
Am Fam Physician. 2019;99(11):682-688
Author disclosure: No relevant financial affiliations.
Varicose veins are twisted, dilated veins most commonly located on the lower extremities. The exact pathophysiology is debated, but it involves a genetic predisposition, incompetent valves, weakened vascular walls, and increased intravenous pressure. Risk factors include family history of venous disease; female sex; older age; chronically increased intra-abdominal pressure due to obesity, pregnancy, chronic constipation, or a tumor; and prolonged standing. Symptoms of varicose veins include a heavy, achy feeling and an itching or burning sensation; these symptoms worsen with prolonged standing. Potential complications include infection, leg ulcers, stasis changes, and thrombosis. Conservative treatment options include external compression; lifestyle modifications, such as avoidance of prolonged standing and straining, exercise, wearing nonrestrictive clothing, modification of cardiovascular risk factors, and interventions to reduce peripheral edema; elevation of the affected leg; weight loss; and medical therapy. There is not enough evidence to determine if compression stockings are effective in the treatment of varicose veins in the absence of active or healed venous ulcers. Interventional treatments include external laser thermal ablation, endovenous thermal ablation, endovenous sclerotherapy, and surgery. Although surgery was once the standard of care, it largely has been replaced by endovenous thermal ablation, which can be performed under local anesthesia and may have better outcomes and fewer complications than other treatments. Existing evidence and clinical guidelines suggest that a trial of compression therapy is not warranted before referral for endovenous thermal ablation, although it may be necessary for insurance coverage.
Varicose veins are subcutaneous veins dilated to at least 3 mm in diameter when measured with the patient in an upright position. They are part of a continuum of chronic venous disorders ranging from fine telangiectasias, also called spider veins, (less than 1 mm; Figure 1) and reticular veins (1 to 3 mm; Figure 1) to chronic venous insufficiency, which may include edema, hyperpigmentation, and venous ulcers. Chronic venous disease is most commonly described using the CEAP (clinical, etiologic, anatomic, pathophysiologic) classification system (Table 1).1
| Clinical recommendation | Evidence rating | References | Comments |
|---|---|---|---|
| There is not enough evidence to determine if compression stockings are effective in the treatment of varicose veins in the absence of active or healed venous ulcers. | B | 7, 15, 19–21 | Based on a Cochrane review and clinical guidelines based on systematic reviews; consensus guidelines and expert opinion |
| Horse chestnut seed extract (Aesculus hippocastanum) and other phlebotonics may ease the symptoms of varicose veins, but long-term studies of the safety and effectiveness of phlebotonics are lacking. | B | 23–25 | Based on systematic reviews/Cochrane review of lower-quality RCTs |
| Referral for interventional treatment of symptomatic varicose veins in nonpregnant patients should not be delayed for a trial of external compression. Interventional treatment should be offered if valvular reflux is documented. | C | 7, 15 | Clinical guidelines based on systematic reviews; consensus guidelines and expert opinion |
| Endovascular laser ablation may be better tolerated than sclerotherapy and surgery, with fewer adverse effects and equal effectiveness. | B | 30, 31 | Based on a Cochrane review of lower-quality RCTs and an RCT on quality-of-life outcomes |
| Classification | Description |
|---|---|
| Clinical* | |
| C0 | No visible or palpable signs of venous disease |
| C1 | Telangiectasias or reticular veins |
| C2 | Varicose veins |
| C3 | Edema |
| C4a | Pigmentation or eczema |
| C4b | Lipodermatosclerosis or atrophie blanche |
| C5 | Healed venous ulcer |
| C6 | Active venous ulcer |
| Etiologic | |
| Ec | Congenital |
| Ep | Primary |
| Es | Secondary (postthrombotic) |
| En | No venous cause identified |
| Anatomic | |
| As | Superficial veins |
| Ap | Perforating veins |
| Ad | Deep veins |
