
Am Fam Physician. 2018;98(1):40-46
Author disclosure: No relevant financial affiliations.
Medical decision-making capacity is the ability of a patient to understand the benefits and risks of, and the alternatives to, a proposed treatment or intervention (including no treatment). Capacity is the basis of informed consent. Patients have medical decision-making capacity if they can demonstrate understanding of the situation, appreciation of the consequences of their decision, and reasoning in their thought process, and if they can communicate their wishes. Capacity is assessed intuitively at every medical encounter and is usually readily apparent. However, a more formal capacity evaluation should be considered if there is reason to question a patient's decision-making abilities. Such reasons include an acute change in mental status, refusal of a clearly beneficial recommended treatment, risk factors for impaired decision making, or readily agreeing to an invasive or risky procedure without adequately considering the risks and benefits. Any physician can evaluate capacity, and a structured approach is best. Several formal assessment tools are available to help with the capacity evaluation. Consultation with a psychiatrist may be helpful in some cases, but the final determination on capacity is made by the treating physician. If a patient is found not to have capacity, a surrogate decision maker should be identified and consulted. If the patient is unable to give consent and identifying a surrogate decision maker will result in a delay that might increase the risk of death or serious harm, physicians can provide emergency care without formal consent.
Informed consent involves providing patients with accurate and adequate information about the risks, benefits, and alternatives of a treatment in a manner that is free from coercion. It also requires that patients have medical decision-making capacity. Medical decision-making capacity has four key elements. Patients must be able to (1) demonstrate understanding of the benefits and risks of, and the alternatives to, a proposed treatment or intervention (including no treatment); (2) demonstrate appreciation of those benefits, risks, and alternatives; (3) show reasoning in making a decision; and (4) communicate their choice.1,2
| Clinical recommendation | Evidence rating | References |
|---|---|---|
| A structured approach should be used when assessing a patient's decision-making capacity. This should include an assessment of any language or communication barriers interfering with the patient's understanding; identification and treatment of any reversible causes of incapacity; a directed interview to assess the elements of consent; and, if needed, the use of a formal tool to assess capacity and cognition. | C | 3, 7, 8 |
| Use of a formal assessment tool such as the Aid to Capacity Evaluation improves accuracy in determining a patient's decision-making capacity. | C | 2, 8 |
| Use of a standard cognitive assessment instrument is helpful in assessing for capacity when patients score at the extremes of the scale (very high score favors capacity and very low score favors incapacity). | C | 2, 15 |
Capacity differs from competence. Although the terms are often used interchangeably, competence is a legal term that is determined by the court system, whereas capacity is a medical term that is determined by the treating physician. According to their strict definitions, lack of competence refers to global decision-making impairment (e.g., finances, property, wills), whereas lack of capacity refers to the inability to make decisions about proposed medical treatments and other aspects of care. Capacity can vary with circumstance; for example, a patient can have the capacity to make small, straightforward decisions such as consenting to take a new medication, but may lack the capacity to consent to a high-risk abdominal surgery.3
Generally, a patient's capacity is readily apparent, and physicians intuitively assess capacity at every medical visit. Because the four elements of capacity (understanding, appreciation, reasoning, and communication) are built into everyday dialogue and interactions, it can be assumed that patients have the capacity to make medical decisions if their conversation demonstrates basic logic. However, a patient's capacity may come into question if the dialogue does not proceed in a logical fashion, if there are abrupt changes in the patient's mental status, or if the patient refuses an obviously beneficial treatment, has a risk factor for impaired decision making (Table 13–5), or readily agrees to an invasive or risky procedure without discussing or considering the risks and benefits.3 If the physician has doubts about a patient's ability to make a decision, a more formal evaluation of capacity should be undertaken. The results can either give the physician confidence to adhere to the patient's wishes or, if a lack of capacity is indicated, to take steps to restrict the patient's autonomy in order to prevent unintended and irreparable harm.
| Acknowledged fear of or discomfort with institutional health care setting |
| Age < 18 years |
| Age > 85 years |
| Chronic neurologic condition |
| Chronic psychiatric condition |
| Low education level |
| Significant cultural or language barrier |
Prevalence
Physicians tend to underdiagnose lack of capacity in their patients. An analysis of eight studies showed that physicians could identify only 42% of patients with incapacity as determined by a formal evaluation.2 It is not clear whether underdiagnosis is the result of physicians' inability to recognize incapacity or their reluctance to make the diagnosis.
