
Am Fam Physician. 2018;97(8):510-516
Author disclosure: No relevant financial affiliations.
Running is a common form of exercise but predisposes athletes to several running-related injuries. Most running injuries are due to overuse and respond to conservative treatment. Tendinopathies in the patellar, Achilles, and hamstring tendons are common, and are primarily treated with eccentric exercise. Iliotibial band syndrome and patellofemoral pain syndrome are less common than patellar tendinopathy and are treated by strengthening exercises for the core and legs in addition to flexibility exercises. Acute hamstring strains and medial tibial stress syndrome require a period of relative rest, followed by stretching and graded return to activity. Tibial stress fractures require an extended period of relative rest, followed by a more gradual return to activity. Early mobilization improves recovery from ankle sprains, and exercise therapy and functional bracing while running for six to 12 months prevents reinjury. Plantar fasciopathy (plantar fasciitis) can be significantly improved with stretching, heel raises, and orthoses that provide arch support.
Approximately 1% of Americans run on an average day, nearly twice as many as those who golf or cycle.1 Running is an excellent form of exercise; even at a slow pace, it is matched in metabolic equivalents only by vigorous swimming or cycling.2,3 However, injuries are common among runners (Table 1).4 A systematic review showed a one-year injury rate of 27% in novice runners, 32% in long distance runners, and 52% in marathon runners.5 The lower prevalence for novice runners seems to be secondary to less running time. Another systematic review found that novice runners were injured twice as often as recreational runners.6
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| Eccentric exercises are primary therapy for patellar and Achilles tendinopathies. | A | 11, 12, 14, 15 |
| Exercise therapy for patellofemoral pain should consist of core and leg strengthening as well as leg flexibility exercises. | A | 23 |
| Exercise therapy for iliotibial band syndrome should consist of hip abductor strengthening and hamstring and iliotibial band stretching. | B | 29 |
