
Am Fam Physician. 2020;101(3):147-158
Author disclosure: No relevant financial affiliations.
Healthy development is likely to occur when an adolescent's risk factors are limited and when protective factors are fostered. Healthy development is further encouraged when youth feel valued, empowered, and form healthy social connections. Threats to the well-being of adolescents typically result from experimentation and psychosocial stressors. SSHADESS (strengths, school, home, activities, drugs, emotions/eating, sexuality, safety) is a mnemonic to facilitate collection of psychosocial history of critical life dimensions emphasizing strengths within a youth's life experience instead of solely focusing on risks, which in isolation can provoke feelings of shame. Because adolescents are more likely to access health care and share sensitive information when confidentiality is assured, clinicians should regularly offer confidential screening and counseling. When limited for time, a brief psychosocial screen may include current stressors, availability of a confidant, and school or work experience as a proxy for well-being. Clinicians should provide education to prevent initiation of tobacco use. Long-acting reversible contraceptives are safe and effective in adolescents and should be offered as first-line options to prevent pregnancy. Sexually active females 24 years or younger should be screened for gonorrhea and chlamydia annually. Adolescents 12 years or older should be screened for major depressive disorder when systems are available to ensure accurate diagnosis, treatment, and follow-up. Adolescents with body mass index at the 95th percentile or higher should be referred for comprehensive behavioral interventions. Seatbelt use and avoidance of distracted or impaired driving should be discussed. Clinicians should discuss digital literacy and appropriate online boundary setting and display of personal information.
Adolescence, the life stage between childhood and adulthood, encompasses the physical, cognitive, and emotional changes of puberty resulting in maturity.1 For this reason, we use adolescence to refer to an expanded age range inclusive of what may be traditionally defined as young adulthood (e.g., 10 to 24 years) to reflect the complex biologic growth and social role transitions that occur during this period.1 Through exploration, an adolescent's thinking progresses from concrete to abstract with greater ability to appreciate consequences and independently seek advice with maturity.1,2 Threats to the well-being of adolescents typically result from experimentation and psychosocial stressors.3–5
WHAT'S NEW ON THIS TOPIC
Adolescents are more likely to access health care, have a more favorable attitude about their clinicians, and share sensitive information when confidentiality is assured. However, approximately 60% do not get time alone with their clinician for confidential discussion despite patient and parental preferences.
In the United States, 95% of youth 13 to 17 years of age report smartphone access, and almost 50% report nearly constant use.
Approximately one-half of new sexually transmitted infections occur in people 15 to 24 years of age. Rates of chlamydia, gonorrhea, and syphilis infections among adolescents increased from 2012 to 2016.