Knowing the prevalence of incapacity in various populations may raise awareness by helping physicians determine the pretest probability. In populations with a higher pretest probability, physicians should be more alert for incapacity and more readily consider performing a capacity evaluation. The prevalence of incapacity in healthy older adults is estimated at 2.8%.6 However, the prevalence is higher in other patient populations: inpatients on a medical ward have an incapacity prevalence of 26%, and those with Alzheimer disease (considering those at all stages) have a prevalence of 54%.6 The highest rate (68%) is among persons with learning disabilities.6
Evaluation
INITIAL STEPS
The first step is to ensure that there are no communication barriers impairing the patient's ability to understand information and communicate with the physician. These might include physical barriers, such as hearing and vision impairments, dysarthria, or dysphagia.9 Language barriers may also be present, including the use of medical jargon that can confuse patients and cause “pseudo-incapacity.” 2 Jargon and complicated explanations can also cause confusion, but further inquiry and rewording can improve their understanding and allow them to make informed decisions.
If there are no communication barriers, the next step is to evaluate for reversible causes of incapacity, such as infection, medication adverse effects, illicit drug use, hypoxia, metabolic derangements, acute neurologic and psychiatric disorders, delirium, and critical illness. The third step is to consider the patient's values and culture; these can weigh heavily on his or her decision and may cause some physicians to question capacity. A Jehovah's Witness who refuses a blood transfusion is a classic example of a value-based decision that should be honored as long as the patient demonstrates the four elements of capacity.
DIRECTED CLINICAL INTERVIEW
If no communication barriers or reversible causes of incapacity are identified, the next step is a capacity assessment with a quick and informal directed clinical interview. This process can help determine whether the patient demonstrates the four elements of capacity. Table 2 provides suggested questions to use in evaluating these four elements.3 When evaluating a patient's responses to these questions, keep in mind that patients do not have to make the “right” choice; they need only to demonstrate a rational examination of pertinent information in arriving at their decision.10 A high burden of proof is needed to restrict autonomy. Therefore, if the evaluation indicates that the patient's understanding and rationale are adequate, that generally establishes capacity, even though someone else in the patient's situation might make a different decision.11
| Questions to determine the patient's ability to understand treatment and care options |
| What is your understanding of your condition? |
| What are the options for your situation? |
| What is your understanding of the benefits of treatment, and what are the odds that the treatment will work for you? |
