
Am Fam Physician. 2018;98(12):738-744
Patient information: See related handout on school absences, written by the authors of this article.
Author disclosure: No relevant financial affiliations.
Frequent school absenteeism has immediate and long-term negative effects on academic performance, social functioning, high school and college graduation rates, adult income, health, and life expectancy. Previous research focused on distinguishing between truancy and anxiety-driven school refusal, but current policy has shifted to reducing absenteeism for any reason. Chronic absenteeism appears to be driven by overlapping medical, individual, family, and social factors, including chronic illness, mental health conditions, bullying, perceived lack of safety, health problems or needs of other family members, inconsistent parenting, poor school climate, economic disadvantage, and unreliable transportation. Family physicians are well positioned to identify patients with frequent absences, intervene early, and tailor treatment plans to the patient’s medical and social needs. Informing parents of the link between school attendance and achievement can be effective in reducing absences. If absenteeism is caused by chronic illness, management should include clear expectations about school attendance and care coordination with school personnel. Mental health conditions that interfere with school attendance can often be treated with cognitive behavior therapy and/or pharmacotherapy. When assessing a child with frequent absences, physicians should inquire about bullying, even if the patient is not known to identify with a vulnerable group. Families and schools are key collaborators in interventions via parent education, parental mental health treatment, and school-based intervention programs.
Frequent school absences are associated with lifelong negative academic, social, and health sequelae,1,2 yet often go unnoticed and unaddressed by schools and government organizations.3 School absenteeism has been called a public health issue and a hidden educational crisis.4,5 It is a complex and varied phenomenon with often interrelated causes. Interventions to reduce absenteeism previously focused on distinguishing truancy from excused absences because of anxiety-driven school refusal. However, recent evidence has shown that missing school is often detrimental even with the permission of parents or physicians,3 and the emphasis has shifted to reducing absenteeism for any reason.6
| Clinical recommendation | Evidence rating | References | |
|---|---|---|---|
| Parents should be informed about the connection between regular school attendance in early grades and academic success. | C | 42, 43 | |
| Physicians can use well-child visits to prepare families for kindergarten (e.g., establishing bedtime and morning routines) and to recommend preschool to families with risk factors for absenteeism. | C | 23, 45, 46 | |
| To address absenteeism in children with chronic illness, physicians should set expectations for regular school attendance; make a written action plan including an individualized emergency protocol, medication list, monitoring instructions, environmental triggers, and emergency contact information; and offer ongoing consultation. | C | 56, 57 | |
| For children with serious illness who need to miss school for treatment, physicians should discuss the likely timeframe for returning, then communicate with school personnel about the patient’s needs once he or she has returned to school. | C | 61 | |
| For children with academic and behavior problems, physicians should ensure that parents are aware of available school-based educational support services, and consider referral for mentoring and cognitive support. | C | 48 | |
| For children with depression or anxiety who miss school: | |||
| Physicians should recommend cognitive behavior therapy or other psychotherapy focused on a graduated return to school. | A | 47 | |
| Physicians should consider prescribing a selective serotonin reuptake inhibitor or serotonin-norepinephrine reuptake inhibitor. | A | 49 | |
| Physicians should recommend family involvement in therapy. | C | 50, 66 | |
| Physicians should connect students with school-based mental health resources when available. | C | 53 | |
| Physicians should screen and treat mothers of school-aged children for depression. | A | 31, 51, 67 | |
Epidemiology
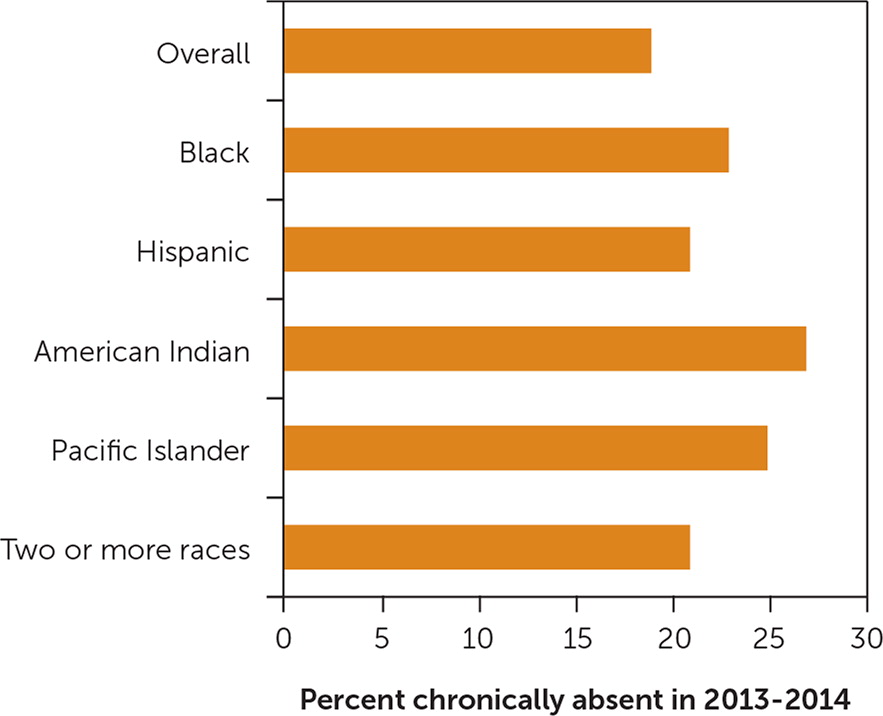