Causes of death among people 10 to 24 years of age in the United States include motor vehicle crashes (22%), other unintentional injuries (20%), suicide (17%), and homicide (15%).3 Furthermore, morbidity involving sexuality, substance misuse, social media, eating, and other stressors is widespread (Table 1).4,6,7 In a national survey of high school students' behavior in the previous month, 39% reported texting while driving, and 30% reported using alcohol.4 Despite these risks, most adolescents thrive.8
| Behavior | 2007 (%) | 2017 (%) |
|---|---|---|
| Poor diet or low physical activity | ||
| Obese | 13.0 | 14.8 |
| Overweight | 15.8 | 15.6 |
| Physically active < 60 minutes on any day in previous seven days | 24.9 | 15.4 |
| Used computer for ≥ 3 hours per average school day for work unrelated to school | 24.9 | 43.0 |
| Sexual activity | ||
| Currently sexually active | 35.0 | 28.7 |
| Did not use a condom during most recent sexual intercourse | 38.5 | 46.2 |
| Did not use any method to prevent pregnancy during most recent sexual intercourse | NA | 13.8 |
| Ever had sexual intercourse | 47.8 | 39.5 |
| Has had at least four sex partners | 14.9 | 9.7 |
| Substance misuse | ||
| Alcohol use within 30 days | 44.7 | 29.8 |
| Ever misused prescription opiates | NA | 14.0 |
| Ever used cocaine, inhalants, heroin, methamphetamine, hallucinogens, or ecstasy | 22.6 | 14.0 |
| Marijuana use within 30 days | 19.7 | 19.8 |
| Smoked ≥ 1 cigarette within 30 days | 20.0 | 8.8 |
| Used electronic vapor product within 30 days | NA | 13.2 |
| Suicide* | ||
| Attempted suicide | 6.9 | 7.4 |
| Experienced persistent feelings of sadness or hopelessness | 28.5 | 31.5 |
| Required treatment after a suicide attempt | 2.0 | 2.4 |
| Seriously considered attempting suicide | 14.5 | 17.2 |
| Unintentional injury | ||
| Carried a gun unrelated to hunting or sport during previous 12 months | NA | 4.8 |
| Carried a weapon in previous 30 days | 18.0 | 15.7 |
| Drove a car after drinking alcohol in previous 30 days (among drivers) | 10.5 | 5.5 |
| Never or rarely wears a seatbelt | 11.1 | 5.9 |
| Ridden in car in past 30 days with a driver who was drinking alcohol | 29.1 | 16.5 |
| Texted or emailed while driving | NA | 39.2 |
| Violence victimization | ||
| Bullied at school | NA | 19.0 |
| Did not go to school because of safety concern | 5.5 | 6.7 |
| Electronically bullied | NA | 14.9 |
| Experienced physical dating violence | 9.9 | 8.0 |
| Experienced sexual dating violence | NA | 6.9 |
| Forced to have sex | 7.8 | 7.4 |
| Threatened/injured with a weapon at school | 7.8 | 6.0 |
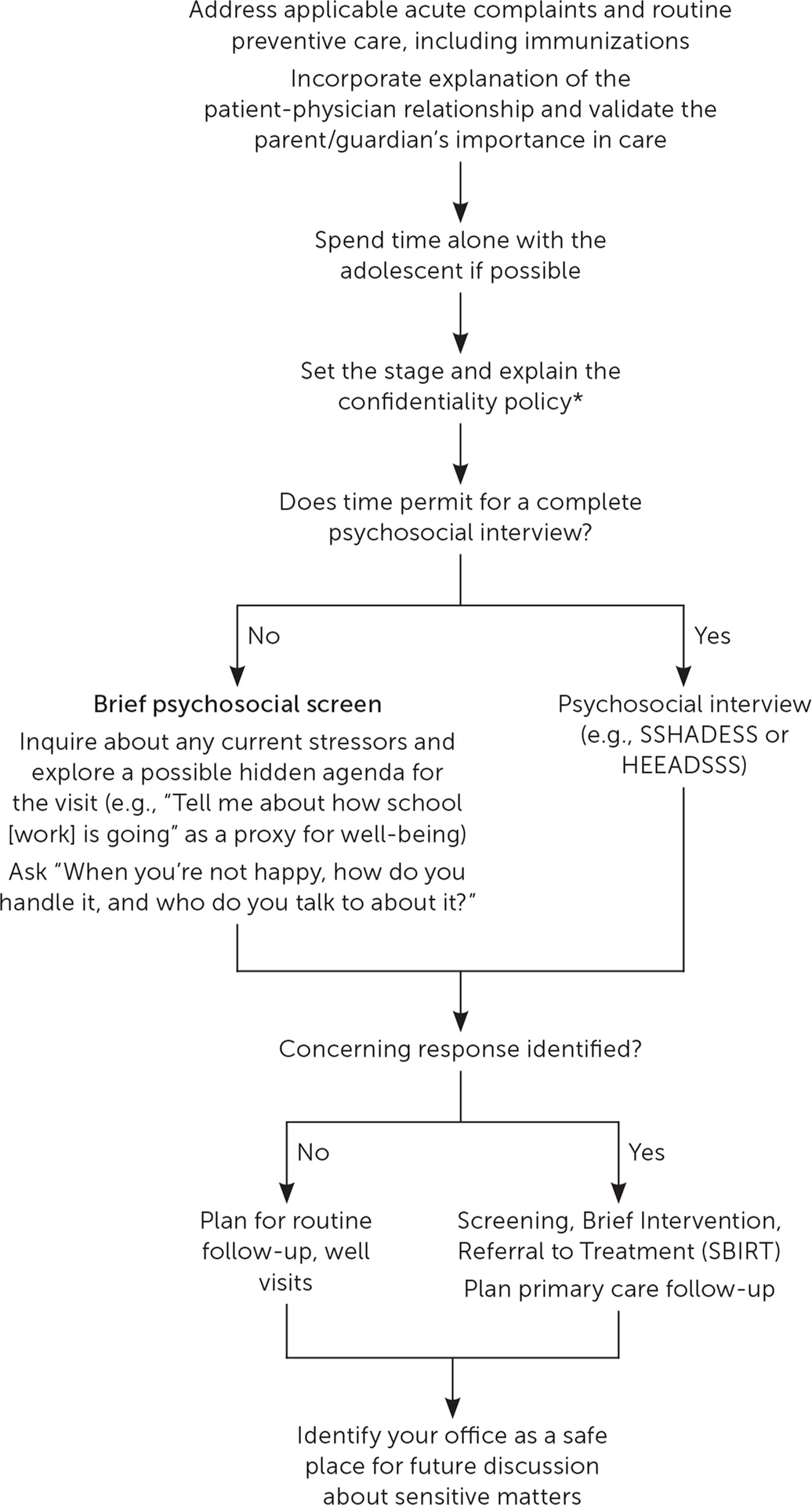
Adolescents typically present to care for acute complaints. Only 70% of school-aged youth have a preventive care visit within four years, and some adolescents are exposed to health care only during sports preparticipation examinations.9 Knowing that adolescents seek health-related information from online and unverified sources,10 clinicians have a unique opportunity to provide accurate information and administer preventive care at all visits through trusted clinician-patient relationships8,10,11 (Table 22,11; Figure 15,8,12).