| What are the risks of treatment, and what are the odds that you may have a side effect or bad outcome? |
| What is your understanding of what will happen if nothing is done? |
| Questions to determine the patient's ability to appreciate how that information applies to his or her own situation |
| Tell me what you really believe about your medical condition. |
| Why do you think your doctor has recommended (specific treatment/test) for you? |
| Do you think (specific treatment/test) is best for you? Why or why not? |
| What do you think will actually happen to you if you accept this treatment? If you don't accept it? |
| Questions to determine the patient's ability to reason with that information in a manner supported by the facts and the patient's own values |
| What factors/issues are most important to you in deciding about your treatment? What are you thinking about as you consider your decision? |
| How are you balancing the pluses and minuses of the treatments? |
| Do you trust your doctor? Why or why not? |
| What do you think will happen to you now? |
| Questions to determine the patient's ability to communicate and express a choice clearly |
| You have been given a lot of information about your condition. Have you decided what medical option is best for you right now? |
| We have discussed several choices. What do you want to do? |
FORMAL CAPACITY ASSESSMENT TOOLS
If the directed interview does not clearly demonstrate capacity, or if additional information is required, the use of a formal assessment tool is the next step. Several tools are available to evaluate capacity, and each has a unique approach. Common assessment tools include the Aid to Capacity Evaluation (ACE; Figure 13), the Hopkins Competency Assessment Test (HCAT; available at http://criminal-justice.iresearchnet.com/forensic-psychology/hopkins-competency-assessment-test-hcat), the Understanding Treatment Disclosure, and the MacArthur Competence Assessment Tool for Treatment.12
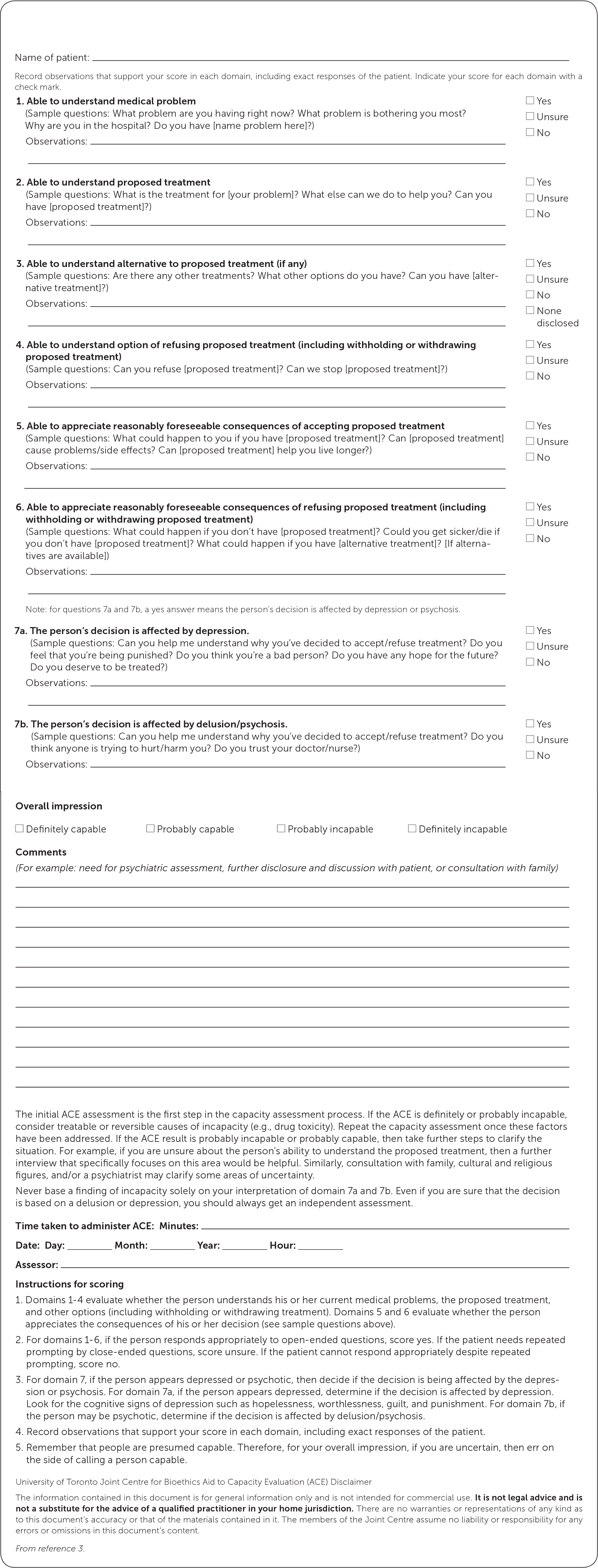
The ACE is a formal, directed, clinical interview that objectively assesses the four elements of capacity. It is widely used and considered the best available online tool. It comes with instructions and is specific to each medical decision. The ACE was validated in a large study that showed that a positive evaluation had a likelihood ratio of 8.5 for predicting decision-making incapacity.2,8
The HCAT is also quick and effective, but it evaluates for generalized incapacity rather than capacity to make specific decisions.13 The HCAT can be helpful if there is concern about the need to transfer decision-making authority to a surrogate, but it is not as helpful if the goal is evaluating for capacity in a specific clinical scenario.
If uncertainty about capacity remains after an evaluation using the ACE, HCAT, or other instrument, consultation with another clinician can be considered. Consultation with a psychiatrist can be particularly helpful and is prudent if the patient has a history of schizophrenia or other psychiatric or delusional disorder. However, the final determination of the patient's capacity should be made by the treating physician.