A recent national survey found that 14% of students—or about 6.8 million children and adolescents in kindergarten through 12th grade—are chronically absent, defined as missing at least 10% of the school year (about 18 days).5 Although absenteeism is often perceived as a high school problem, one-half of chronically absent students are enrolled in elementary and middle schools.7 Nationally, 10% of kindergarteners and first graders are chronically absent.8 Rates of chronic absenteeism between states, school districts, and even schools within a district vary from less than 5% to more than 50%.9 Although some of the highest rates occur in urban, heavily nonwhite schools, high rates can also occur in rural, mostly white districts.7 In at least one state, the age distribution is U-shaped, with rates of absenteeism fairly high in kindergarten, decreasing to their lowest point in fifth grade, and then increasing between sixth and 12th grades.10 National rates are similar for males and females, although their reasons for being absent may differ.11 English-speaking learners are somewhat less likely to be chronically absent than their non–English-speaking peers, and students with disabilities are 1.5 times more likely to be chronically absent.12 Students of Native American and Pacific Islander descent are 65% more likely than white students to miss three or more weeks of school, black students are 36% more likely, and Hispanic students are 11% more likely (Figure 1).12
Sequelae
Children who frequently miss school for any reason are at risk of low academic achievement, social problems, risky health behaviors, dropping out of school, nonenrollment in college, and related adult sequelae such as lower income, frequent work absences, and poorer health.1,4,13–17 High levels of absenteeism as early as kindergarten are associated with long-term consequences, including low reading proficiency in third grade and low academic achievement in fifth grade, which correlate with lower rates of high school graduation and college enrollment.7,8 Frequent absences are associated with negative outcomes for children of all socioeconomic groups.18 However, absenteeism perpetuates economic and social disadvantages in children from lower socioeconomic backgrounds.19,20
Etiology
Illness is the most commonly reported reason for absences, but children who are frequently absent often do not have a chronic disease and may not be ill. In one study of frequently absent students, more than 40% of those reporting an absence due to illness or injury were actually home for other reasons, such as transportation problems, family activities, or parental illness.21 Absences are often driven by overlapping individual, medical, family, and social factors (Table 1).4,8,10–13,15,19,22–37 A greater number of risk factors is associated with a higher frequency of absences.29
| Individual factors |
| Bullying 8 or perceived lack of safety at school 22 |
| Chronic illness (e.g., asthma, diabetes mellitus, obesity) 12 |
| Did not attend center-based preschool 23 |
| Disability 12 or special education4 |
| Exposure to tobacco smoke (in children with asthma) 24 |
| Exposure to violence 25 |
| History of frequent absences 4 |
| Lack of access to medical or dental care 12 |
| Low academic achievement 10 |
| Mental health conditions (e.g., attention-deficit/hyperactivity disorder, anxiety, depression, behavioral problems) 26–28 |
| Pregnancy or parenthood 29 |
| Sleep deficiency 30 |
| Substance use 22 |
| Family factors |
| Child has caregiving responsibilities at home 11 |
| Food insecurity 4 |
| Health problems in family members,15 including persistent maternal depression 31 |
| Housing instability 10 or homelessness 19 |
| Lack of structure or supervision 32 |
| Parent did not go to college 29 |
| Parent had negative school experiences and thinks missing school is acceptable 19 |
| Parent is incarcerated 33 |
| Parent is unemployed 34 |
| Parent works night shift or multiple jobs 13 |
| School and community factors |
| Cultural barriers 19 |
| Economic disadvantage 12 |
| Member of socially vulnerable group (e.g., lesbian, gay, bisexual, transgender) 35 |
| Nonwhite race 12 |
| School factors (e.g., poor school climate,8 no school nurse,36 air pollution/lack of green space 37) |
| Unreliable school transportation 15 |
| Unsafe route to school 8 |
Assessment
Attendance Works, a national school attendance advocacy organization, considers any child who misses more than 5% of school days (about nine days per year) to be at risk of academic and social problems.7 The early grades are a critical period of engagement with the educational process, and full engagement is associated with academic and social success.38 Any of the risk factors for chronic absenteeism can weaken a child’s engagement in education, and the presence of multiple risk factors significantly increases the risk of absences. Even excused absences may cause the child to fall behind academically and lose connections with peers and supportive school personnel. This disengagement makes attendance less rewarding and more anxiety provoking, and can lead to chronic absenteeism and school dropout. Physicians can best intervene when absences begin.39 Although no standardized screening tool is available, physicians should consider asking children and their guardians about frequent absences during well-child visits and preparticipation sports physicals. Requests for school excuse notes should also trigger further inquiry about absences.