| Screening/counseling | Recommendation | Grade; year |
|---|---|---|
| Cancer | ||
| Cervical | Screen every three years with cervical cytology alone in women 21 to 29 years of age | Grade A; 2018 |
| Screening women < 21 years is not recommended | Grade D; 2018 | |
| Skin: behavioral | Counsel young adults and adolescents with fair skin types about minimizing exposure to ultraviolet radiation | Grade B; 2018 |
| Testicular | Screening is not recommended | Grade D; 2011 |
| Cardiovascular health | ||
| Blood pressure (hypertension) | Insufficient evidence to assess the balance of benefits and harms of screening asymptomatic adolescents to prevent cardiovascular disease in childhood or adulthood | Grade I; 2013 |
| Screen those ≥ 18 years; obtain measurements outside of the clinic setting for diagnostic confirmation before starting treatment | Grade A; 2015 | |
| Lipid disorders | Insufficient evidence to assess the balance of benefits and harms of screening ≤ 20 years | Grade I; 2016 |
| General health | ||
| Intimate partner violence | Screen women of reproductive age and provide or refer women who screen positive to ongoing support services | Grade B; 2018 |
| Obesity | Screen and offer or refer to comprehensive, intensive behavioral interventions | Grade B; 2017 |
| Prevention of neural tube defects | Recommend that all women who are planning or capable of pregnancy take a daily supplement containing 0.4 to 0.8 mg of folic acid | Grade A; 2017 |
| Scoliosis | Insufficient evidence to assess the balance of benefits and harms of screening in children and adolescents 10 to 18 years of age* | Grade I; 2018 |
| Mental health | ||
| Depression | Insufficient evidence to assess the balance of benefits and harms of screening in children ≤ 11 years | Grade I; 2016 |
| Screen adolescents 12 to 18 years of age and adults, including pregnant and postpartum women; adequate diagnostics, effective treatment, and follow-up should be in place | Grade B; 2016 | |
| Suicide risk | Insufficient evidence to assess the balance of benefits and harms of screening adolescents in primary care | Grade I; 2014 |
| Sexually transmitted infections | ||
| Behavioral | Provide intensive behavioral counseling for all sexually active adolescents | Grade B; 2014 |
| Chlamydia and gonorrhea | Screen sexually active women ≤ 24 years | Grade B; 2014 |
| Insufficient evidence to assess the balance of benefits and harms of screening in males | Grade I; 2014 | |
| Hepatitis B virus infection | Screen those at high risk of infection (e.g., > 2% hepatitis B virus prevalence in country of origin, HIV infection, injection drug users, household contacts or sex partners of others with hepatitis B virus infection, men who have sex with men, immunocompromised persons, or those in other high-prevalence settings) | Grade B; 2014 |
| Screen for hepatitis B virus in pregnant women at their first prenatal visit | Grade A; 2019 | |
| Herpes simplex virus infection | Routine serologic screening in asymptomatic adolescents is not recommended, including in women who are pregnant | Grade D; 2016 |
| HIV infection | Screen adolescents ≥ 15 years; screen younger adolescents with risk factors†; offer preexposure prophylaxis with effective antiretroviral therapy to those at high risk of HIV acquisition | Grade A; 2019 |
| Screen pregnant women | Grade A; 2019 | |
| Syphilis | Screen adolescents who are at increased risk of infection‡ | Grade A; 2016 |
| Screen pregnant women | Grade A; 2018 | |
| Substance abuse | ||
| Alcohol | Evidence is insufficient to assess the balance of benefits and harms of screening and brief behavioral counseling interventions for adolescents 12 to 17 years of age | Grade I; 2018 |
| Screen for unhealthy alcohol use in those ≥ 18 years, including pregnant women, and provide those engaged in risky or hazardous drinking with brief behavioral counseling interventions to reduce unhealthy alcohol use | Grade B; 2018 | |
| Tobacco | Provide interventions, including education or brief counseling, to prevent initiation of tobacco use among adolescents | Grade B; 2013 |
| Ask all individuals ≥ 18 years about tobacco use, advise to stop, and provide behavioral interventions for cessation; if nonpregnant, also offer U.S. Food and Drug Administration–approved pharmacotherapy for cessation | Grade A; 2015 | |
| Evidence is insufficient to assess the balance of benefits and harms of pharmacotherapy intervention for tobacco cessation in pregnant women. | Grade I; 2015 | |
| Evidence is insufficient to recommend electronic nicotine delivery systems for tobacco cessation in adults, including pregnant women. | Grade I; 2015 | |
Approach to Visits
CONFIDENTIALITY
Clinicians should regularly offer confidential screening and counseling because when confidentiality is assured, adolescents are more likely to access health care, have a more favorable attitude about their clinicians, and share sensitive information.13–15 However, approximately 60% do not get time alone with their clinician for confidential discussion despite patient and parental preferences.13,14,16 Clinicians may request privacy by asking, “As part of my routine practice, may I take a moment to speak privately with your daughter about possible stressors [or] to help her begin to take responsibility for her health care?”5 and clarify the approach to confidentiality.5,8,17
