
Am Fam Physician. 2018;97(1):38-44
Patient information: See related handout on pityriasis rosea written by the authors of this article.
Author disclosure: No relevant financial affiliations.
Pityriasis rosea is a common self-limiting rash that usually starts with a herald patch on the trunk and progresses along the Langer lines to a generalized rash over the trunk and limbs. The diagnosis is based on clinical and physical examination findings. The herald patch is an erythematous lesion with an elevated border and depressed center. The generalized rash usually presents two weeks after the herald patch. Patients can develop general malaise, fatigue, nausea, headaches, joint pain, enlarged lymph nodes, fever, and sore throat before or during the course of the rash. The differential diagnosis includes secondary syphilis, seborrheic dermatitis, nummular eczema, pityriasis lichenoides chronica, tinea corporis, viral exanthems, lichen planus, and pityriasis rosea–like eruption associated with certain medications. Treatment is aimed at controlling symptoms and consists of corticosteroids or antihistamines. In some cases, acyclovir can be used to treat symptoms and reduce the length of disease. Ultraviolet phototherapy can also be considered for severe cases. Pityriasis rosea during pregnancy has been linked to spontaneous abortions.
Pityriasis rosea is a self-limiting skin condition that presents as discrete scaly papules and plaques along the Langer lines (cleavage lines) over the trunk and limbs. This generalized rash is usually preceded by a herald patch on the trunk.1,2 The incidence is 170 cases per 100,000 persons per year.2 It typically affects persons 10 to 35 years of age.2 Some studies report that males and females are equally affected,3 whereas others report that females are affected more often.2 Data on seasonal variation are conflicting, but studies show a higher prevalence during winter.2,3
WHAT IS NEW ON THIS TOPIC
Pityriasis Rosea
Although a small 2000 study of erythromycin suggested possible benefits for pityriasis rosea, subsequent studies concluded that erythromycin and other macrolides are ineffective.
Several randomized controlled trials found that acyclovir, 400 to 800 mg five times per day, improves symptoms and lesion resolution in severe cases.
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Symptoms of pityriasis rosea can be managed with oral or topical corticosteroids or oral antihistamines. | C | 2 |
| Macrolide antibiotics have no benefit in the management of pityriasis rosea. | B | 41–44 |
| Acyclovir is effective in the treatment of pityriasis rosea and may be considered in severe cases. | B | 39, 45–49 |
Etiology
The epidemiology and clinical course of pityriasis rosea suggest an infectious etiology. Temporal case clustering, which indicates infectious transmission, has been documented in regression analysis models.4 Bacterial agents have not been linked to pityriasis rosea.5 A viral etiology was proposed after intranuclear and intracytoplasmic virus-like particles were observed by microscopy. An increase in CD4 lymphocytes and Langerhans cells in the dermis also suggest a viral etiology.6 The most common viruses linked to pityriasis rosea are human herpesvirus-6 and -7 (HHV-6 and -7). HHV-6 typically affects children by two years of age, whereas HHV-7 typically affects children by six years of age.6 Roseola infantum (exanthema subitum) is a common presentation of these viruses in children.7 The development of pityriasis rosea later in life suggests reactivation of these viruses.6,8
