Am Fam Physician. 2019;100(2):82-88
Related letter: Skin Disorders in Patients with Skin of Color
Author disclosure: No relevant financial affiliations.
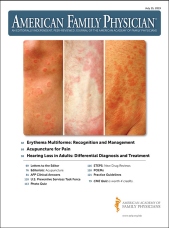
Erythema multiforme is an immune-mediated reaction that involves the skin and sometimes the mucosa. Classically described as target-like, the erythema multiforme lesions can be isolated, recurrent, or persistent. Most commonly, the lesions of erythema multiforme present symmetrically on the extremities (especially on extensor surfaces) and spread centripetally. Infections, especially herpes simplex virus and Mycoplasma pneumoniae, and medications constitute most of the causes of erythema multiforme; immunizations and autoimmune diseases have also been linked to erythema multiforme. Erythema multiforme can be differentiated from urticaria by the duration of individual lesions. Erythema multiforme lesions are typically fixed for a minimum of seven days, whereas individual urticarial lesions often resolve within one day. Erythema multiforme can be confused with the more serious condition, Stevens-Johnson syndrome; however, Stevens-Johnson syndrome usually contains widespread erythematous or purpuric macules with blisters. The management of erythema multiforme involves symptomatic treatment with topical steroids or antihistamines and treating the underlying etiology, if known. Recurrent erythema multiforme associated with the herpes simplex virus should be treated with prophylactic antiviral therapy. Severe mucosal erythema multiforme can require hospitalization for intravenous fluids and repletion of electrolytes.
Erythema multiforme is an acute, typically self-limited skin condition with lesions that can be isolated, recurrent, or persistent.1 Erythema minor affects only the skin and erythema major includes mucocutaneous involvement.1,2 Although it was previously thought that erythema multiforme was on the same pathologic spectrum as Stevens-Johnson syndrome (SJS) and toxic epidermal necrolysis, it is now accepted that erythema multiforme is a distinct disease.3,4
| Clinical recommendation | Evidence rating | Comments |
|---|---|---|
| Suspect erythema multiforme in patients with a target or iris lesion characterized by three concentric segments: a dark center, surrounded by a lighter pink ring, both of which are surrounded by a red ring.1 | C | Expert opinion |
| Symptomatic treatment with topical steroids or antihistamines is recommended for acute episodes of uncomplicated erythema multiforme.1,21 | C | Expert opinion |
| Oral anesthetics may be helpful in decreasing the pain of oral erythema multiforme lesions.1,4,6 | C | Case series, expert opinion |
| Urgent ophthalmologic consultation is recommended for patients with any ocular erythema multiforme involvement.1 | C | Expert opinion |
| Continuous prophylactic antiviral treatment is recommended for recurrent herpes simplex virus–associated erythema multiforme.41 | B | Based on a single, double-blind, placebo-controlled trial |
Etiology
Erythema multiforme is caused by a cell-mediated immune response, and infections are associated with 90% of cases.6 Although herpes simplex virus (HSV) type 1 is the most commonly identified etiology, HSV-2 also has been shown to cause erythema multiforme8 (Figure 1). Mycoplasma pneumoniae is the second most common etiology, especially in children.6,9 Although medications cause less than 10% of erythema multiforme cases, many drugs have been associated with erythema multiforme, most commonly nonsteroidal anti-inflammatory drugs, antiepileptics, and antibiotics.1,4,6 Drug-associated lesions have tested positive for tumor necrosis factor-α (TNF-α), and HSV-associated lesions have tested positive for interferon-γ.10 Types of antibiotics associated with erythema multiforme include sulfonamides, penicillins, erythromycin, nitrofurantoin, and tetracyclines. Other medications include barbiturates, phenothiazines, statins, and TNF-α inhibitors11 (Table 1).

