
Am Fam Physician. 2017;96(12):797-804
Author disclosure: No relevant financial affiliations.
Pigmentation disorders are commonly diagnosed, evaluated, and treated in primary care practices. Typical hyperpigmentation disorders include postinflammatory hyperpigmentation, melasma, solar lentigines, ephelides (freckles), and café au lait macules. These conditions are generally benign but can be distressing to patients. Appropriate dermatologic history, skin examination, and skin biopsy, when appropriate, can help exclude melanoma and its precursors. In addition to addressing the underlying condition, hyperpigmentation is treated with topical agents, chemical peels, cryotherapy, light or laser therapy, or a combination of these methods. Café au lait macules are treated with surgical excision or laser therapy if treatment is desired. Hypopigmentation disorders include vitiligo, pityriasis alba, tinea versicolor, and postinflammatory hypopigmentation. Treatment of vitiligo depends on the distribution and extent of skin involvement, and includes topical corticosteroids and calcineurin inhibitors, ultraviolet A therapy (with or without psoralens), narrowband ultraviolet B therapy, and cosmetic coverage. Patients with stable, self-limited vitiligo may be candidates for surgical grafting techniques, whereas those with extensive disease may be candidates for depigmentation therapy to make skin tone appear more even. Other hypopigmentation disorders may improve or resolve with treatment of the underlying condition.
Pigmentation disorders of the skin are commonly encountered in primary care practice. Although they are often benign and easily distinguishable based on appearance and location, it may be necessary to perform a skin biopsy to exclude melanoma and its precursors. Some disorders result in cosmetic or psychological concerns to the patient, necessitating evaluation and treatment. Proper diagnosis allows the physician to facilitate appropriate skin treatment, provide reassurance, or initiate appropriate referral.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Triple combination therapy (fluocinolone 0.01%/hydroquinone 4%/tretinoin 0.05% [Tri-luma]) is the most effective agent for treatment of moderate to severe epidermal melasma. | C | 1, 7 |
| Triple combination therapy (fluocinolone 0.01%/hydroquinone 4%/tretinoin 0.05%) can enhance resolution of solar lentigines treated with cryotherapy. | B | 11 |
| Class III corticosteroids and narrowband ultraviolet B are the most effective and safest treatments for localized and generalized vitiligo, respectively. | B | 14 |
| Topical tacrolimus (Protopic) 0.1% ointment is a safe and effective alternative to topical corticosteroids for treatment of pityriasis alba. | B | 26 |
| Topical antifungal agents and topical adapalene (Differin) gel are effective treatments for tinea versicolor. | A | 27, 28 |
Hyperpigmentation is the result of excess melanin production, distribution, or transport. Common etiologies include postinflammatory hyperpigmentation, melasma, solar lentigines, ephelides, and café au lait macules. Hypopigmentation results from a reduction of melanocytes or an inability of the melanocytes to produce melanin or properly transport melanosomes. Vitiligo, pityriasis alba, tinea versicolor, and postinflammatory effect are common causes of pigment loss. This article discusses clinical features of each condition, updated and novel treatments, and current evidence supporting their use. Table 1 summarizes current treatments.1
| Disorder | Description | Location | Etiology | Treatment* |
|---|---|---|---|---|
| Hyperpigmentation disorders | ||||
| Postinflammatory hyperpigmentation | Irregular, darkly pigmented macules/patches | Previous sites of injury or inflammation | Trauma, inflammation | Triple combination therapy,† hydroquinone, retinoids, azelaic acid (Finacea), chemical peels, laser therapy |
| Melasma | Pigmented, well-defined macules; light brown, brown, or gray | Face (centrofacial 63%, malar 21%, mandibular 16%) or forearms | Pregnancy, oral contraceptives, phenytoin (Dilantin), idiopathic | Triple combination therapy,† chemical peels, light or laser therapy, sunscreen |
| Solar lentigines | 1- to 3-cm well-circumscribed macules; light yellow to dark brown, variegated | Face, hands, forearms, chest, back, shins | Acute or chronic ultraviolet exposure | Triple combination therapy† with or without cryotherapy, hydroquinone, retinoids, chemical peels, cryotherapy, intense pulsed light, laser therapy |