Once alone, clinicians can set the stage for a trustworthy relationship by reiterating the purpose of privacy (e.g., to ensure success by discussing positive aspects of life and psychosocial stressors without judgment)8 and limitations to privacy according to applicable minor consent laws (eTable A). Clinicians may consider stating, “Everything we talk about is private (e.g., protected by law) unless I'm particularly worried about your safety, meaning you ending your life or someone else's life or that someone is abusing you. If involvement of others is important, I will tell you, and together we will discuss the way to proceed.”5,8
| Topic | Description | Website |
|---|---|---|
| Contraception | Resource for contraceptive methods, including where to receive emergency contraception | www.bedsider.org |
| Family planning clinics | List of federally funded family planning clinics | www.hhs.gov/opa/title-x-family-planning/initiatives-and-resources/title-x-grantees-list |
| Information privacy and protection | Guidance on pediatric health care information privacy and protection | www.aap.org/en-us/advocacy-and-policy/aap-health-initiatives/healthy-foster-care-america/Documents/Confidentiality_Laws.pdf |
| Mental health services | Journal article reviewing state laws about what parents can do regarding decision-making for adolescent mental health treatment | https://www.tandfonline.com/doi/abs/10.1080/1067828X.2013.777380?journalCode=wcas20 |
| Sexual and reproductive health services | Adolescent health care, including descriptions of confidential services | www.cdc.gov/teenpregnancy/health-care-providers/teen-friendly-health-visit.htm |
| Fact sheets with sexual and reproductive health policy by state | www.guttmacher.org | |
| Sexual assault | Resource for information about sexual assault, including safety and prevention tips, consultation and training, and help line number | https://www.rainn.org/about-sexual-assault |
| Sexually transmitted infections testing and treatment | Free online search tool for where to get tested for HIV or other sexually transmitted infections | https://gettested.cdc.gov/ |
| State-specific minor consent laws (comprehensive; for purchase) | Comprehensive guide to states' minor consent laws | www.cahl.org |
| Statutory rape reporting | Review of reporting requirements for clinicians based on state law | https://aspe.hhs.gov/system/files/pdf/75531/report.pdf |
| Substance abuse services | Journal article reviewing state laws about what parents can do about decision-making for adolescent substance abuse | https://www.tandfonline.com/doi/abs/10.1080/1067828X.2013.777380?journalCode=wcas20 |
Mentioning commonly discussed protected topics such as mental health, drug use, or sexual activity may ease the patient's fear about disclosing sensitive information.8,13–15 Clinicians should strive to prevent confidentiality lapses with electronic health record use (printable prescription and problem lists, automated appointment reminders, test results mailed or visible on patient portals), local pharmacy practices, and billing information.5,18,19
The American Academy of Family Physicians supports clinicians in helping adolescents, young adults, and their parents be aware of the importance of confidential care.20
STRENGTH-BASED INTERVIEWING
Healthy development is likely to occur when an adolescent's risk factors are limited and when protective factors are fostered. Healthy development is further encouraged when adolescents feel valued and empowered and when they form healthy social connections within their schools, peer groups, families, and communities.8,21,22 Clinicians may use motivational interviewing and shared decision-making to help adolescents build confidence for behavioral change.8
SSHADESS (strengths, school, home, activities, drugs, emotions/eating, sexuality, safety) is a mnemonic to facilitate collection of a psychosocial history of critical life dimensions (Table 3).8 Based on the traditional HEEADSSS (home, education/employment, eating, activities, drugs, sexuality, suicide/depression, safety) model,5 this approach emphasizes identifying strengths within a youth's life experience while assessing risks, which in isolation can provoke feelings of shame. 8 Prior examples of a patient overcoming adversity or showing resilience can be incorporated into discussion using praise and reflective interviewing.5,8 SSHADESS also prioritizes initial queries about school functioning—which may be expected and less personal than other topics—and broad screening for emotions and stress rather than limited focus on depression.5,8 The patient's history should be tailored to each patient's personal context (including any adverse childhood or marginalization experiences that may be disclosed as trust is built) instead of a rigid checklist approach.5,8 See Table 4 for questions regarding social media use to be used in conjunction with the SSHADESS mnemonic.5
| Aspect of life | Example questions† |
|---|---|
| Strengths | What do you like doing? |
| How would you describe yourself? | |
| Tell me what you're most proud of? | |
| How would your best friends describe you? | |
| School | What do you enjoy most/least about school? |
| What would you like to do when you get older? | |