| Infections | Cytomegalovirus | |
| Epstein-Barr virus | ||
| Hepatitis C virus | ||
| Herpes simplex virus type 1, herpes simplex virus type 2 | ||
| Influenza virus | ||
| Mycoplasma pneumoniae | ||
| Vulvovaginal candidiasis | ||
| Drugs | Antibiotics | |
| Erythromycin | ||
| Nitrofurantoin | ||
| Penicillins | ||
| Sulfonamides | ||
| Tetracyclines | ||
| Antiepileptics | ||
| Barbiturates | ||
| Nonsteroidal anti-inflammatory drugs | ||
| Phenothiazines | ||
| Statins | ||
| Sulfonamides | ||
| Tumor necrosis factor-α inhibitors | ||
| Vaccines | ||
| Other conditions | Inflammatory bowel disease | |
| Malignancy | ||
| Menstruation | ||
Vaccines such as measles, mumps, and rubella; smallpox; hepatitis B; meningococcal (Figure 2); pneumococcal; varicella; influenza; and Haemophilus influenzae have also been associated with erythema multiforme, although incidence is low.12–16 Less commonly, erythema multiforme has been associated with autoimmune diseases, such as inflammatory bowel disease17 and malignancies, specifically leukemia and lymphoma.18 Persistent erythema multiforme and refractory erythema multiforme have been found in patients with solid organ cancers, such as renal cell carcinoma and gastric adenocarcinoma.19,20

Clinical Presentation
TYPICAL APPEARANCE
Erythema multiforme lesions typically begin as pink or red papules, which can then become plaques.21,22 These lesions can cause burning or itching.23 Over the next three to five days, the lesions transform into a variety of appearances.1,3,6,24 The classic lesion of erythema multiforme is called the target or iris lesion. It is a round lesion of three concentric segments: a dark center, surrounded by a lighter pink ring, both of which are surrounded by a red ring1,8 (Figure 3). Atypical lesions may only have two zones of color and may have poorly defined borders1,25 (Figure 4). Lesions are initially found symmetrically on the extremities, especially on extensor surfaces. The lesions usually spread centripetally but tend to be fewer on patients' trunks. Palms and soles also may be involved. Erythema multiforme has a predilection for areas of current sunburn or physical trauma.6 Cutaneous lesions usually heal without complication, but skin hyperpigmentation may occur.1 Isolated episodes of erythema multiforme most commonly follow HSV infections by an interval of 10 days and usually resolve within two weeks.22 However, some episodes of erythema multiforme have been documented to persist for up to five weeks.26


Mucosal lesions are present in 25% to 60% of patients with erythema multiforme.6 Prodromal weakness, fever, and malaise are common symptoms in patients with mucosal involvement.1,6 When these associated symptoms are present, they usually occur at least one week before skin lesions occur.4 Although the oral mucosa is the most commonly involved, genital and ocular mucosa also may develop lesions.2 Mucosal lesions usually begin as edematous, erythematous lesions that may develop into shallow erosions with pseudomembranes6 (Figure 5). Mucosal erosions may be extremely painful; therefore, clinicians should assess the patient's ability to maintain oral intake.

RECURRENT AND PERSISTENT ERYTHEMA MULTIFORME
Patients may experience recurrent erythema multiforme with multiple episodes. A study of 48 patients with recurrent erythema multiforme reported an average of six episodes per year.27 The mean disease duration was from six to 10 years.27,28 Recurrent erythema multiforme may occur because of the reactivation of HSV (Figure 6), even if there are no symptoms of an active HSV outbreak.1,8 Although recurrent erythema multiforme has been associated with a variety of medical conditions (e.g., HSV, M. pneumoniae, hepatitis C, menstruation), the study did not find an association with any identified cause in 60% of patients.27 In 2018, a retrospective review of recurrent erythema multiforme found that compared with adults, recurrent erythema multiforme in children shows a male predominance, causes more hospitalizations, and has less of a treatment response to immunosuppression.29