| An | No venous location identified |
| Pathophysiologic | |
| Pr | Reflux |
| Po | Obstruction |
| Pr,o | Reflux and obstruction |
| Pn | No venous pathophysiology identifiable |
Varicose veins are common on the lower extremities, with widely varying estimates of prevalence.2 A recent study found that telangiectasias occur in 43% of men and 55% of women, and varicose veins occur in 16% of men and 29% of women.3 In a population with a mean age of 60 years, the prevalence of CEAP classification C0 to C6 is 29%, 29%, 23%, 10%, 9%, 1.5%, and 0.5%, respectively.4
Etiology
Venous disease resulting in valvular reflux appears to be the underlying cause of varicose veins.5 The exact pathophysiology is debated, but it involves a genetic predisposition, incompetent valves, weakened vascular walls, and increased intravenous pressure. In most cases, the valvular dysfunction is presumed to be caused by a loss of elasticity in the vein wall, with failure of the valve leaflets to fit together. Rather than blood flowing from distal to proximal and superficial to deep, failed or incompetent valves allow blood to flow in the reverse direction. With increased pressure on the affected venous system, the larger veins may become elongated and tortuous. Shear stress on venous endothelial cells due to reversed or turbulent blood flow and inflammation are also important etiologic factors for venous disease.6
Varicose veins in the legs may involve the main axial superficial veins (the great saphenous vein and the small saphenous vein or their superficial tributaries).7 Established risk factors for varicose veins include family history of venous disease; female sex; older age; chronically increased intra-abdominal pressure due to obesity, pregnancy, chronic constipation, or a tumor; prolonged standing; deep venous thrombosis causing damage to valves and secondary revascularization; and arteriovenous shunting.8,9
Diagnosis
CLINICAL PRESENTATION
The clinical presentation of varicose veins varies, and some patients may be asymptomatic.10 Localized symptoms may be unilateral or bilateral and include pain, burning, itching, and tingling at the site of the varicose veins. Generalized symptoms consist of aching, heaviness, cramping, throbbing, restlessness, and swelling in the legs.7,11 Symptoms are often worse at the end of the day, especially after prolonged standing, and usually resolve when patients sit and elevate their legs. Women are significantly more likely than men to report lower limb symptoms.12 Patients are more likely to have symptoms and increasing severity of symptoms with increasing CEAP clinical class (C0 to C6).6
Although varicose veins may cause varying degrees of discomfort or cosmetic concern, they are rarely associated with significant complications. Signs of a more serious underlying vascular insufficiency may include changes in skin pigmentation, eczema, infection, superficial thrombophlebitis, venous ulceration, loss of subcutaneous tissue, and lipodermatosclerosis (a decrease in lower leg circumference due to chronic inflammation, fibrosis, and contraction of the skin and subcutaneous tissues). Although rare, hemodynamically significant external hemorrhage resulting from the perforation of a varicose vein has been reported.13
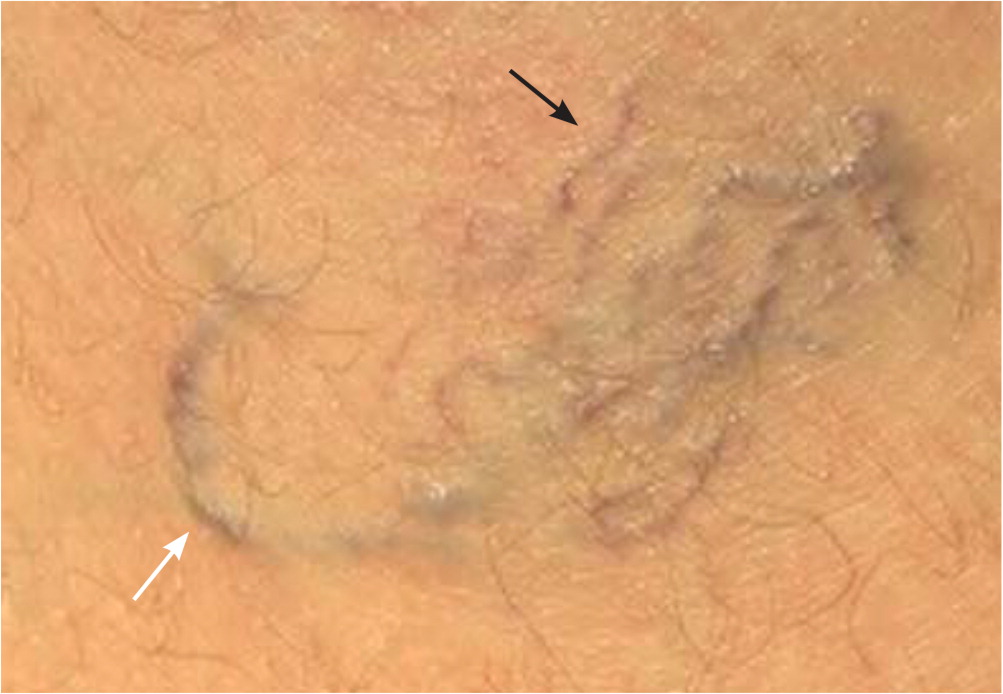
Evaluation of patient risk factors, symptoms, and typical physical examination findings helps determine a diagnosis. Through inspection and palpation, the examiner should note the size and distribution of varicose veins, the presence and type of edema, and the presence of skin discoloration, excoriation, or ulceration. Fan-shaped varicose veins in the ankle (corona phlebectatica; Figure 2) are considered an early sign of advanced venous disease. Decreased ankle mobility, atrophie blanche (a circular whitish area of scar tissue surrounded by dilated capillaries), and lipodermatosclerosis are also signs of advanced venous disease.1 Noting locations of other varicosities is important. Perineal, vulvar, or groin varicosities may be a sign of pelvic vein incompetence or obstruction, which may include abdominal, pelvic, or renal masses.7 Bedside clinical tests used to detect the site of reflux, such as palpation for a retrograde transmitted impulse from the saphenofemoral junction through the long saphenous vein (tap test) or for transmission of a thrill or impulse with coughing at the saphenofemoral junction (cough test), are of limited value because of their poor sensitivity or specificity.14