| Ephelides | 1- to 2-mm sharply defined macules, red or tan to light brown | Face, neck, chest, arms, legs | Childhood onset after sun exposure in susceptible individuals (skin types I or II) | Fades in winter months so treatment may be unnecessary; cryotherapy, hydroquinone, azelaic acid, chemical peels, laser therapy |
| Café au lait macules | 1- to 20-cm tan to brown macules, epidermal, present at birth or early childhood | Most commonly trunk but may appear anywhere | Increased melanin in melanocytes/basal keratinocytes | Laser therapy, surgical excision |
| Hypopigmentation disorders | ||||
| Vitiligo | Hypopigmented macules and patches; sharply defined; 5 to 50 mm; coalescent | Face, hands, forearms, neck, genitalia, body folds, periorificial; lip-tip pattern | Unknown, possibly immune-mediated | High-potency topical corticosteroids (class II and III), topical calcineurin inhibitors, narrowband ultraviolet B, psoralen and ultraviolet A, systemic corticosteroids |
| Pityriasis alba | Hypopigmented, irregular patches; fine scale; itchy | Face, head, neck, forearms | Possible association with atopic dermatitis aggravated by sunlight exposure | Sunscreen, topical corticosteroids, tacrolimus (Protopic) ointment |
| Tinea versicolor | Hypopigmented or pink plaques; may be hyperpigmented; fine scale | Neck, chest, back, abdomen, proximal extremities | Malassezia spp. infection | Topical antifungals, topical adapalene (Differin) gel |
| Postinflammatory hypopigmentation | Loss of pigment (variable), macules, patches | Varies | Tinea versicolor, atopic dermatitis, pityriasis alba, psoriasis, guttate parapsoriasis, dermabrasion, chemical peels, intralesional corticosteroid use | Treatment of underlying condition when applicable |
Skin Types
The Fitzpatrick scale, which ranges from skin types I to VI, is used to define and estimate skin response to ultraviolet exposure (Table 21). Certain skin pigmentation disorders are more common in particular skin phenotypes (e.g., solar lentigines or ephelides in lighter skin [types I to III], melasma in darker skin [types IV to VI]).1 Skin types can be classified using online tools.
| Skin type | Skin/hair/eye color | Characteristics |
|---|---|---|
| I | White; very fair; red or blond hair; blue eyes; freckles | Always burns, never tans |
| II | White; fair; red or blond hair; blue, hazel, or green eyes | Usually burns, tans with difficulty |
| III | Cream white; fair with any eye or hair color; very common | Sometimes mild burn, gradually tans |
| IV | Brown; typical Mediterranean/Caucasian skin | Rarely burns, tans easily |
| V | Dark brown; Middle-Eastern skin | Very rarely burns, tans very easily |
| VI | Black | Never burns, tans very easily |
Hyperpigmentation Disorders
POSTINFLAMMATORY HYPERPIGMENTATION
Postinflammatory hyperpigmentation is a common consequence of trauma or inflammation primarily in darker skin types (III to VI). Lesions can persist for months or years, and can be psychologically devastating to some patients.
Postinflammatory hyperpigmentation presents as irregular, darkly pigmented skin at sites of previous injury or inflammation, as a consequence of laser or light therapy, or following cryotherapy. Inflammation stimulates prostaglandin, leukotriene, and thromboxane production, resulting in epidermal melanocyte hypertrophy and increased melanin synthesis (Figures 1 and 2).


Combination therapy usually produces the best results. Treatment of the underlying condition (e.g., acne, eczema) can help speed recovery, although weeks or months of therapy may be required, and resolution of hyperpigmentation is slow. Kligman's formula (hydroquinone 2%, tretinoin [Retin-A] 0.025%, and mometasone [Elocon] 0.1%) and Tri-luma (fluocinolone 0.01%/hydroquinone 4%/tretinoin 0.05%) are among the commercially available combination products. Azelaic acid (Finacea), dexamethasone, salicylic acid, glycolic acid peels, retinoids, and laser treatments are sometimes helpful as monotherapy. Initial treatment with hydroquinone followed by serial chemical peels may be useful in chronic hyperpigmentation. Risk of ochronosis (blotchy hyperpigmentation) with typical hydroquinone formulations (2% to 4%) is rare. Topical retinoids (e.g., tretinoin, 0.05% to 0.1%; tazarotene [Tazorac], 0.1%) are somewhat effective at reducing hyperpigmentation and disease severity, and are well tolerated. Treatment options may be affected by cost and insurance coverage.2–5
In one limited trial involving patients at lowest risk of postinflammatory hyperpigmentation, pretreatment with topical tretinoin showed no conclusive benefit.6 No preventive measures have proven beneficial in any skin type.