However, the studies linking HHV-6 and -7 with pityriasis rosea are conflicting and small. Early polymerase chain reaction studies did not detect active viral DNA in patients with pityriasis rosea, despite their having positive antibodies to HHV-6 and -7.9 A later study using a calibrated quantitative real-time polymerase chain reaction assay found active HHV-6 and -7 in plasma and skin samples.10 Only HHV-7 was found in the peripheral blood mononuclear cells. Another study using polymerase chain reaction testing with specific primers found active HHV-6 and -7 in plasma and tissue samples.11 Electron microscopy detected HHV particles in various stages of morphogenesis in 71% of the 21 patients studied.12 Serologic studies have been of limited value because of their inability to determine acute vs. previous infection.6,9,11,13
Clinical Presentation
CLASSIC
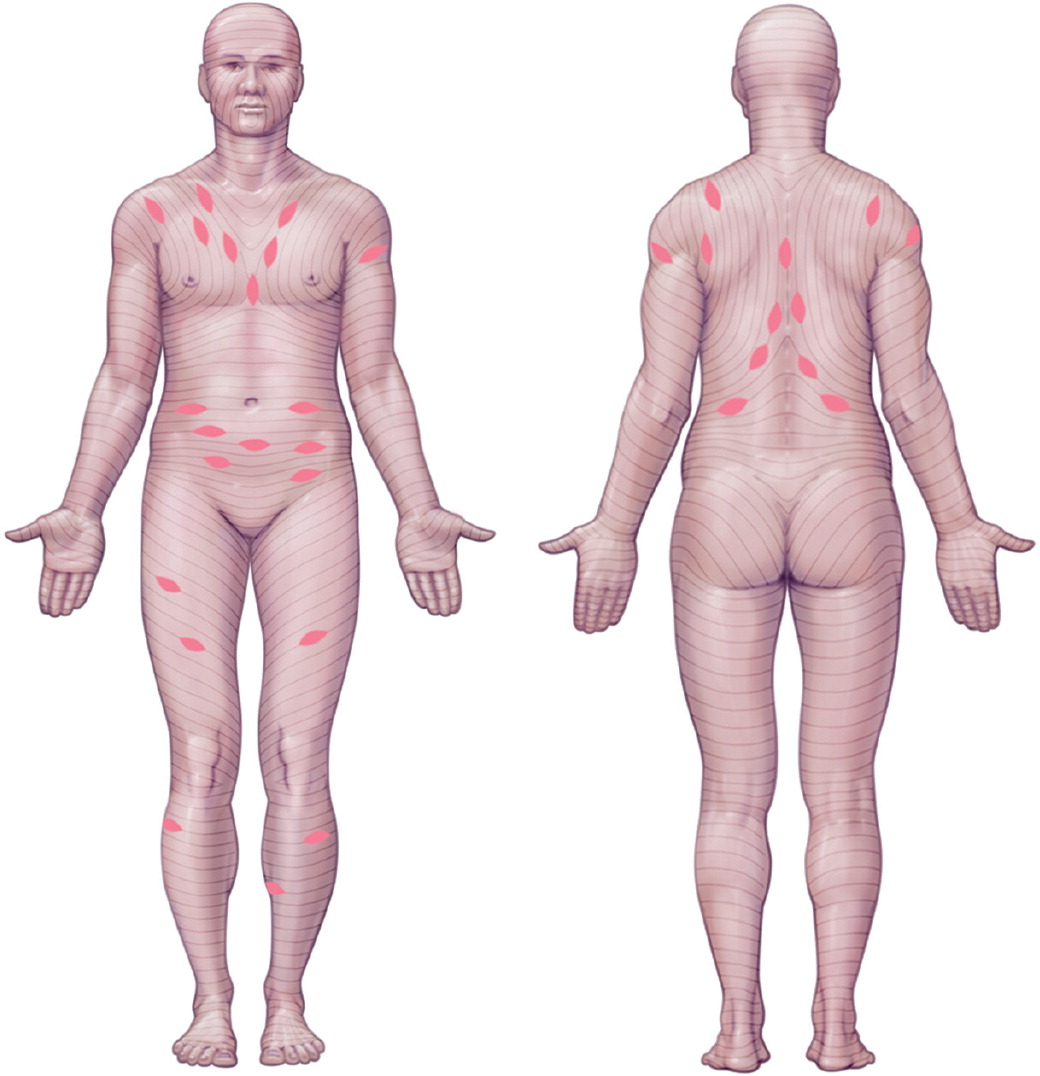
The diagnosis of pityriasis rosea is based on clinical and physical examination findings. Classic pityriasis rosea starts with a herald patch on the trunk (Figure 1 and Figure 21) in up to 90% of cases.3 The patch is erythematous with slightly elevated scaling borders and a lighter depressed center. It can measure 3 cm or more in diameter and may be the only skin manifestation for approximately two weeks.3 Prodromal symptoms (e.g., general malaise, fatigue, nausea, headaches, joint pain, enlarged lymph nodes, fever, sore throat) present before or during the course of the rash in 69% of patients.6 The generalized rash, also known as the secondary eruption, presents on the trunk along the Langer lines (Figure 3 and Figure 41, and Figure 5, Figure 6 and Figure 71) and may extend to the upper arms and upper thighs.2,3 These lesions are smaller than the herald patch and can continue to appear up to six weeks after the initial eruption.2 A rash on the back may have a “Christmas tree” pattern, whereas a rash on the upper chest may have a v-shaped pattern (Figure 8).1 The mean duration of the rash is 45 days; however, it can last up to 12 weeks.2,3 Moderate to severe pruritus occurs in 50% of patients.2







ATYPICAL
Atypical pityriasis rosea has a different rash distribution, morphology, size, and number of lesions. In pityriasis rosea gigantea of Darier, the patient has fewer and larger lesions. Inverse pityriasis rosea predominantly involves the face, axillae, and groin. Pityriasis rosea of Vidal presents with large patches on the axillae or inguinal region.1,3
RELAPSES
SPECIAL POPULATIONS
Differential Diagnosis
The differential diagnosis of pityriasis rosea includes several conditions (Table 1).1,3,7 If the diagnosis is uncertain, skin biopsy will help exclude other pathologies.3 The histology of pityriasis rosea will usually show focal parakeratosis, spongiosis, and acanthosis in the epidermis, and extravasated red blood cells with perivascular infiltrates of lymphocytes, monocytes, and eosinophils in the dermis.