Diagnosis
Erythema multiforme is diagnosed clinically, based on the patient's history and physical examination. It is important to ask about recent symptoms of infection (e.g., HSV, M. pneumoniae) and medication use.1 Most cases of erythema multiforme do not require further diagnostic tests. However, in unclear cases, skin biopsies and laboratory tests may be helpful in excluding other diagnoses.1 The results of skin biopsies vary based on the timeline of the lesion and the location of the biopsy within the lesion.3,22 Direct immunofluorescence can help differentiate between erythema multiforme and autoimmune blistering diseases, such as bullous pemphigoid.1
The differential diagnosis includes many conditions, such as pityriasis rosea, urticaria, viral exanthema, fixed drug eruption, bullous pemphigoid, SJS, polymorphous light eruption, paraneoplastic pemphigus, and hypersensitivity reactions1,3,10,34 (Table 21,8,35–37). Urticaria symptoms resemble erythema multiforme, and these two conditions should be distinguished based on the presentation of the lesions. Erythema multiforme typically has fixed lesions for a minimum of seven days,6 and individual urticarial lesions often resolve within one day.3,21 Fixed drug eruption usually has fewer lesions than erythema multiforme and a medication change is usually present in the patient's history.38 Mucosal lesions associated with SJS may resemble erythema multiforme's mucosal lesions, but can be differentiated by the lesion patterns on the skin.1,25 Although SJS usually contains widespread erythematous or purpuric macules with blisters, erythema multiforme manifests as papular, often target-shaped lesions.39 Patients with SJS should receive urgent medical attention because of the risk of complications.39,40
| Differential diagnosis | Clinical manifestation |
|---|---|
| Bullous pemphigoid | Pruritic, erythematous plaques with tense bullae; with or without mucosal involvement |
| Fixed drug eruption | Few, well-circumscribed erythematous plaques with medication history |
| Hypersensitivity reaction | Morbilliform eruption most commonly found on the upper extremities, trunk, face |
| Paraneoplastic pemphigus | Polymorphous, erythematous mucocutaneous lesions, including papules, bullae, and erosive lesions; presence of underlying malignancy |
| Pityriasis rosea | Scaly, erythematous plaques following herald patch formation on trunk |
| Polymorphous light eruption | Erythematous papules and plaques in areas exposed to sunlight |
| Stevens-Johnson syndrome | Atypical macular target lesions with central dusky erythema, bullae; several mucosal involvements at one or more sites |
| Urticaria | Pruritic, sharply demarcated papules/plaques; transient, usually lasting less than 24 hours |
| Viral exanthema | Diffuse maculopapular rash, palatal petechiae; with or without systemic findings such as lymphadenopathy or splenomegaly |
Treatment
The management of erythema multiforme depends on the underlying etiology and the disease severity1 (Figure 7). Most recommendations are based on small case series or expert opinion, and there have been few clinical trials. When a recent infection or drug is the cause of the erythema multiforme eruption, treat the infection or discontinue the medication. Manage acute, uncomplicated erythema multiforme with symptomatic treatment using topical steroids or antihistamines.1,21 If HSV is the cause, expert opinion recommends early administration of oral acyclovir to reduce the severity and duration of the erythema multiforme eruption.34 However, in cases of established HSV-related erythema multiforme, there is no evidence that antiviral therapy improves the time to lesion resolution.1,6
Mucosal erythema multiforme may be very painful. Based on expert opinion and case series, treatment options include high-potency topical corticosteroid gel and oral antiseptic or anesthetic solutions.1 Severe cases of mucocutaneous erythema multiforme may cause decreased oral intake, which leads to hospitalization for intravenous fluids and repletion of electrolytes.1,4 This is a leading cause of morbidity in those with erythema multiforme.6 Month-long prednisone tapers can be initiated for patients with severe symptoms, but no controlled studies have supported this treatment.1 Patients with ocular involvement should be evaluated by an ophthalmologist immediately because visual sequelae may be permanent.
Recurrent HSV-associated erythema multiforme can be treated with continuous prophylactic antiviral therapy.28,41 Data to support treatment are limited, with a single placebo-controlled trial of 20 patients finding a significant reduction in recurrences with 400 mg of acyclovir administered twice daily over a six-month period (median zero vs. three recurrences over six months, P < .001).41 It has been recommended based on pathophysiologic reasoning that therapy may be continuous or intermittent, but only continuous therapy has been studied.1,41 Options include acyclovir (400 mg twice per day), valacyclovir (Valtrex; 500 mg twice per day), or famciclovir (250 mg twice per day), but there are insufficient studies to determine the recommended duration of treatment.1 For patients who do not respond to antiviral medications, a variety of other treatment options include immunosuppressives, antimalarials, corticosteroids, and others.1 Systemic agents for treatment of refractory recurrent erythema multiforme have been used, but there is little evidence to support these treatments.1 A small study indicated thalidomide as a treatment for reducing the duration of erythema multiforme flare-ups, but further research is encouraged.42
This article updates a previous article on this topic by Lamoreux, et al.3
Data Sources: A PubMed search was completed in Clinical Queries using the term erythema multiforme. The search included meta-analyses, systematic reviews, clinical trials, and reviews. Also searched were Essential Evidence Plus, Cochrane Database of Systematic Reviews, U.S. Preventive Services Task Force, DynaMed, UpToDate, and the American Academy of Family Physicians website. Search dates: March 2018, June 2018, September 2018, December 2018, and March 2019.