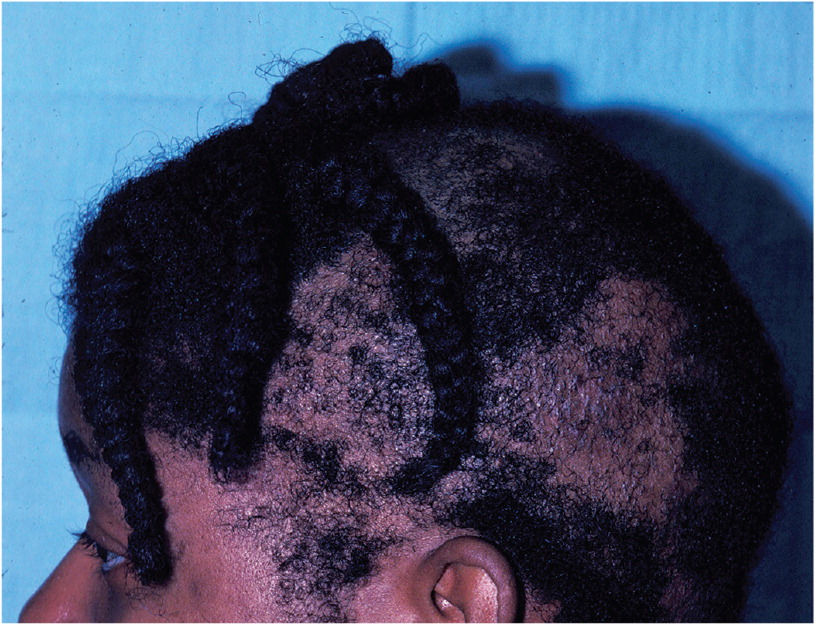
Trichotillomania may be difficult to diagnose if the patient is not forthcoming about pulling at his or her hair. Patients typically present with frontoparietal patches of alopecia that progress posteriorly and may include the eyelashes and eyebrows. Bare patches are typical, and the hair may appear uneven, with twisted or broken off hairs. Trichotillomania may lead to problems with self-esteem and social avoidance. Complications include infection, skin damage, and permanent scarring.18
The optimal treatment for this condition is not known, and psychiatric referral may be indicated. Treatment options include cognitive behavior therapy19 and selective serotonin reuptake inhibitors, although strong evidence of a treatment effect has not been demonstrated. Preliminary evidence suggests positive treatment effects with acetylcysteine, olanzapine (Zyprexa), and clomipramine (Anafranil).19 A combination of cognitive behavior therapy and medications may be more effective than either approach alone.19
TRICHORRHEXIS NODOSA
Trichorrhexis nodosa occurs when hairs break secondary to trauma or because of fragile hair (Figure 7). It affects the proximal hair shaft, although the distal shaft may also be involved.20 Causative traumas include excessive brushing, heat application, tight hairstyles, trichotillomania, and conditions that cause excessive scalp scratching. Chemical traumas include harsh hair treatments (e.g., excessive use of bleach, dye, shampoo, perms, or relaxers21) and excessive exposure to salt water. Examples of congenital or genetic conditions that may cause trichorrhexis nodosa include trichorrhexis invaginata (bamboo hair), intussusception of the hair shaft at the keratinization zone, Menkes disease, keratinization defects due to defective copper metabolism, and argininosuccinic aciduria.22 Rarely, trichorrhexis nodosa can be a manifestation of hypothyroidism.23

On examination, hairs appear to have white nodes; on closer inspection, these are shown to be fracture sites along the shaft and cortex that have split into several strands. On dermoscopy, hairs look like two brooms or paint brushes thrust together.
If the diagnosis is not clear, laboratory testing should include a complete blood count, iron studies, copper level, liver function testing, thyroid-stimulating hormone level, and serum and urine amino acid levels. Treatment includes avoiding or minimizing physical and chemical trauma.
ANAGEN EFFLUVIUM
Anagen effluvium is abnormal diffuse hair loss (usually abrupt) during the anagen phase due to an event that impairs the mitotic or metabolic activity of the hair follicle. The incidence of anagen effluvium after chemotherapy is approximately 65%24; it is most commonly associated with cyclophosphamide, nitrosoureas, and doxorubicin (Adriamycin). Other causative medications include tamoxifen, allopurinol, levodopa, bromocriptine (Parlodel), and toxins such as bismuth, arsenic, and gold. Other medical and inflammatory conditions, such as mycosis fungoides or pemphigus vulgaris, can lead to anagen effluvium.25
Patients typically present with diffuse hair loss that begins days to weeks after exposure to a chemotherapeutic agent and is most apparent after one or two months.26 Approximately 50% of women with cancer consider hair loss to be the most traumatic aspect of chemotherapy and nearly 10% would decline treatment for fear of hair loss.26,27
Anagen effluvium is usually reversible, with regrowth one to three months after cessation of the offending agent. Permanent alopecia is rare. A large meta-analysis of clinical trials concluded that scalp cooling was the only intervention that significantly reduced the risk of chemotherapy-induced anagen effluvium.27 However, scalp cooling should be discouraged because it may minimize delivery of chemotherapeutic drugs to the scalp, leading to cutaneous scalp metastases.27
This article updates previous articles on this topic by Mounsey and Reed4 ; Springer, et al.28 ; and Thiedke.29
Data Sources: We searched PubMed using the key words alopecia areata, tinea capitis, trichotillomania, trichorrhexis nodosa, anagen effluvium, and telogen effluvium. We also searched reference lists from relevant articles and textbooks.
