Am Fam Physician. 2020;101(8):472-480
Patient information: See related handout on chronic diarrhea, written by the authors of this article.
Author disclosure: No relevant financial affiliations.
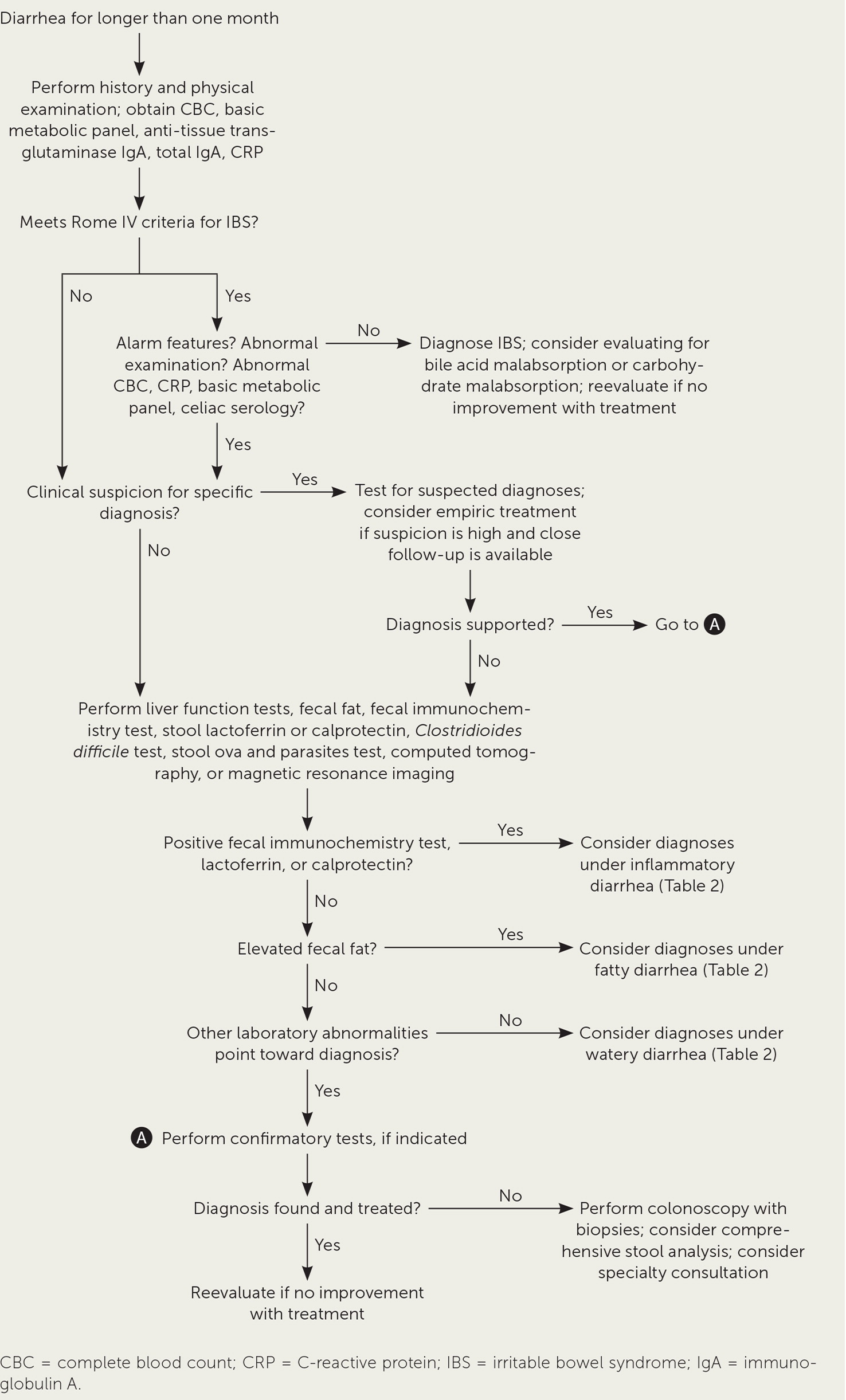
Chronic diarrhea is defined as a predominantly loose stool lasting longer than four weeks. A patient history and physical examination with a complete blood count, C-reactive protein, anti-tissue transglutaminase immunoglobulin A (IgA), total IgA, and a basic metabolic panel are useful to evaluate for pathologies such as celiac disease or inflammatory bowel disease. More targeted testing should be based on the differential diagnosis. When the differential diagnosis is broad, stool studies should be used to categorize diarrhea as watery, fatty, or inflammatory. Some disorders can cause more than one type of diarrhea. Watery diarrhea includes secretory, osmotic, and functional types. Functional disorders such as irritable bowel syndrome and functional diarrhea are common causes of chronic diarrhea. Secretory diarrhea can be caused by bile acid malabsorption, microscopic colitis, endocrine disorders, and some postsurgical states. Osmotic diarrhea can present with carbohydrate malabsorption syndromes and laxative abuse. Fatty diarrhea can be caused by malabsorption or maldigestion and includes disorders such as celiac disease, giardiasis, and pancreatic exocrine insufficiency. Inflammatory diarrhea warrants further evaluation and can be caused by disorders such as inflammatory bowel disease, Clostridioides difficile, colitis, and colorectal cancer.
Chronic diarrhea is defined as a predominantly decreased stool consistency lasting longer than four weeks.1,2 The prevalence is estimated to be 1% to 5% of the adult population.1 Common causes include irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), celiac disease, and microscopic colitis. The differential diagnosis for chronic diarrhea is broad; however, a thorough history and physical examination can narrow the diagnostic evaluation. The British Society of Gastroenterology published guidelines for the evaluation of chronic diarrhea, and other authors suggest similar diagnostic approaches, but supporting evidence is weak.1,2 The recommendations in this article are based on the evidence available and published guidelines for the evaluation of causes of chronic diarrhea. Figure 1 is an algorithm for the diagnosis of chronic diarrhea.1–4