| Functional bracing while running should be continued for six to 12 months after an ankle sprain to improve stability and prevent recurrence. | A | 37 |
| Foot orthoses are beneficial for plantar fasciopathy (plantar fasciitis). There is no evidence that custom orthoses are superior to commercially available products. | A | 46, 47 |
| Eccentric exercises should be considered for treatment of hamstring tendinopathy. | C | 18, 54 |
| Recommendation | Sponsoring organization |
|---|---|
| Do not routinely order radiography for diagnosis of plantar fasciitis/heel pain in employees who stand or walk at work. | American College of Occupational and Environmental Medicine |
| Avoid ordering knee magnetic resonance imaging for a patient with anterior knee pain without mechanical symptoms or effusion unless the patient has not improved following completion of an appropriate functional rehabilitation program. | American Medical Society for Sports Medicine |
| Do not perform surgery for plantar fasciitis before trying six months of nonoperative care. | American Orthopaedic Foot and Ankle Society |
| Injury | Prevalence (%) |
|---|---|
| Knee | 28 |
| Patellar tendinopathy | 12 |
| Iliotibial band syndrome | 10 |
| Patellofemoral pain syndrome | 6 |
| Foot and ankle | 21 to 38 |
| Ankle sprain | 10 |
| Achilles tendinopathy | 6 to 9 |
| Plantar fasciopathy (plantar fasciitis) | 5 to 18 |
| Hamstring | 19 |
| Hamstring tendinopathy | 12 |
| Hamstring muscle injury | 7 |
| Tibia | 14 |
| Medial tibial stress syndrome | 10 |
| Tibial stress fracture | 4 |
About 80% of running injuries are due to overuse.4 Most involve the knee, hamstring, tibia, ankle, or plantar fascia.4 Common acute injuries include ankle sprains and hamstring strains. Studies show that women are at a significantly lower overall risk of running-related injuries.7 One study showed that women have an increased incidence of knee and plantar fascia injuries.8
Knee Injuries
PATELLAR TENDINOPATHY
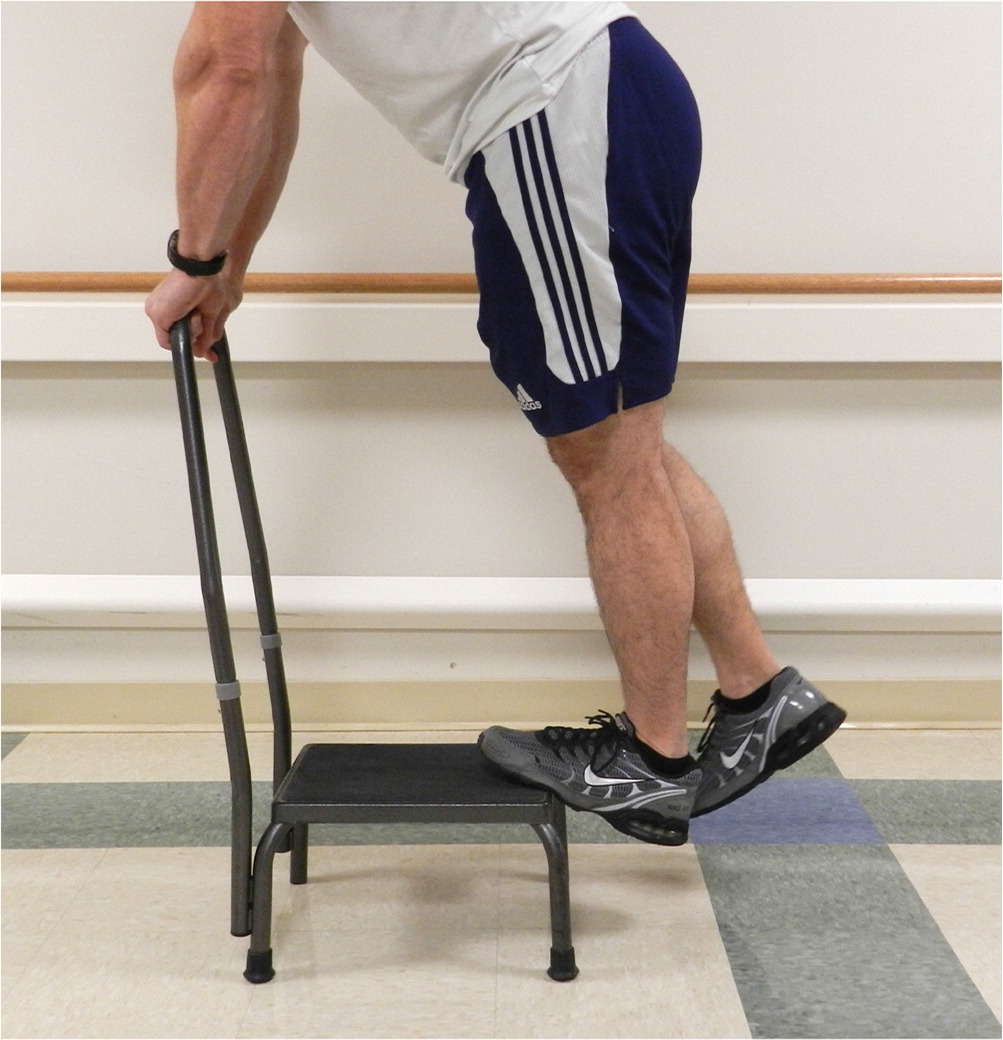