Assessment of a child with frequent absences should include inquiries about the family and school environments, as well as the child’s history (Table 2).4,8,10–12,19,26–28,31–33,35–37 Frequent absences are often driven by more than one factor. For example, a student may have academic or social problems at school, leading to anxiety that causes him or her to stay home due to a stomachache. Another student may worry that his undocumented immigrant status will be discovered at school, and he may simultaneously be disengaged because of cultural barriers. A child who lacks appropriate adult supervision and adequate food may arrive at school late and hungry, and she may be less able to focus on academics or self-regulate her emotions, leading to behavioral problems and suspension. A child with diabetes mellitus who attends a school without a nurse may often feel ill and leave school early. Physicians caring for such children must ensure that they have a full understanding of their patient’s medical, family, and social contexts.
| Perform physical examination and mental status examination; obtain student’s medical history and student’s and family’s psychiatric history 12,26–28,31 |
| Obtain information from school about student’s attendance and adjustment 4 |
Obtain information about:
|
| Administer the School Refusal Assessment Scale-Revised (http://www.oxfordclinicalpsych.com/view/10.1093/med:psych/9780195308297.001.0001/med-9780195308297-interactive-pdf-004.pdf) |
| Consider assessment for anxiety or depression, or referral to mental health professional 26,28 |
The School Refusal Assessment Scale-Revised (available at http://www.oxfordclinicalpsych.com/view/10.1093/med:psych/9780195308297.001.0001/med-9780195308297-interactive-pdf-004.pdf) is a self- and parent-report inventory with good test-retest reliability and internal consistency, and may be helpful to physicians investigating the emotional reasons behind frequent absences.40,41
Prevention
There is some evidence that simply informing parents about the link between attendance and academic achievement reduces absences. Schools reported reduced absences after sending postcards that informed kindergarten parents of this connection and included the number of days their child had missed.42,43 Physicians can use waiting room materials and prekindergarten well-child visits to preemptively educate parents about the link between early school attendance and academic success.
A recent longitudinal study of more than 14,000 children found that even when controlling for socioeconomic status, children who participated in center-based prekindergarten were less likely to be chronically absent the following year.23 Prekindergarten provides early exposure to a setting similar to kindergarten, allowing the family to become accustomed to the school routine. Physicians can encourage families with risk factors for chronic absenteeism to consider center-based preschool, which may also provide early identification and remediation of problems associated with absenteeism later on.44 Preschool-age well visits can also be an opportunity for physicians to help families prepare for the transition to kindergarten (e.g., planning bedtime and morning routines).45,46
Interventions
| Individual interventions |
| Cognitive behavior therapy 47 |
| Mentoring48 |
| Pharmacotherapy 49 |
| Preschool developmental and behavioral support 44 |
| Family interventions |
| Family involvement in therapy 50 |
| Parental education 42 |
| Support for parental mental health (e.g., treatment for depression) 31,51 |
| School and community interventions |
| Access to medical care 13 |
| Center-based preschool programs 23 |
| Collaboration between schools and medical professionals 6 |
| Community schools 19 |
| Parental education campaigns43 |
| Safe and reliable transportation52 |
| School-based mental health programs53 |
| School-based support for vulnerable and at-risk populations54 |
| School nurse interventions55 |
CHRONIC ILLNESS
Physicians can help children with chronic illnesses such as asthma, obesity, and diabetes by reinforcing the importance of regular school attendance 56; providing written action plans, including an individualized emergency protocol, medication list, monitoring instructions, environmental triggers, and emergency contact information; and offering ongoing consultation.57 Physicians can also increase school attendance for chronically ill children by consulting with schools. The Centers for Disease Control and Prevention notes that physicians can improve the health of children with asthma by serving as consultants to school multidisciplinary teams.58 Consulting physicians provided standing orders for albuterol administration to symptomatic children, consulted with school nurses about emergent or refractory cases, and provided extra training to nurses. This model resulted in a statistically significant reduction in missed school days for children with asthma and for students overall, regardless of health status.59
Physicians can also collaborate with school nurses to support school attendance for their patients. Attendance records for more than 10,000 elementary school students showed that students were more likely to attend school when a full-time nurse was available.36 A hospital-funded, school-based program in Michigan significantly reduced absenteeism when school nurses used hospital resources and staff to help manage students’ chronic medical conditions.55
SERIOUS ILLNESS
Serious illnesses such as cancer may cause even previously well-functioning children to have trouble returning to school.60,61 Physicians should discuss the likely timeframe for returning at the time of diagnosis of any serious illness that requires school withdrawal.62 After the child returns to school, the physician should communicate with school personnel about the patient’s needs and to ensure that the transition back to school is successful.