MELASMA
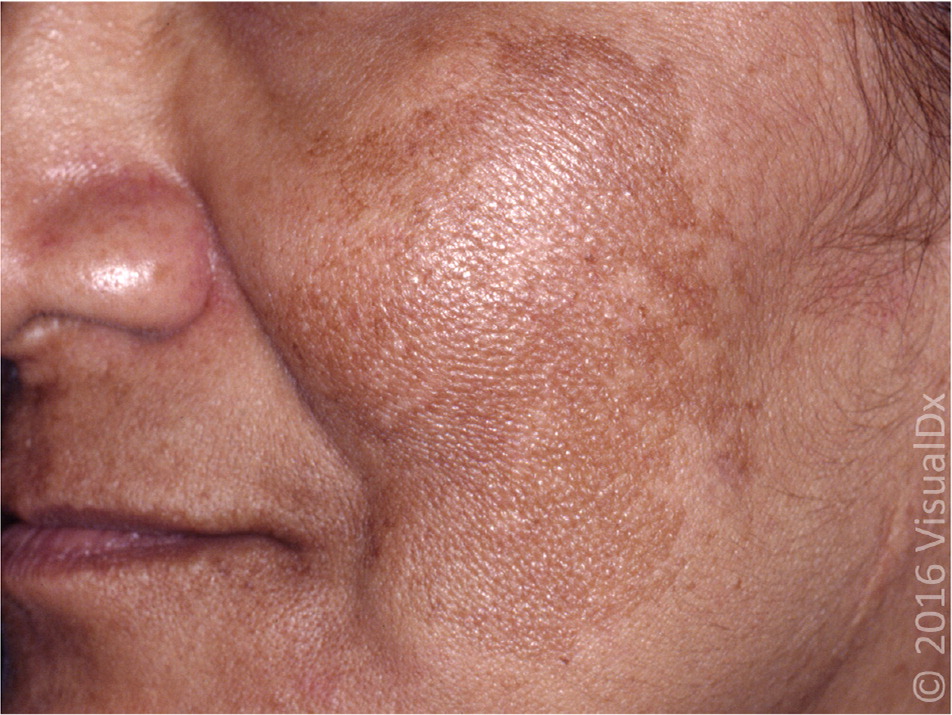
Melasma is a progressive, macular, nonscaling hypermelanosis of sun-exposed skin, primarily on the face and dorsal forearms (Figure 3). It is usually associated with pregnancy or use of oral contraceptives or anticonvulsants (e.g., phenytoin [Dilantin]), or it may be idiopathic. Melasma disproportionately affects women (9:1 ratio), as well as skin types IV to VI.1 It is usually asymptomatic, but it may be cosmetically distressing to the patient. There are three typical patterns of distribution: centrofacial (63%), malar (21%), and mandibular (16%).1 It is usually, but not always, bilateral. Epidermal melasma tends to be light brown, enhancing under Wood Lamp examination. Dermal melasma appears grayish in color and is nonenhancing. Mixed types of melasma are dark brown with variable enhancement. Dermal melasma is resistant to topical therapy. Dermatologic referral is recommended in these cases.1
An evidence-based review of melasma treatments, including topical depigmenting therapies (hydroquinone, tretinoin, and fluocinolone), chemical peels, and light and laser therapies, demonstrated that combination triple therapy (Tri-luma) was most effective for treating moderate to severe melasma but had a high incidence of erythema and peeling (40%).7 Treatment must be continued indefinitely to maintain effect. Chemical peels, light therapy, and laser therapy had mixed results. Adverse events included irritation of skin and postprocedure hyperpigmentation, which was more common in darker skin types.7–10
Sunscreens are universally recommended to prevent worsening of melasma from further sun exposure. Pregnancy-induced melasma tends to fade postpartum, and treatment should be postponed to allow natural fading.
SOLAR LENTIGINES
Solar lentigines (liver spots) are macular, 1- to 3-cm, hyperpigmented, well-circumscribed lesions on sun-exposed surfaces of the skin. They vary from light yellow to dark brown and often have a variegated appearance. The face, hands, forearms, chest, back, and shins are the most common locations (Figure 4). Whites and Asians are most often affected.