Patellar tendinopathy is the most common knee injury in runners.4 Patients experience anterior knee pain localized to the inferior patella and proximal patellar tendon, which is often tender on examination. Pain with a single-leg decline squat is also characteristic. To test for this, the patient should extend the unaffected knee, then squat with the affected leg to stress the patellar tendon9 (Figure 1). See a video of a single leg decline squat. Ultrasonography can provide a definitive diagnosis.10 A small study comparing physical examination with ultrasonography showed that characteristic history and painful single-leg decline squats each have a positive likelihood ratio (LR+) of 4 and a negative likelihood ratio (LR–) of 0.5 for patellar tendinopathy.11
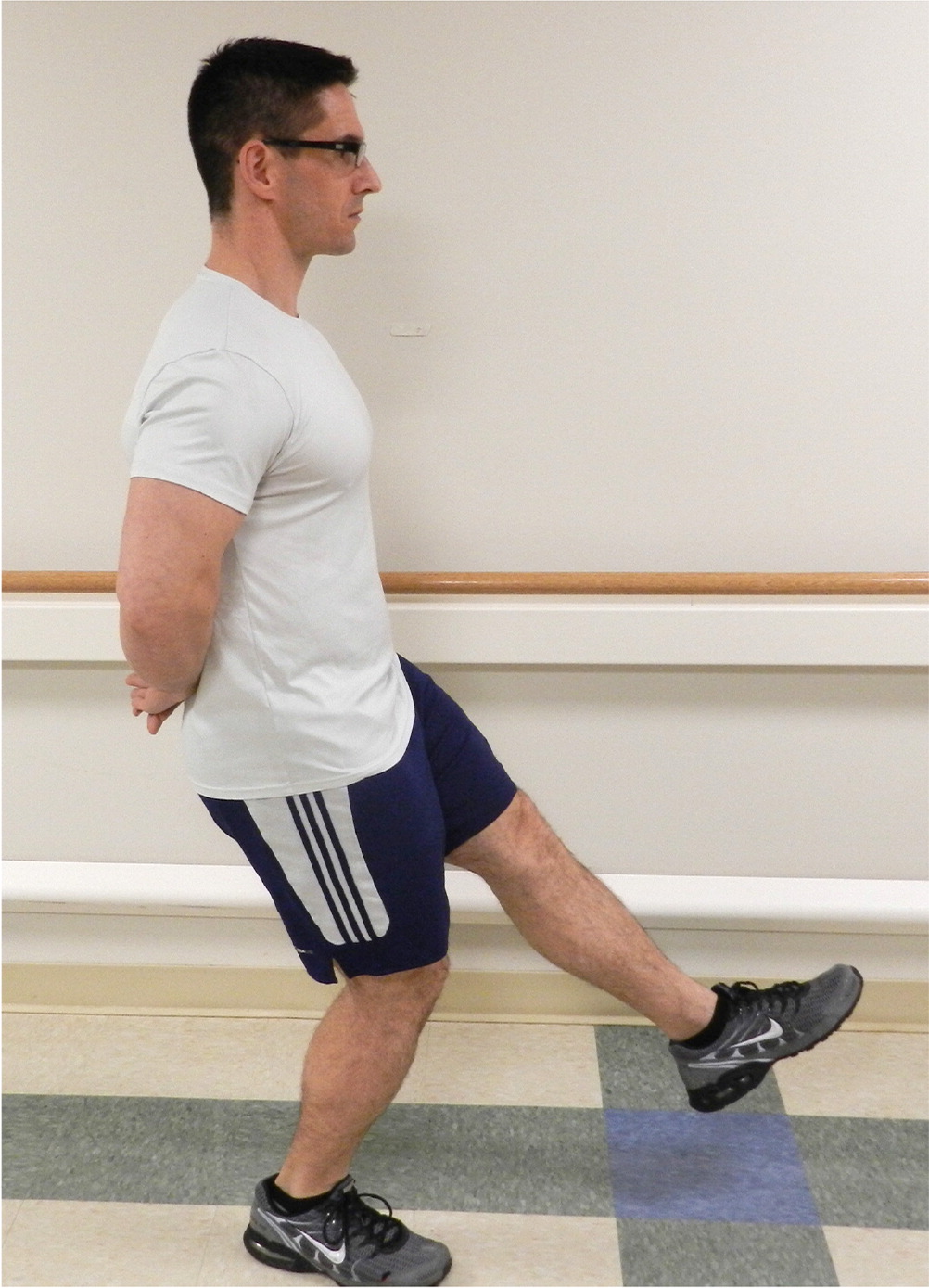
Single-Leg Decline Squat
Treatment is generally conservative and includes eccentric exercises (Table 2).12–18 Exercises should be performed on a decline board and should cause some discomfort.12 Patellar taping and extracorporeal shock wave therapy are not effective treatments for patellar tendinopathy.13 Surgery may be considered for patients whose symptoms do not improve after three months (up to 10% of patients).19 Data on surgical repair are limited, but a recent systematic review demonstrated significant symptom improvement.20
| Tendinopathy | Exercises |
|---|---|
| Achilles | Eccentric heel lowering: Standing on toes on a step, slowly lower heels below toes, then return. (For insertional Achilles tendinopathy, do not lower heels below toes.) |
| Hamstring | Single-leg squat: Flex and extend knee. |
| Lunges: Lower knee in large step. | |
| Nordic curls: From kneeling position, lower trunk forward while feet are held. | |
| Patellar | Decline knee bends: Flex and extend knees while standing on decline board. |
PATELLOFEMORAL PAIN SYNDROME
Patellofemoral pain syndrome is characterized by anterior knee pain, often behind the patella. Pain is worse after activities that stress the patellofemoral joint (e.g., climbing or descending stairs, squatting, running). Patients may report feelings of instability or crepitus. An effusion or history of trauma makes the diagnosis less likely.21 A small study showed that pain with squatting, kneeling, or resisted quadriceps contraction could indicate patellofemoral pain syndrome; the presence of any two of these findings has a LR+ of 4, whereas lack of pain with squatting has a LR– of 0.2.22 Table 3 lists signs and symptoms that differentiate patellar tendinopathy from patellofemoral pain syndrome.11,22