| Clinical recommendation | Evidence rating | Comments |
|---|---|---|
| A normal C-reactive protein or fecal calprotectin level effectively rules out inflammatory bowel disease for patients who meet Rome IV diagnostic criteria for irritable bowel syndrome without alarm features.1,3,13,30 | A | Good-quality meta-analysis and clinical guidelines |
| Serologic testing should be performed for celiac disease in all patients presenting with chronic diarrhea.1,3,8 | C | Evidence-based guidelines, consistent retrospective evidence |
| Clinicians testing for Clostridioides difficile infection should examine only diarrheal stools.21 | C | Evidence-based guidelines, consistent observational evidence |
History
Most patients use the word diarrhea to describe loose stools3; however, some patients may use it to describe fecal urgency, frequency, or incontinence.2 The Bristol Stool Scale (https://www.aafp.org/afp/2011/0801/p299.html#afp20110801p299-f1) is helpful in distinguishing diarrhea from pseudodiarrhea.5 This article covers diarrhea as it is commonly defined in the medical literature (i.e., Bristol types 5 to 7).2,3
Clinicians should ask patients about key historical features, including stool appearance and odor, the presence of urgency or tenesmus, pain, the frequency and duration of symptoms, whether diarrhea persists at night or with fasting, and possible triggers.2,4 A thorough travel and dietary history can help guide the clinician toward an appropriate workup for infections or food intolerance. A review of systems can reveal extraintestinal manifestations of the disease. A complete medication history, including over-the-counter medications, illicit drug use, alcohol use, and supplements, is indicated. Table 1 lists medications commonly associated with diarrhea6; however, a patient can experience diarrhea from almost any medication.1,4 A discussion of current medical diagnoses and any prior surgical procedures may identify an etiology. A behavioral health history should be obtained, including the psychosocial impact of symptoms on the patient and potential secondary gain. Documentation from any previous office visits, laboratory testing, and diagnostic procedures should be obtained before further testing.4 Table 2 lists clues to specific diagnoses.1–4,6–21 Diagnoses affecting immunocompromised patients with chronic diarrhea are beyond the scope of this article.