Solar lentigines result from a local mild proliferation of basal melanocytes from acute and chronic ultraviolet exposure, and subsequent increase in melanization. They differ from ephelides, which result from increased melanin production. The differential diagnosis includes ephelides, café au lait macules, pigmented actinic keratoses, and lentigo maligna. Biopsy should be performed if there is rapid growth or change in a lesion, symptomatic lesions (e.g., pain, itching, easy bleeding, poor healing), atypical lesions, or lesions with features suspicious for melanoma.1
Treatment consists of topical (e.g., hydroquinone, retinoids) and ablative (e.g., chemical peels, cryotherapy, intense pulsed light, lasers) therapies. Topical therapies for solar lentigines are the most consistently effective treatments. Hydroquinone is effective but can cause hypersensitivity and acneiform eruptions. Topical triple combination therapy may be used with or without cryotherapy. In one study, triple combination therapy used with cryotherapy enhanced resolution of solar lentigines and was well tolerated.11 Retinoids such as tazarotene (0.1% cream), tretinoin (0.025% to 0.05%), and adapalene gel (Differin, 0.1% or 0.3%) may reduce hyperpigmentation, but evidence is limited.1 Adapalene 0.1% gel has been approved for over-the-counter sale by the U.S. Food and Drug Administration.
Chemical peels with 30% to 35% trichloroacetic acid solution or cryotherapy with liquid nitrogen have resulted in significant lightening of lentigines, but data are limited on long-term improvements and recurrences are common.1 Cryotherapy is associated with pain and a risk of hyperpigmentation. Brief cryotherapy (less than five seconds) with repeated treatments is preferred over more intense one-time treatment. Multiple light and laser modalities are also effective, but they are more likely to cause postinflammatory hyperpigmentation and usually require dermatologic referral.1 Figures 5a and 5b show solar lentigines before and after laser treatment.

Prevention of solar lentigines requires limiting sun exposure and regularly using sunscreen, especially in patients with fair skin (types I to III) and those prone to freckling, and by prevention of sunburns, especially after 20 years of age.
EPHELIDES
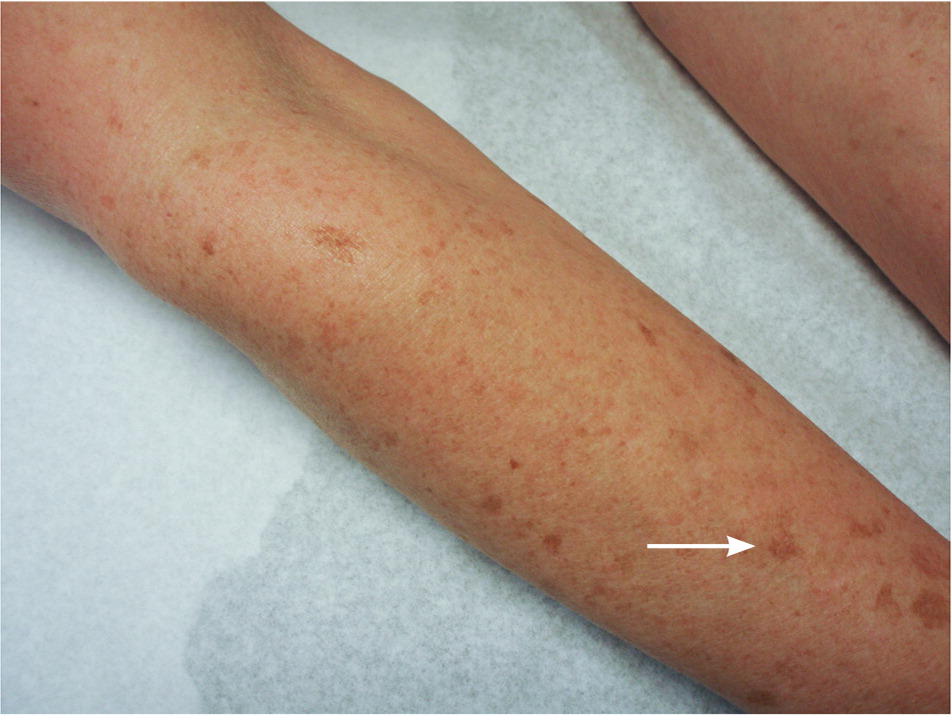
Ephelides (freckles) are small, 1- to 2-mm, sharply defined macular lesions of uniform color, most often found on the face, neck, chest, arms, and legs. Color may vary from red to tan to light brown, and number from a few to hundreds (Figure 6). Onset is usually in childhood after sun exposure. These lesions should be differentiated from juvenile lentigines (2 to 10 mm), which appear in early childhood, and solar lentigines (2 to 20 mm), which usually appear later in life. Ephelides are asymptomatic, and treatment is not necessary. Undesired lesions can be treated similarly to lentigines using cryotherapy, hydroquinone, azelaic acid, glycolic acid peels, and laser and other light-based therapies.1,12