| How are your grades? Do you feel like you're doing your best at school? (If no) Why not? | |
| What is getting in the way? | |
| Do you feel safe on the way to school and in school? | |
| Home | Who do you live with? |
| How do you get along with the people you live with? | |
| Could you talk to anyone in your family if you were stressed? | |
| Activities | Do you have a best friend or adult you can trust outside of your family? |
| Are you still involved in the activities you were doing last year? | |
| Are you spending as much time with your friends as you used to? | |
| Drugs/substance misuse | Do any of your friends talk about smoking cigarettes, taking drugs, or drinking alcohol? |
| Do you smoke cigarettes? Drink alcohol? Have you tried sniffing glue, smoking weed, using pills, or other drugs? | |
| When/if you smoke, drink, or get high, how does it make you feel or what does it do for you? | |
| Emotions | Have you been feeling stressed? |
| Do people get on your nerves more than they used to? | |
| Have you been having trouble sleeping lately? | |
| Have you been feeling down, sad, or depressed? Have you thought of hurting yourself or someone else? | |
| Have you ever tried to hurt yourself? | |
| Eating | Would you describe yourself as a healthy eater? |
| Have you been trying to gain or lose weight? Tell me why. | |
| Sexuality | Are you attracted to anyone? Tell me about that person. (Use gender-neutral language.) |
| Are you attracted to guys, girls, or both? Are you comfortable with your sexual feelings? | |
| What kind of things have you done sexually? Kissing? Touching? Oral sex? Have you ever had sexual intercourse? | |
| What steps do you take to protect yourself? | |
| Have you ever worried that you could be pregnant? | |
| Have you ever been worried about or had a sexually transmitted infection? | |
| Safety | Are there a lot of fights at your school? |
| Do you carry weapons? | |
| Do you feel safe at school? Have you been bullied? | |
| Has anyone ever touched you physically or sexually when you didn't want them to? (Note that abuse is asked about in the context of safety, not sexuality.) |
| How many hours do you spend on any given day in front of a screen, such as a computer, television, or phone? Do you wish you spent less time on these things? |
| Some of my patients spend most of their free time online. What types of things do you use the internet for? |
| Have you messaged photos or texts that you have later regretted? |
| Can you think of a friend who was harmed by spending time online? |
| How often do you view pornography (or nude images or videos) online? |
| Have you ever sent unclothed pictures of yourself to anyone online? |
| When was the last time you sent a text message while driving? |
A therapeutic alliance through rapport and continuity of care may reinforce clinicians' recommendations and improve outcomes.8,23 Clinicians may request permission before inquiring about sensitive topics and should limit yes-or-no questions, which can hinder response depth and appear disingenuous.5 Questions should generally progress from impersonal to personal (e.g., “Are any of your classmates experimenting with cigarettes?” before “Have you experimented with cigarettes?”).5,8 Clinicians should thank patients for disclosing personal information, share their concerns respectfully and empathetically (e.g., “I'm worried that your daily marijuana use may affect your goal of military service.”), and reflect patients' previously disclosed examples of resilience. 5 Diminishing statements such as “I understand” or “It's not that big of a deal” should be avoided.5,8
When limited for time, clinicians may prioritize a therapeutic history over thoroughness. In such circumstances, a brief psychosocial screen may include current stressors, availability of a confidant when needed, and school or work experience as a proxy for well-being.8 Previsit computer or written questionnaire-administered comprehensive screening may increase efficiency, but evidence on patient-oriented outcomes, including clinicians' actions based on acquired information, is lacking.24 Privacy may be warranted at every visit because adolescents may present with a hidden agenda. For example, one study showed approximately 50% of youth who completed suicide visited a primary care setting in the preceding month.25
Recommendations
SOCIAL MEDIA
In the United States, 95% of youth 13 to 17 years of age report smartphone access, and almost 50% report nearly constant use or more frequent use than several times per day.26 Traditional and social media, interactive video games, and other digital content can improve adolescents' social support and access to diverse information but may negatively affect health (e.g., sleep, attention, learning, mood, weight, driving safety), compromise personal privacy, and reveal inaccurate content and unsafe contacts.5,27–29
Clinicians should ask about media exposure and educate families about digital literacy, open family communication, and boundary setting on content and display of personal information. Recommendations for a family media use plan (www.healthychildren.org/MediaUsePlan), lifestyle modifications, or behavioral health consultation may help limit risk (Table 5).5,27,28,30
| Questions | Recommendations |
|---|---|