| Osmotic Citrates, phosphates, sulfates Magnesium-containing antacids and laxatives Sugar alcohols (e.g., mannitol, sorbitol, xylitol) Secretory Antiarrhythmics (e.g., quinine) Antibiotics (e.g., amoxicillin/clavulanate [Augmentin]) Antineoplastics Biguanides Calcitonin Cardiac glycosides (e.g., digitalis) Colchicine Nonsteroidal anti-inflammatory drugs (may contribute to microscopic colitis) Prostaglandins (e.g., misoprostol [Cytotec]) | Motility Macrolides (e.g., erythromycin) Metoclopramide (Reglan) Stimulant laxatives (e.g., bisacodyl [Dulcolax], senna [Senokot]) Malabsorption Acarbose (Precose; carbohydrate malabsorption) Aminoglycosides Orlistat (Xenical; fat malabsorption) Thyroid supplements Pseudomembranous colitis (Clostridioides difficile) Antibiotics (e.g., clindamycin, fluoroquinolones, cephalosporins, penicillin) Antineoplastics Immunosuppressants Proton pump inhibitors (can also cause diarrhea through other mechanisms) |
| Diagnosis | Clinical features | Tests |
|---|---|---|
| Watery diarrhea – functional disorders | Improves at night and with fasting7 | To evaluate for alternative diagnoses: inflammatory bowel disease, celiac disease |
| Functional diarrhea | Rome IV diagnostic criteria; normal abdominal, skin, oral, and rectal examinations; no alarm features3 | CBC, CRP, basic metabolic panel, anti-tissue transglutaminase IgA, total IgA1,3,8 |
| IBS | Rome IV diagnostic criteria; normal abdominal, skin, oral, and rectal examinations; no alarm features3 | CBC, CRP, basic metabolic panel, anti-tissue transglutaminase IgA, total IgA1,3,8 |
| Nonceliac gluten sensitivity | Gluten food trigger, can have systemic symptoms similar to celiac disease9 | Tissue transglutaminase IgA, total IgA, upper gastrointestinal endoscopy with duodenal biopsy to rule out celiac disease8 |
| Paradoxical diarrhea (see page around impacted stool)7 | History of constipation, opioid use; hemorrhoids, impacted stool found during digital rectal examination or anoscopy | Radiography as needed |
| Watery diarrhea – secretory disorders | Nocturnal symptoms and symptoms despite fasting7 | Fecal osmotic gap < 50 mOsm per kg7 |
| Bacterial enterotoxins (e.g., cholera) | Can cause chronic symptoms in immunocompromised patients10 | HIV, stool tests or serology for specific pathogens10 |
| Bile acid malabsorption | Similar to functional diarrhea and IBS1,2,4 | SeHCAT where available, serum C4, FGF19, 48-hour fecal bile acids, trial of cholestyramine (Questran)11 |
| Brainerd diarrhea | History of raw milk consumption, acute diarrhea fails to resolve12 | No specific testing, rule out other diagnoses12 |
| Crohn disease ileitis | Fever, weight loss, arthralgias; family history; abdominal pain and tenderness, perianal disease or fissuring, and skin manifestations13 | CBC, fecal calprotectin, colonoscopy with biopsies and ileoscopy; consider upper gastrointestinal endoscopy13 |
| Endocrine disorders | Fatigue, anxiety; dermatitis or dry skin, tachycardia4 | Thyroid-stimulating hormone, serum electrolytes, adrenocorticotropic hormone stimulation test4 |
| Medications, alcoholism | Table 1, nonosmotic laxative use, alcohol abuse6 | Trial off medication when feasible, treat underlying behavioral health disorders |
| Microscopic colitis | Similar to functional diarrhea and IBS; medication use, smoking14,15 | Colonoscopy with biopsies of normal-appearing mucosa14,15 |
| Neuroendocrine tumors | Carcinoid syndrome (watery diarrhea, flushing, bronchospasm, hypotension, right-sided heart failure), often relatively asymptomatic4 | CT or magnetic resonance imaging, endoscopy, specific hormone assays, based on high index of clinical suspicion4 |