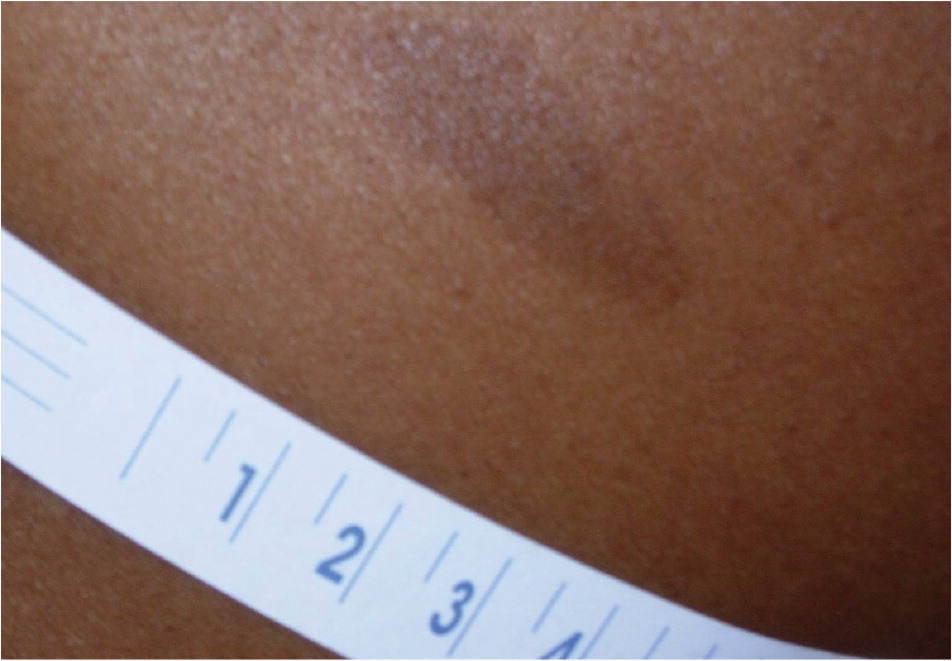
CAFÉ AU LAIT MACULES
Café au lait macules are tan to brown macules ranging from 1 to 20 cm and are present at birth or early in life (Figure 71). They are epidermal and may be found on any body part, most commonly the trunk. About 10% to 30% of the general population has an isolated café au lait macule.13 They are asymptomatic and do not require treatment. They result from an increase in melanin concentration in melanocytes and basal keratinocytes. More than six lesions (5 mm or larger prepubertal or 15 mm or larger postpubertal) should raise suspicion for tuberous sclerosis, neurofibromatosis, Albright syndrome, or Fanconi anemia. Cosmetic treatments include laser therapy or surgical excision.1
Hypopigmentation Disorders
VITILIGO
Vitiligo is an immune-mediated skin condition resulting in a loss of pigmentation (Figure 81 and Figure 9). Its exact etiology is unknown. It affects all skin types and is generally considered a cosmetic condition, but it can cause significant psychological distress, particularly in black patients, prompting requests for treatment. Quality of life is often negatively affected.


Vitiligo is present in 0.5% to 2% of the general population. There is no race or sex predilection. Family history is positive in 25% to 30% of patients with vitiligo.1 Onset is often insidious but is commonly related to a recent stress, illness, or trauma (e.g., sunburn). Peak onset is in the second and third decades of life, with 50% occurring before 20 years of age.1 There is some association between vitiligo and thyroid disease, pernicious anemia, and diabetes mellitus.
There are two common types of vitiligo: segmental and nonsegmental (i.e., localized and generalized). Segmental vitiligo presents as a unilateral or band-shaped distribution of hypopigmented macules, usually 5 to 50 mm in size and coalescent, with rapid stabilization and early age of onset. Nonsegmental vitiligo is typically bilateral or scattered symmetrically and evolves over time. It is considered generalized when it covers more than 10% of body surface area. Acral or acrofacial vitiligo typically involves the face and distal extremities (the so-called lip-tip pattern). Lesions of the head and neck tend to be most responsive to treatment; lesions on the extremities and genitalia tend to be more recalcitrant.