| Which social media sites and/or apps do you use? | Discuss privacy settings |
| Develop a family media use plan | |
| www.healthychildren.org/MediaUsePlan | |
| Discuss digital literacy, critical thinking, and boundary setting | |
| Exposure to inaccurate content | |
| Exposure to unsafe contacts | |
| Display of personal information | |
| Discuss open family communication about media | |
| How long do you spend on social media in a typical day? | Limit nonscholastic screen time to 1 or 1.5 hours daily |
| Participate in at least 1 hour of physical activity daily | |
| Achieve 8 to 12 hours of sleep nightly; remove electronics | |
| Do you think you use social media too much? | Ask what was tried to remedy the overuse |
| Ask what barriers are present; what has been successful | |
| Does viewing social media cause you stress? | Assess mental health risk |
| Recommend a follow-up visit | |
| Refer to a behavioral health professional | |
| Do you use electronic media before bed? | Avoid electronic devices in the bedroom |
| Avoid screen exposure for 1 hour before bedtime | |
| Have you experienced cyberbullying, sexting, or an online user asking to have sex with you? | Facilitate communication between adolescent and caregiver about online citizenship and safety |
| Treat others with respect online | |
| Avoid cyberbullying and sexting | |
| Be wary of online solicitation | |
| Avoid communications that compromise personal safety and privacy |
SUBSTANCE USE
The American Academy of Pediatrics recommends that clinicians screen adolescents for substance use and, if applicable, provide a brief intervention, establish follow-up, and consider referral (e.g., for weekly or more frequent use).12,31 The CRAFFT+N (car, relax, alone, forget, family/friends, trouble, nicotine) screening tool is sensitive for identifying problematic substance use (https://crafft.org/).32
Approximately 87% of adult tobacco users initiate use before age 18; such use can have lifelong deleterious health consequences.33 Among 12th graders in the United States in 2018, 29% reported using a nicotine product, and 21% reported using electronic cigarettes.34 Electronic cigarette users are more likely than nonusers to use combustible cigarettes, and users of nicotine or tobacco products are more likely than nonusers to use marijuana.35,36 Nicotine products may disproportionately affect neural pathways involving attention, cognition, addiction, and mood if used in adolescence.37 Clinicians should counsel adolescents to prevent initiation of, or stop, nicotine or tobacco use.11,37 Limited evidence suggests that behavioral support or smoking cessation medications facilitate long-term cessation in youth.38
Adolescents who experiment with alcohol, marijuana, energy drinks, supplements, unauthorized prescription opioids, or other substances may develop problematic use. Although evidence for adolescents is limited, brief behavioral counseling to reduce alcohol use has demonstrated benefit in adults.39 Marijuana use by adolescents has been associated with abnormal neural development and may increase the risk of depression and suicidality in adulthood40; clinicians should consider local state laws and patient age when counseling individuals on its use.31 Use of prescribed opioids before high school graduation is associated with a 33% increased risk of subsequent opioid misuse.41 Buprenorphine is approved to treat opioid-addicted adolescents 16 years and older.42 Energy drinks contain unregulated ingredients and stimulants, have no therapeutic benefit, and may cause toxicity; screening for use provides opportunities for education.43 A previous article in American Family Physician provides further information about recognition and management of adolescent substance misuse.44
SEXUAL HEALTH
Adolescent pregnancy, a risk factor for adverse fetal and maternal outcomes,45 has become less common in recent years.46 According to a survey among adolescents 15 to 19 years of age, this trend was attributed to improvements in contraceptive use as opposed to changes in rates of sexual behaviors.46 Clinicians should counsel adolescents on pregnancy risk, healthy relationships, and contraception, including long-acting reversible contraception as a first-line option and availability of emergency contraception.5,47,48 Reducing barriers to contraceptives for adolescents reduces health disparities and abortion rates without increasing rates of sexual activity.49–51 Discussions about menstruation and bleeding patterns should be conducted regularly and may serve as a proxy for overall health status.52
Approximately one-half of new sexually transmitted infections occur in adolescents 15 to 24 years of age.53 Rates of reported chlamydia, gonorrhea, and syphilis infections among adolescents have increased from 2012 to 2016.53 As part of the confidential sexual history, clinicians should assess sexual behaviors, including number of partners, barrier contraceptive use, and a history of sexually transmitted infections (Table 6).2,5,54 Abstinence, if practiced, should be reinforced.54 Clinicians should annually screen for gonorrhea and chlamydia in sexually active females 24 years or younger.11,54 Adolescents who are at high risk for these infections may benefit from testing every three to six months.54 Age- and risk-specific immunizations should be provided.