| Patellar tendinopathy | Patellofemoral pain syndrome |
|---|---|
| Symptoms | |
| Pain at inferior patellar pole | Pain location often nonspecific |
| Pain with jumping | Pain with stairs (usually more going down) |
| Pain with squatting | Pain with squatting |
| Theater sign: pain with standing after sitting for extended time | |
| Knee buckling/giving way with pain | |
| Examination findings | |
| No effusion, except inferior patella | No effusion |
| Pain with decline squat test | Pain with squatting, but not more with decline squat test |
| Tenderness at inferior patellar pole | No specific tenderness |
| Patellar compression pain (poor sensitivity) | |
| Patellar tilt pain (poor sensitivity) | |
Exercise is the mainstay of conservative treatment for patellofemoral pain syndrome. A systematic review found that the most effective treatment is six weeks of daily exercises focused on flexibility and leg and core strengthening.23 Taping the knee to reduce lateral pressure (McConnell taping), infrapatellar bands, knee braces, and therapeutic ultrasound have not been proven beneficial.24,25 A randomized controlled trial showed no difference when knee arthroscopy was added to home exercise in patients with patellofemoral pain syndrome.26 Nonsteroidal anti-inflammatory drugs provide short-term pain relief, but no benefit over placebo at three months.27
ILIOTIBIAL BAND SYNDROME
Iliotibial band syndrome causes lateral knee pain by impingement of the iliotibial band against the lateral femoral condyle when the knee is flexed 20 to 30 degrees.28 Pain is localized approximately 2 cm proximal to the lateral joint line, worsens with running, and may be associated with a popping sensation.29 Pain initially occurs later in runs, but progressively starts earlier or even at rest.30 The Noble compression test is diagnostic, although its accuracy has not been studied. Pressure is applied along the iliotibial band 2 cm proximal to the lateral femoral epicondyle, and the knee is passively flexed from 0 to 60 degrees (Figure 2). In a positive test, the patient experiences typical knee pain at 30 degrees of flexion.31 See a video of the Noble compression test.