There are multiple treatment modalities for vitiligo. Combination therapy tends to be more effective at repigmentation than monotherapy, although recurrence is common (up to 40%), as is treatment failure.14 Improvement in quality of life, as measured by standardized questionnaires (e.g., Dermatology Quality of Life Index), does not consistently correlate with repigmentation success.14
High-potency topical corticosteroids (betamethasone 0.1% or fluocinonide 0.05% ointment) and topical calcineurin inhibitors (tacrolimus [Protopic] and pimecrolimus [Elidel]) are mainstays for localized treatment of limited vitiligo. Systemic therapies such as psoralen and ultraviolet A, narrowband ultraviolet B (UVB), and systemic corticosteroids are useful for more widespread or treatment-resistant disease. These therapies generally require dermatologic referral.
A Cochrane review found that class III corticosteroids (e.g., betamethasone) and narrowband UVB are the most effective and safest treatments for localized and generalized vitiligo, respectively.14 Afamelanotide, a novel melanocyte-stimulating hormone implant, has been shown in small studies to accelerate repigmentation when used with narrowband UVB, potentially limiting UVB exposure. Phase 2 and 3 studies are ongoing in the United States.15 Vitamin D analogues, antioxidants, light therapy, latanoprost (Xalatan), and excimer laser treatments have been studied alone and in combination, although none was conclusively better than standard treatment, and most studies were small and unreplicated, and inconsistently reported quality-of-life measures.16–23
Sun protection is recommended in vitiligo. Broad-spectrum sunscreens, sun-protective clothing (hats, shirts, pants) and certain makeup can offer protection to affected areas. Concealers (e.g., Dermablend, Cover-mark), topical dyes, and sunless self-tanning products (best on skin types II and III) may reduce skin pigment disparity.
For most patients with extensive generalized vitiligo (more than 50% of body surface area affected), homogeneous skin depigmentation therapy with topical mono-benzone 20% is successful, although recurrences are possible. However, monobenzone is no longer available in the United States. Possible alternatives include cryotherapy and laser therapy.24 Sun protection is essential after treatment.1
Patients with segmental, stable, or lip-tip vitiligo can be treated with autologous transplantation methods. Split thickness and suction blister epidermal grafting techniques appear to be the safest and most effective, although transplant studies often lacked comparative controls.17
Future studies on vitiligo are investigating the effect of psychological interventions on disease management. It is possible that such modalities in combination with standard treatment regimens may provide additional benefit.25
PITYRIASIS ALBA
Pityriasis alba is a disorder commonly associated with atopic dermatitis, usually presenting as hypopigmented, irregular patches on the face, head, neck, and forearms in children and young adults. It is most notable in skin types III to VI. A fine scale with itching is occasionally present. Excessive unprotected sun exposure may be a trigger.
Because pityriasis alba is self-limited, no treatment is necessary. However, topical corticosteroids and sunscreens are first-line treatments in symptomatic patients. Use of low-potency hydrocortisone (0.5% to 2.5%) can minimize the risk of skin atrophy, striae, and steroid acne. Topical tacrolimus 0.1% ointment, applied twice per day, is considered a safe and effective alternative. Mild skin irritation is common.26
TINEA VERSICOLOR
Tinea versicolor (pityriasis versicolor) is a superficial fungal skin infection, caused by Malassezia spp. It often presents as hypopigmented or pink plaques with fine scale on the neck, chest, back, abdomen, and proximal extremities. Occasionally, it may be hyperpigmented. The diagnosis is often clinical, with confirmation by microscopy using potassium hydroxide preparation. Standard treatments include topical selenium sulfide, zinc pyrithione, and antifungals (e.g., onazole). Adapalene gel was also found to be noninferior to ketoconazole in one study.27 Topical allylamines (e.g., terbinafine [Lamisil]) were better than azoles (e.g., ketoconazole) for sustained cures.28 Oral antifungal treatment may be used if topical treatment is unsuccessful or impractical.
POSTINFLAMMATORY HYPOPIGMENTATION
Inflammatory conditions of the skin can cause loss of pigment. Tinea versicolor, atopic dermatitis, pityriasis alba, psoriasis, and guttate parapsoriasis may affect pigment production or transport. Treatment of the underlying condition may improve hypopigmentation over time. Dermabrasion, chemical peels, cryotherapy, and intralesional corticosteroids can also reduce pigment locally, and these risks should be discussed with patients before treatment.
Data Sources: The literature search was performed using PubMed with key words postinflammatory hyperpigmentation, postinflammatory hypopigmentation, solar lentigines, tinea versicolor, melasma, vitiligo, café au lait macules, and pityriasis alba, and was limited to randomized controlled trials, practice guidelines, and clinical reviews for the past five years. References from Essential Evidence Plus were also used. Search dates: September 2015 and June 2017.