| Action | Example |
|---|---|
| Setting the stage | |
| Address confidentiality* | “Everything we talk about is private [by law], unless I'm particularly worried about your safety, meaning you ending your life or someone else's life or that someone is abusing you. If involvement of others is important, I will tell you, and we can together discuss the way to proceed. Do you have any questions about what is and isn't confidential?” |
| Seek permission to proceed | “I talk to my patients alone for a few moments to discuss aspects of life going well and not well. My goal is to establish trust; I commit to being honest and will avoid judgment during our conversation. May I ask you some personal questions that will help me understand what kind of health advice I can offer you?” |
| Sexuality-specific items | |
| Use gender-neutral language when appropriate | “Have you had a romantic or sexual relationship with someone?” |
| “Tell me more about your relationship(s).” | |
| Clarify unfamiliar terminology | “Can you clarify what you mean by pansexual identification?” |
| Ask direct, respectful questions for clarification if indicated | “What are your plans for birth control?” |
| “Are you participating in sex education classes?” | |
| “Have you been sexually involved with anyone in the past six months?”† | |
| “Are your sexual activities enjoyable?” | |
| “Have you and your partner talked about consent—and the importance of obtaining consent from each other before having sexual contact?” | |
| “What are your concerns or questions about sex?” | |
| “What have you learned about HIV and sexually transmitted infections?” | |
| “What types of sexual experiences have you had?” (instead of “Are you sexually active?”) | |
| “Have any of your relationships been violent?” | |
| “Have you ever been pregnant or worried that you may be pregnant?” | |
| “Have you ever had or worried that you had a sexually transmitted infection?” | |
| Use open-ended questions | “How (often) do you use condoms? If you don't use them, what gets in the way?” |
| “What does the term safer sex mean to you?” | |
| Describe how clinicians can help | “I'm here to educate you and give you information. I hope you'll make good decisions but realize that not every decision will be perfect. If you ever make a mistake, my goal is that you will trust me to help take care of you.” |
| Set goals | “Can we schedule an appointment to discuss birth control before you become sexually active?” |
| “I'm amazed at how you navigated the bullying situation at school. Are you able to use a similar approach in asking new partners to get tested for sexually transmitted infections?” | |
| Use supportive statements when possible | “That must have been hard for you.” |
| “Thank you for sharing your experience with me.” | |
| “You have made the decision to wait to have sex. It sounds like you are making the decision that is right for you.” | |
Many adolescents face issues with sexual orientation and gender identity formation.54 Family connectedness and social support have been shown to be protective against negative mental health outcomes and high-risk sexual behaviors in sexual minority and gender minority populations.54 Clinicians may help adolescents disclose to family members if requested.54
OBESITY AND EATING DISORDERS
More than 30% of adolescents in the United States are overweight or obese.4,55 The U.S. Preventive Services Task Force recommends screening for obesity in adolescents using body mass index percentile and offering or referring to comprehensive, intensive behavioral interventions, including exercise, nutrition, and behavioral modification.11,56,57 Surveillance of the body mass index percentile trend may help identify obesity and disordered eating.56
For obesity prevention, clinicians may recommend 60 minutes of moderate to vigorous physical activity daily and optimization of sleep habits; however, exercise interventions alone may not improve body mass index or health outcomes.30,56 Clinicians may discuss healthy eating patterns, including increased intake of fruits and vegetables, plant-based fats and proteins, legumes, whole grains, and nuts, and avoidance of sweet beverages and processed foods.58
Eating disorders have high lifetime mortality because of disease complications and risk of suicide. If an eating disorder is diagnosed, clinicians should recommend evidence-based treatments (e.g., family-based therapy) and arrange for multidisciplinary care, including a therapist and dietitian.59 Weight restoration is an initial goal and may require inpatient admission59 (eTable B).