IMAGING STUDIES
When venous disease is severe or interventional therapy is being considered, venous duplex ultrasonography is the modality of choice.7,15 Duplex ultrasonography is a simple, noninvasive, painless, and readily available modality that can assess the anatomy and physiology of the lower extremity venous system. It can help determine which saphenous junctions are incompetent, the diameter of the junctions, the extent of reflux, and the location and size of other incompetent perforating veins. It can also assess for acute and occult deep venous thrombosis and superficial thrombophlebitis. Reflux is defined as a retrograde flow duration of more than 350 milliseconds in the perforating veins, more than 500 milliseconds in the superficial and deep calf veins, and more than 1,000 milliseconds in the femoropopliteal veins.16,17 Other imaging modalities, such as computed tomography, magnetic resonance imaging, venography, and plethysmography, are used only if venous ultrasonography is inconclusive or for more complex surgical situations.7
Treatment
Use of the CEAP classification system is important for diagnosis but does not provide guidance for treatment decisions. Treatment options for varicose veins include conservative management and interventional therapies such as thermal ablation, endovenous sclerotherapy, and surgery (Table 2).7,15,18 The decision to proceed with treatment and the choice of treatment are based on symptoms and patient preferences. Other considerations include cost, potential for complications, availability of resources, insurance reimbursement, and physician training. The presence or absence of deep venous insufficiency and the characteristics of the affected veins can also help guide treatment.17
| Treatment | Comments | |
|---|---|---|
| Conservative measures | ||
| Compression (e.g., bandages, support stockings, intermittent pneumatic compression devices) | Compression stockings can provide relief from discomfort, although evidence is lacking; external compression is first-line treatment only in pregnant women | |
| Elevation of the affected leg | May improve symptoms in some patients | |
| Lifestyle modifications | Examples include avoidance of prolonged standing and straining, exercise, wearing nonrestrictive clothing, modification of cardiovascular risk factors, and interventions to reduce peripheral edema | |
| Weight loss | Weight loss may improve symptoms in patients who are obese | |
| Phlebotonics | Most are available as dietary supplements (often with multiple agents in one supplement) and are sold over the counter in the United States; horse chestnut seed extract (Aesculus hippocastanum) may provide symptomatic relief, but long-term studies are lacking | |
| Interventional | ||
| Thermal ablation | ||
| External laser thermal ablation | Works best for telangiectasias | |
| Endovenous thermal ablation (using a laser or radio waves) | Used for larger vessels, including the greater saphenous vein | |
| Endovenous sclerotherapy | A variety of agents may be used, including hypertonic saline, sodium tetradecyl (Sotradecol), and polidocanol (Varithena) | |
| Surgery (ligation and stripping or phlebectomy with multiple small incisions) | Although surgery has historically been the most widely recommended treatment option, a growing body of literature does not consistently support surgery as the best interventional treatment option; updated surgical techniques use small incisions to reduce scarring, blood loss, and complications and limit removal of the superficial axial veins from the groin to knee, and may be performed under local or regional anesthesia | |
Over the past 10 years, there has been a significant change in the recommendations for treatment of symptomatic varicose veins. This is in large part because of the lack of evidence supporting the use of compression stockings and the rise of minimally invasive endovascular techniques.