ACADEMIC CHALLENGES
The prevalence of absenteeism is higher in students with disabilities or low academic achievement. Physicians should monitor school attendance in these patients, ensure that parents are aware of available school-based educational support services, and consider referral for mentoring and cognitive support.48
MENTAL HEALTH AND BEHAVIORAL PROBLEMS
Anxiety is often a factor in frequent absences, even if other factors such as chronic illness are also present. A 2015 Cochrane review showed that cognitive behavior therapy is an effective treatment for anxiety in children; however, the evidence was inconclusive about the best method of therapy.47 Smaller studies of other behavioral interventions, including emotional-focused cognitive behavior therapy, parent training, and dialectical behavioral therapy, also showed positive effects on anxiety related to school refusal.50,63,64
The selective serotonin reuptake inhibitors fluoxetine (Prozac), paroxetine (Paxil), fluvoxamine, and sertraline (Zoloft), as well as one serotonin-norepinephrine reuptake inhibitor (venlafaxine), reduce symptoms of anxiety compared with placebo.49 Referral to a child psychiatrist is recommended when symptoms do not respond to pharmacotherapy. Family involvement in treatment is important for students in whom mental health conditions affect school attendance. Even if the primary problem is not emotional (e.g., an academic problem or illness), school absences are often reinforced by the benefits of staying home, such as parental attention, free time, and respite from academic or social challenges.65 Parents may benefit from family therapy to learn methods to encourage school attendance. Family therapy is also effective for behavioral problems that can interfere with school attendance.66
Physicians should connect students who have frequent absenteeism with school-based mental health services, especially if behavioral problems interfere with attendance. The results of a quasi-experimental study evaluating school-related outcomes of an expanded school mental health model showed reduced suspensions and improved attendance in 159 students who received in-school therapy from a community mental health clinician for one year, compared with 148 students who received services from guidance and school counselors.53
PARENTING PROBLEMS
Persistent maternal depression is associated with increased school absences in their children.31,51 This condition is highly treatable, and physicians should consider administering a simple depression screen to parents at the kindergarten well-child visit and initiating treatment when indicated.67 Physicians should refer families with parenting concerns to family therapy, in-home visits, or parenting classes.19
BULLYING AND VICTIMIZATION
Students who identify with socially vulnerable groups may feel unsafe and avoid school. Lesbian, gay, bisexual, transgender, and queer students who experience victimization in school are more likely to have increased absences. A study of school-based support for 7,261 lesbian, gay, bisexual, and transgender students showed a positive association between attendance and the presence of supportive school personnel.54 Physicians may benefit victimized students by encouraging them to alert a supportive adult at school, or by offering to contact that person directly. Physicians should inquire about bullying when assessing a child with frequent absences, even if the child is not known to identify with a socially vulnerable group. Additional strategies for helping children and adolescents prevent bullying are available in a recent article in American Family Physician.68
SOCIAL STRESSORS
Data Sources: A PubMed search was conducted using the key terms school refusal, absenteeism, and truancy. The search included meta-analyses, randomized controlled trials, clinical trials, and reviews. The Cochrane database, PsychINFO, the Agency for Healthcare Research and Quality evidence reports, the Oxford Clinical Psychology Treatments that Work database, and Clinical Evidence were also searched. Search dates: January 21, 2018, and August 10, 2018.