| Acute food refusal |
| Acute medical complications of malnutrition (e.g., syncope, seizure, heart failure, pancreatitis) |
| Arrested growth and development |
| Behavioral health or medical conditions that limit outpatient management (e.g., severe depression, obsessive compulsive disorder, type 1 diabetes mellitus) |
| Dehydration |
| Electrocardiogram abnormalities (e.g., prolonged QTc interval) |
| Electrolyte disturbances (e.g., hypokalemia, hyponatremia, hypophosphatemia) |
| Failure of outpatient treatment |
| Median body mass index ≤ 75% for age and sex |
| Physiologic instability including autonomic dysfunction |
| Bradycardia (< 50 beats per minute during the day; < 45 beats per minute at night) |
| Hypotension (< 90/45 mm Hg) |
| Hypothermia (< 96°F [35.5°C]) |
| Orthostatic increase in pulse (> 20 beats per minute) or decrease in blood pressure (> 20 mm Hg systolic or > 10 mm Hg diastolic) |
| Uncontrollable bingeing and purging |
MENTAL HEALTH
The U.S. Preventive Services Task Force recommends that clinicians screen adolescents starting at age 12 and adults for major depressive disorder when systems are in place to ensure accurate diagnosis, treatment, and follow-up.11,60,61 The Patient Health Questionnaire has been validated in adolescents (Table 762–65). Clinicians should interview individuals privately about depressive symptoms and formulate individualized plans if depression, self-harm, or suicidality is identified.63 Self-injury among adolescents may be related to poor coping skills and difficulty managing emotions; the risk of subsequent suicide is substantially higher among those who use violent methods (e.g., a firearm) than with nonviolent methods.66
| Over the past 2 weeks, how often have you been bothered by the following problems? | Not at all | Several days | More than one-half of the days | Nearly every day |
|---|---|---|---|---|
| PHQ-2 (first two questions) | ||||
| 1. Little interest or pleasure in doing things | 0 | 1 | 2 | 3 |
| 2. Feeling down, depressed, irritable, or hopeless | 0 | 1 | 2 | 3 |
| PHQ-9 (all questions, including the first two) | ||||
| 3. Trouble falling or staying asleep or sleeping too much | 0 | 1 | 2 | 3 |
| 4. Feeling tired or having little energy | 0 | 1 | 2 | 3 |
| 5. Poor appetite, weight loss, or overeating | 0 | 1 | 2 | 3 |
| 6. Feeling bad about yourself, that you are a failure, or that you have let yourself or your family down | 0 | 1 | 2 | 3 |
| 7. Trouble concentrating on things such as schoolwork, reading, or watching television | 0 | 1 | 2 | 3 |
| 8. Moving or speaking so slowly that others could have noticed or, the opposite, being so fidgety or restless that you have been moving around a lot more than usual | 0 | 1 | 2 | 3 |
| 9. Thoughts that you would be better off dead or of hurting yourself in some way | 0 | 1 | 2 | 3 |
| Total: | _____+ | _____+ | _____ |
Adolescents diagnosed with mild depressive symptoms may be supported and monitored for approximately eight weeks before treatment; those with moderate to severe symptoms should be offered treatment or referral for treatment.63,67 Combining a selective serotonin reuptake inhibitor and psychotherapy is likely more effective and safer than a single modality.67,68 One-half to two-thirds of adolescents respond positively to selective serotonin reuptake inhibitors and typically better than placebo; suicidality risk has been estimated to be 4% among those medicated vs. 2% using placebo.68 When prescribing psychotropics, clinicians should establish a safety plan and short-interval follow-up, review the U.S. Food and Drug Administration's boxed warning for suicidal thinking and behavior, slowly titrate up from low initial doses, consider psychiatry referral if comorbid conditions exist, and remind caregivers to restrict access to lethal means (e.g., medication stores, weapons).63,67 See a recent article in American Family Physician for more information about depression in adolescents.69
SAFETY
In the United States, motor vehicle crashes are the number one cause of mortality among adolescents and may be attributed to driving inexperience, distraction, and risky behavior.3,70 The American Academy of Pediatrics recommends that clinicians encourage seatbelt use, adherence to graduated driver's licensing laws (e.g., nighttime, passenger restrictions), and avoidance of distracted or impaired driving.70
Approximately 1.5 million sports- and recreation-related concussions occur yearly among adolescents 18 years and younger in the United States.71 Individualized management should include immediate removal from play with a brief period of physical and cognitive rest followed by step-wise return to sport or play.72
Clinicians should inquire about patients' risk of violence (e.g., history of abuse, gang involvement, low school commitment, fear of assault, use of weapons). Interventions may focus on connecting adolescents with positive adult role models, community programs, and mental health services to develop coping skills and healthy relationships.2,73 Firearms should be stored unloaded, locked, and separate from ammunition.74
Data Sources: A PubMed search was completed using the MeSH function with the key phrase adolescent used in a number of specialized queries with the terms confidentiality, psychosocial history, depression, social media, or other key terms related to psychosocial history taking and the specific conditions highlighted in this article. We identified the latest guidelines on the aforementioned topics from the American Academy of Pediatrics, the Centers for Disease Control and Prevention, and the U.S. Preventive Services Task Force; the reference lists of these guidelines were searched for additional articles. Other queries included Essential Evidence Plus and the Cochrane Database of Systematic Reviews. Search dates: December 1, 2018, through March 1, 2019; September 2, 2019.
The views expressed in this publication are those of the authors and do not reflect the official policy or position of the Uniformed Services University of the Health Sciences; the Departments of the Army, Navy, or Air Force; the Department of Defense; or the U.S. government.