| Condition | Distinguishing characteristics |
|---|---|
| Lichen planus | 1- to 10-mm, sharply defined, flat-topped violaceous papules typically on wrists, lumbar region, shins, scalp, glans penis, and mouth; lesions may be asymptomatic |
| Nummular eczema | Grouped small vesicles and papules 4 to 5 cm in diameter; round or coin-shaped lesions with an erythematous base and distinct borders, often on shins and backs of hands; pruritus is often intense |
| Pityriasis lichenoides chronica | Red-brown papules with central mica-like scales randomly arranged on trunk and proximal extremities with chronic, relapsing course; hypo- or hyperpigmentation may be present after lesions resolve |
| Pityriasis rosea–like eruption associated with medications | Similar presentation to pityriasis rosea, but lesions resolve after causative medication is discontinued (Table 2) |
| Seborrheic dermatitis | Orange-red or gray-white skin with greasy or white dry scaling macules, papules, or patches; diffuse scalp involvement with marked scaling; worsens in winter because of dry conditions; pruritus increases with perspiration |
| Secondary syphilis | 0.5- to 1-cm, pink to brownish-red, round to oval macules and papules on the trunk, palms, and soles; patchy, “moth-eaten” alopecia on the scalp and beard area; mucous membrane involvement with round or oval patches covered by hyperkeratotic white to gray membrane |
| Tinea corporis | Scaling, sharply marginated plaques of various sizes with or without pustules or vesicles along the margins; lesions present with peripheral enlargement and central clearing, producing an annular configuration with concentric rings or arcuate lesions |
| Viral exanthems | Diffuse maculopapular erythema; mucosal involvement with microulcerative lesions, palatal petechiae, or conjunctivitis; systemic findings of lymphadenopathy, hepatomegaly, and splenomegaly |
Case reports have documented pityriasis rosea–like eruptions associated with certain medications (Table 2).1,16–38 In these cases, the rash is more extensive and pruritic than in classic pityriasis rosea, and the histopathology is distinct. Some case studies report the presence of dermal eosinophil infiltrates.3
| Adalimumab (Humira) |
| Allopurinol |
| Arsenic compounds |
| Asenapine (Saphris) |
| Atenolol |
| Bacille Calmette-Guérin therapy |
| Barbiturates |
| Bismuth |
| Bupropion (Wellbutrin) |
| Captopril |
| Clonidine |
| Clozapine (Clozaril) |
| Ergotamine |
| Etanercept (Enbrel) |
| Gold compounds (e.g., auranofin [Ridaura]) |
| Hepatitis B vaccine |
| Imatinib (Gleevec) |
| Influenza (H1N1) vaccine |
| Interferon alfa-2a |
| Isotretinoin |
| Ketotifen (Zaditor) |
| Lamotrigine (Lamictal) |
| Lisinopril |
| Nortriptyline (Pamelor) |
| Omeprazole (Prilosec) |
| Pneumococcal polysaccharide vaccine (Pneumovax) |
| Rituximab (Rituxan) |
| Smallpox vaccine |
| Terbinafine (Lamisil) |
| Yellow fever vaccine |
Treatment
The self-limited course of pityriasis rosea allows for watchful waiting and symptomatic treatment of pruritus in most patients. Treatment with oral antihistamines or topical or oral corticosteroids is advised based on expert consensus and low potential for harm.2,39 Patients with more severe disease or those who choose active treatment should weigh the potential benefits of faster resolution against the adverse effects associated with these therapies.
MACROLIDES
A pseudo-randomized, double-blind, placebo-controlled trial of 90 patients showed complete resolution of pityriasis rosea after six weeks in 73% of those treated with oral erythromycin.40 However, a larger open-label study of 184 patients followed for eight weeks was not able to replicate those findings.41 Studies of azithromycin (Zithromax) and clarithromycin (Biaxin) with six weeks of follow-up did not show benefit in the treatment of pityriasis rosea.42–44
ANTIVIRALS
Antiviral medications have been studied for the treatment of pityriasis rosea because of its link with HHV-6 and -7. Cidofovir (Vistide) and foscarnet may be effective against these viruses, but they have more adverse effects than acyclovir.45 In small studies with fewer than 100 patients, those who took acyclovir, 800 mg five times per day for seven days, had significant improvements in symptoms and lesion resolution.39,46–48 Lower doses (400 mg three to five times per day for seven days) also were effective in small randomized controlled trials that followed patients for up to four weeks.39,49 Two studies of acyclovir given in the first week after rash development had conflicting results.46,47 However, acyclovir appears to be a reasonable treatment option for severe cases of pityriasis rosea.
PHOTOTHERAPY
Two small studies found improvements in severity and symptoms in patients with pityriasis rosea who received ultraviolet B phototherapy multiple times per week for up to four weeks.50,51 Another study of 15 patients with extensive disease used low-dose ultraviolet A phototherapy two or three times per week until resolution or no further improvement of the rash.52 Most patients had notable improvement after the second or third treatment. Pruritus was reduced in 12 of 15 patients.
Pityriasis Rosea in Pregnancy
Pregnant women are more susceptible to pityriasis rosea because of their altered immune response.3 One case series of 61 pregnant women with pityriasis rosea found a 13% overall rate of spontaneous abortion. The rate was 57% in patients who developed pityriasis rosea in the first 15 weeks of gestation.53,54 Treatment with acyclovir can be considered,39 although more studies are needed to clarify its potential benefits.
This article updates a previous article on this topic by Stulberg and Wolfrey.1
Data Sources: PubMed Clinical Queries, Essential Evidence, UpToDate, and the Cochrane Database of Systematic Reviews were searched using the term pityriasis rosea. Search dates: October and November 2016, and August 2017.