Noble Compression Test
Treatment for iliotibial band syndrome is primarily exercise therapy focused on strengthening hip abductors and improving flexibility of the hamstring and iliotibial band.29 The combination of nonsteroidal anti-inflammatory drugs and stretching is superior to placebo and stretching.32 A small study of corticosteroid injections in runners showed reduced pain during running seven to 14 days after injection.33 Surgery is becoming more common when conservative measures are ineffective, but evidence is limited to case series.29
Foot and Ankle Injuries
ANKLE SPRAINS
Ankle sprains are common in runners. They typically result from ankle inversions that damage one or more of the lateral ankle ligaments. Initial evaluation should rule out fracture, using the Ottawa ankle and foot rules to determine whether radiography is necessary.34 Syndesmotic injury should be considered, although neither physical examination nor radiography is sufficiently sensitive to rule out this condition; magnetic resonance imaging (MRI) is preferred.35 PRICE (protection, rest, ice, compression, elevation) therapy is traditionally recommended, but a review of low-quality studies suggests that early mobilization leads to more rapid recovery than rest or immobilization.36 A meta-analysis of 46 systematic reviews of ankle sprain treatments suggests that functional bracing is the most important intervention for ankle sprain.37 Bracing (including taping, external support, and orthoses) is recommended during exercise for six to 12 months after injury to improve stability and prevent recurrence.37 The meta-analysis also found strong evidence that exercise therapy can help prevent recurrence.37 Information about managing ankle sprains is included in a previous American Family Physician article.34
ACHILLES TENDINOPATHY
Achilles tendinopathy presents as aching posterior heel pain. Most patients with this condition have midportion tendinopathy, with pain, swelling, and tenderness on the Achilles tendon 2 to 6 cm above its insertion into the calcaneus. Insertional Achilles tendinopathy accounts for 25% of cases, with pain and swelling at the insertion to the posterior calcaneus.38 Diagnosis can usually be made clinically, although ultrasonography and MRI effectively demonstrate pathologic changes and can show an occult tendon rupture.39
Treatment of Achilles tendinopathy consists of eccentric heel-lowering exercises (Table 2).12–18 For patients with mid-portion tendinopathy, this exercise should be performed with toes on a step so that the heel can be lowered below the toes14 (Figure 3). See a video of eccentric Achilles exercises. A small study found significant benefit from three months of eccentric exercise after five years, but only 40% of patients were completely pain free.15 Shock wave therapy has limited evidence of benefit, with improvement in patients with insertional tendinopathy but not for those with the more common midportion tendinopathy.40 Topical glyceryl trinitrate patches showed benefit over placebo in two studies, but no benefit vs. physical therapy in one smaller study.16 Injections and surgical techniques have insufficient evidence of benefit.16,41
Eccentric Achilles Exercises
PLANTAR FASCIOPATHY (PLANTAR FASCIITIS)
The plantar fascia is a band of connective tissue that spans from the medial tubercle of the calcaneus to the toes and provides static and dynamic stabilization of the medial longitudinal arch of the foot.42 Plantar fascia pain is typically located at the medial calcaneal tubercle, is worse with early morning ambulation, and improves with activity. Typical findings include tenderness over the medial calcaneal tubercle that extends along the plantar fascia, often with crepitus, thickness, or swelling.43 The Windlass test, in which the toes are passively extended, can elicit pain by stretching the fascia.43 Although the diagnosis of plantar fasciopathy is clinical, a plantar fascia thickness of more than 4 mm on ultrasonography or plain radiography can support the diagnosis.44 Radiography showing thickening of the plantar fascia and thinning or loss of the fat pad below the fascial insertion has 85% sensitivity and 95% specificity for plantar fasciopathy (LR+ = 17; LR– = 0.16).44 Calcaneal bone spurs are usually not associated with the plantar fascia and are not useful for diagnosis. Ultrasonography may show rupture of the plantar fascia.44
Many treatments have been proposed for plantar fasciopathy; passive stretching of the plantar fascia (e.g., pulling back toes with a hand or towel [Figure 4]) and active strength training (e.g., heel raises) are recommended. A small study showed that although strength training was more effective than passive stretching at three months, both were equally effective at six and 12 months.45 A meta-analysis showed that foot orthoses with arch support led to improvement in pain and function after 11 weeks.46 A Cochrane review found insufficient evidence that custom orthoses were more effective than a stretching and strengthening program or non-custom orthoses.47 A Cochrane review of low-quality trials suggested that local steroid injections reduce pain at one month but not afterward; data were insufficient to determine the effectiveness of other injected substances.48 Additional information about the management of plantar fasciopathy is included in a previous American Family Physician article.49