CONSERVATIVE MANAGEMENT
Conservative treatment options include external compression; lifestyle modifications, such as avoidance of prolonged standing and straining, exercise, wearing nonrestrictive clothing, modification of cardiovascular risk factors, and interventions to reduce peripheral edema; elevation of the affected leg; weight loss; and phlebotonics. These measures are recommended for patients who are not candidates for endovenous or surgical management, do not desire intervention, or are pregnant.7,15
Compression has long been recommended as initial therapy for varicose veins. However, there is not enough evidence to determine if compression stockings are effective in the treatment of varicose veins in the absence of active or healed venous ulcers.7,19–21 The 2013 National Institute for Health and Care Excellence clinical guidelines recommend offering external compression only if interventional treatment is ineffective and as first-line therapy only in pregnant women.15
In some cases, a trial of external compression may be required by insurance companies before approval of interventional treatments. Although the optimal length and pressure for effective treatment has not been determined, typical recommendations include wearing 20 to 30 mm Hg elastic compression stockings with a gradient of decreasing pressure from the distal to proximal extremity.22
Phlebotonics are oral and topical therapies that may increase venous tone, improve capillary hyperpermeability, and decrease blood viscosity with the goal of decreasing symptoms of chronic venous insufficiency.23 They include flavonoids or other compounds often extracted from plants, such as rutin (also called rutoside), diosmin, hidrosmin, disodium flavodate, French maritime pine bark extract (Pycnogenol), grape seed extract, and horse chestnut seed extract (Aesculus hippocastanum). Diosmiplex (Vasculera) is the only prescription formulation available in the United States.23 Diosmiplex is derived from orange rinds and is categorized as a medical food, not a drug. The usual dosage is 630 mg daily.
Horse chestnut seed extract appears to be safe and effective in reducing pain, edema, and pruritus from chronic venous insufficiency when used for two to 16 weeks. The common dosage is 300 mg twice daily or 50 mg of escin, the active compound.24 There is moderate-quality evidence that other phlebotonics may improve edema and possibly decrease symptoms such as cramps, restless legs, and paresthesia.25
Most phlebotonics are available as dietary supplements in the United States, and many formulations contain multiple phlebotonics in a single supplement. Long-term studies of the safety and effectiveness of phlebotonics for the treatment of varicose veins are lacking.25
INTERVENTIONAL TREATMENTS
Thermal Ablation. Thermal ablation destroys damaged veins using an external laser or via endovenous catheter using a laser (endovenous laser ablation) or radio waves (radiofrequency ablation). External laser thermal ablation works best for telangiectasias. In this therapy, hemoglobin absorbs the laser light leading to thermocoagulation.26 Endovenous thermal ablation can be used for larger vessels, including the great saphenous vein. Under ultrasound guidance, a laser optical fiber or radiofrequency catheter electrode is inserted into the vein in a distal to proximal direction. Heat from the laser or radio waves coagulates the blood in the vein, resulting in closure of the vein and redirection of blood flow to functional veins.26,27
Endovenous thermal ablation is performed after a local anesthetic is injected around the vein. Patients can walk after the procedure and may be discharged home the same day. Patients may return quickly to work and other activities. There is a risk (approximately 7%) of surrounding nerve damage attributed to thermal injury; however, most nerve damage is temporary.27 Endovenous thermal ablation is recommended as first-line treatment for nonpregnant patients with symptomatic varicose veins and documented valvular reflux, and need not be delayed for a trial of external compression.7,15