COGNITIVE TESTING
Assessing cognition can be useful but is not required to determine capacity. The Mini-Mental State Examination (available at https://www.uml.edu/docs/Mini%20Mental%20State%20Exam_tcm18-169319.pdf) and the Montreal Cognitive Assessment (available at http://www.mocatest.org) are two tools that are commonly used to evaluate cognition. They can be helpful in evaluating capacity when patients score at the extremes of the scoring scale.14 For example, patients who score less than 20 on the 30-point Mini-Mental State Examination are 6.3 times more likely to have incapacity, whereas patients who score 25 or higher are unlikely to have incapacity (likelihood ratio = 0.14).2 Similarly, the 30-point Montreal Cognitive Assessment has been shown to predict incapacity. In one study of 90 patients with Parkinson disease, a score of less than 22 had a 94% sensitivity and 90% specificity for identifying incapacity.15
FINAL DECISION
Determining that a patient lacks capacity and restricting his or her autonomy require clear and convincing evidence that the patient's decision will cause unintended and irreparable harm. If there is uncertainty after conducting a full capacity evaluation, the final judgment should err on the patient's side.4,16,17 Each state has its own definition of capacity. Although laws are similar among states and incorporate the four elements of capacity, there may be slight differences. Thus, if an evaluation leads to a diagnosis of incapacity and legal proceedings are involved, consultation with a medical attorney is prudent.
Surrogate Decision Makers
If a physician determines that a patient does not have the capacity to make a treatment decision, consent for treatment must be obtained from other sources. If the patient has an advance directive applicable to the clinical situation, it should be used to guide decisions. If not, the physician should determine whether the patient has designated a medical power of attorney. If there is no valid medical power of attorney, the closest relative usually becomes the surrogate. The priority of relatives varies by state, but the typical order is spouse, adult children, parents, siblings, and other relatives.
Up to 16% of patients in intensive care units do not have a known relative or medical power of attorney, so a court-appointed health fiduciary is an option.18 If the patient is not able to give consent and delaying care to identify a surrogate will increase the risk of death or serious harm, the physician can provide emergency care without formal consent under the assumption that a reasonable person would have consented to the treatment.4
Documentation
When performing a capacity assessment, it is important to document the evaluation in the medical record. Exact responses to the questions are helpful, along with a brief summary of the interview. If a formal assessment tool is used, it should be included in the medical record. Ultimately, the clinician must document the rationale used in determining the patient's capacity.3
Clinical Application
CASE 1
An 88-year-old woman who lives alone presents to the emergency department after a fall. Her sodium level is 120 mEq per L (120 mmol per L), and she is admitted to the hospital. Her outpatient records show that she has not refilled her heart failure medications in more than six months. On day 3 of hospitalization, she states that she is feeling better and wants to go home. Physical examination reveals global muscle weakness and inability to get out of bed without assistance. The inpatient team recommends transfer to a rehabilitation facility, but the patient refuses.
CASE 2
A 56-year-old man with schizophrenia is brought to the emergency department by his brother. He has a large, non-healing ulcer on his left lower leg that is obviously infected. His brother reports that the patient has diabetes mellitus and stopped taking his medications six months ago. On examination, the patient demonstrates disorganized thinking and describes auditory hallucinations. He refuses treatment and says the government is trying to kill him.
CASE DISCUSSION
Case 1 is an example of a patient who may understand her situation and treatment options, but may not appreciate the consequences of her decision. If she is discharged home, where she lives by herself, she will not be able to perform activities of daily living. She does not realize that this will lead to harm. From this informal assessment, she seems to lack appropriate decision-making capacity. A formal assessment using the ACE will likely confirm this conclusion. If she continues to insist on hospital discharge, steps can be taken to involve family members or other surrogate decision makers to arrive at a decision that will be acceptable to the patient and is appropriate for her safety.
Case 2 is an example of poor reasoning due to psychiatric illness. The patient cannot synthesize complex data to make an informed decision; therefore, he lacks decision-making capacity. Psychiatric consultation should be obtained and appropriate treatment instituted.
Data Sources: A literature search was performed in PubMed using the terms capacity and evaluating capacity. We also searched the National Guideline Clearinghouse and the Cochrane database. Search date: January 2017.
The opinions or assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the Department of Defense.