Hamstring Injuries
Hamstring injuries include acute strains and chronic tendinopathy. In both cases, the pain is more likely to be proximal. Acute strains present suddenly, often after sprinting.50 Strains can be accompanied by bruising or a palpable focal muscle defect.50 Plain radiography is not helpful unless avulsion of the ischial tuberosity is suspected.51 MRI can determine the injury severity and help estimate return to activity.51 Initial RICE (rest, ice, compression, elevation) is recommended but has not been studied.51 Acute strains require activity limitation until the patient can walk normally, followed by physical therapy in which range of motion is gradually increased.52
Hamstring tendinopathy presents as cramping pain in the posterior thigh or deep buttock with an insidious onset. Pain may radiate to the popliteal fossa and is worsened by running and sitting.53 Examination may show tenderness over the hamstring origin at the ischial tuberosity. A small study supports the modified bent-knee test, with a LR+ of 10.2 and a LR– of 0.12.17 In this test, the patient lies supine while the examiner lifts the leg to 90 degrees with the knee bent, then rapidly straightens the leg (see a video of the modified bent-knee test). Eccentric exercise is recommended based on evidence for other tendinopathies, but data for hamstring tendinopathy are limited to case reports.54 Exercises include the single-leg squat, lunges, and Nordic curls (Table 2).12–18 A survey of 38 patients showed that corticosteroid injections provided pain relief at one month in 50% of patients, and at six months in 24%.55
Modified Bent-Knee Test
Tibial Injuries
MEDIAL TIBIAL STRESS SYNDROME
Medial tibial stress syndrome (shin splints) is a common bone stress injury with tibial periostitis and microfractures over the anterior tibia.56 It typically presents with pain over the middle or distal one-third of the posteromedial tibial border. The most sensitive physical examination finding is tenderness to palpation over this area.57 Mild swelling over the area is also common. Exertional compartment syndrome can present with similar pain, but the pain resolves with rest and there is no tenderness at rest.58 Radiography is useful if a tibial stress fracture is suspected. MRI has been proven more sensitive and specific than bone scintigraphy for diagnosis of medial tibial stress syndrome and stress fracture.57
Treatment of medial tibial stress syndrome is conservative. Relative rest and calf stretching are recommended because evidence links tightness in the soleus and posterior tibialis to medial tibial stress syndrome.59 Although a recent systematic review showed no high-quality evidence for any alternative intervention, two small trials suggested possible benefit from extracorporeal shock wave therapy.59
TIBIAL STRESS FRACTURE
The tibia is the most common stress fracture site in runners, followed by the tarsal navicular, metatarsals, femur, and pelvis.60 Tibial stress fractures commonly occur with rapid increases in activity and are associated with the female athlete triad, in which bone density decreases as a result of poor nutrition and reduced estrogen levels.61 As with medial tibial stress syndrome, tibial stress fractures present with pain and tenderness on palpation, most commonly over the middle to distal one-third of the anterior tibia.57 Patients with significant pain or difficulty walking should undergo MRI.58
Treatment of tibial stress fractures involves a temporary (six to eight weeks) cessation of running, with continued weight bearing unless walking is painful. Return to activity should be slow and dependent on pain levels.61 Trials of pneumatic bracing, ultrasonography, and vitamin D supplementation have not shown consistent results.62 Surgery may be considered for failure of union. A systematic review found that athletes with tibial stress fractures can take three to 10 months to return to sports.63
Data Sources: PubMed searches were completed using the key terms running injuries and runners. After the major injuries were identified, searches were performed for each individual injury. The searches included systematic reviews, meta-analyses, randomized controlled trials, and review articles. We also searched the Cochrane database, Essential Evidence Plus, and Clinical Evidence. In addition, references in these resources were searched. Search dates: November and December 2016, and January 2017.
The views expressed in this article are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Department of Defense, or the U.S. government.