Endovenous Sclerotherapy. Endovenous sclerotherapy involves using ultrasound guidance to inject superficial veins with an agent that causes inflammation of the endothelium, resulting in fibrosis and occlusion in the vein.27 Sclerotherapy is typically used for small (1 to 3 mm) and medium (3 to 5 mm) veins or to treat recurrent varicose veins after surgery; however, there is not a precise diameter used to make treatment decisions.28
A needle is inserted into the vein lumen and the sclerosing agent is injected, often with air to create a foam. The foam displaces the blood and reacts with the vascular endothelium, sealing and scarring the vein. A variety of agents may be used, including hypertonic saline, sodium tetradecyl (Sotradecol), and polidocanol (Varithena). There is no evidence that any of these agents is superior to the others in terms of effectiveness or patient satisfaction.29
Surgery. Historically, surgery with ligation and stripping of the great or small saphenous vein has been the standard of care for the treatment of varicose veins after the failure of conservative therapy. However, a growing body of literature does not consistently support surgery as the best interventional treatment option, and the 2013 National Institute for Health and Care Excellence clinical guidelines recommend surgery as third-line therapy after endovenous thermal ablation and sclerotherapy.15,30,31
Updated surgical techniques use small incisions to reduce scarring, blood loss, and complications and limit removal of the superficial axial veins from the groin to knee. Some of these procedures can be performed under regional or local anesthesia.7 Ligation and stripping of the great and small saphenous vein are probably the best-known procedures. Typically, the vein is divided proximally, a vein stripper is passed distally to an incision made near the knee to access the tip of the stripper. The proximal end of the stripper is secured to the vein and the vein is then removed as the stripper is pulled distally. Nonsaphenous and smaller veins can be removed via phlebectomy, during which a scalpel or large-gauge needle is used to create punctures every 2 to 3 cm along a varicose vein. Segments of the damaged vein are removed using forceps or small hooks.
OUTCOME DATA
A 2014 Cochrane review concluded that endovenous laser ablation, radiofrequency ablation, and foam sclerotherapy are as effective as surgery for great saphenous vein varices.30 Prior literature suggested that traditional surgical treatment of varicose veins with great saphenous vein ligation at the saphenofemoral junction and stripping has a five-year recurrence rate of 20% to 28%.30 Clinical recurrence of varicose veins at five years was measured in only one study in the Cochrane review and suggested no difference between endovenous laser ablation and surgery.30 Maintaining saphenous vein occlusion at six months is less likely with sclerotherapy than with endovenous laser ablation or surgery (43% vs. 80%).31 Endothermal ablation resulted in less recurrence of reflux at one year compared with surgery when treating varicose veins of the small saphenous vein resulting from incompetence of the saphenous-popliteal junction.27
Nonsurgical therapies may have faster return-to-work and recovery times than surgery. Endovenous laser ablation may be better tolerated than sclerotherapy and surgery, with fewer adverse effects and equal effectiveness.30,31 For all three therapies, rates of minor and major complications, including numbness, persistent bruising or tenderness, skin ulceration, skin staining, and lumpiness, are relatively low (1% to 7%).31 Hematomas occur more often with surgical treatment than with foam sclerotherapy or radiofrequency ablation. Endovenous laser ablation appears to be superior to surgery in terms of technical failure and neovascularization. Although all interventional treatment leads to symptomatic improvement, the improvement at six months may be more significant with endovenous laser ablation and surgery than with foam sclerotherapy.31
This article updates a previous article on this topic by Jones and Carek.18
Data Sources: A search was performed in Essential Evidence Plus. Additionally, PubMed and the Cochrane database were searched using the key term varicose veins. The PubMed search was limited to English language, humans, 10 years, and systematic reviews. Search dates: March 15, 2018; June 6, 2018; and February 21, 2019.