| Postsurgical (gastrectomy, cholecystectomy, vagotomy, intestinal resection) | Surgical history1; surgical scars found during abdominal examination | Bile acid malabsorption after cholecystectomy; small intestinal bacterial overgrowth after intestinal resection |
| Vasculitis (e.g., Behçet syndrome) | Oral and genital aphthosis, uveitis, aneurysm, thrombosis, arthralgia, pseudofolliculitis16 | CBC, CRP, clinical diagnosis often requiring time16 |
| Watery diarrhea – osmotic disorders | Improves with fasting7 | Fecal osmotic gap > 100 mOsm per kg (from 10) |
| Carbohydrate malabsorption (e.g., lactose, fructose); can also cause a fatty malabsorptive diarrhea | Food triggers, family history | Breath tests, trial of food avoidance1 |
| Celiac disease; can also cause a fatty malabsorptive diarrhea | Gluten food trigger, family history, type 1 diabetes mellitus, Down syndrome, neurologic symptoms, dermatitis herpetiformis, iron deficiency anemia8 | Tissue transglutaminase IgA, total IgA, upper gastrointestinal endoscopy with duodenal biopsy, human leukocyte antigen class II DQ2 and DQ8 in certain clinical situations8 |
| Medications, excessive intake of certain foods | Medication and dietary history for osmotic laxative or antacid use and excessive sugar alcohol intake1 | No specific tests |
| Fatty diarrhea malabsorptive disorders | Usually higher than average stool volume7 | Fecal fat (applies to both types of fatty diarrhea) |
| Amyloidosis | Dysphagia, hepatic abnormalities, type 2 diabetes mellitus, cardiac or lung manifestations17; electrocardiogram abnormalities or abnormal pulmonary function testing | Tissue biopsy17 |
| Chronic mesenteric ischemia | Postprandial abdominal pain, history of atherosclerotic or thrombotic disease18; physical examination findings suggesting peripheral vascular disease | Duplex ultrasonography, CT angiogram18 |
| Lymphatic damage (e.g., congestive heart failure, lymphoma) | Fatigue, dyspnea, lymphadenopathy, edema | Chest radiography, echocardiography, other testing based on suspected diagnosis |
| Medications (e.g., orlistat [Xenical], acarbose [Precose]) | Medication history | Trial off medication if feasible |
| Noninvasive small bowel parasite (e.g., Giardia) | History of exposure to untreated water12 | Stool antigen, serum antibodies12 |
| Small intestinal bacterial overgrowth | IBS or functional diarrhea symptoms1 | Hydrogen breath tests, proximal jejunal aspirate with > 105 colony-forming units per mL coliform bacteria1 |
| Structural (e.g., gastric bypass, short bowel syndrome, fistulae) | Surgical history, history of infection or inflammation1 | Radiography or endoscopy as indicated1 |
| Tropical sprue | History of travel or living in endemic areas12 (e.g., tropical regions of Caribbean, South Africa, India, and southeast Asia) | Clinical diagnosis, duodenal biopsy mimics celiac disease12 |
| Whipple disease (Tropheryma whippelii infection) | Arthralgias, cognitive dysfunction, edema, adenopathy12 | Mucosal biopsy, polymerase chain reaction testing, immunohistochemistry12 |
| Fatty diarrhea – maldigestive disorders | Stools may not be very loose7 | Fecal fat (applies to both types of fatty diarrhea) |
| Hepatobiliary disorders | History of risk factors, hepatomegaly, right upper quadrant pain, ascites, sequelae of hepatic disease | Hepatic function tests, right upper quadrant ultrasonography |
| Inadequate luminal bile acid | History of distal ileal disease or resection, rare congenital disorders7 | No specific testing |
| Pancreatic exocrine insufficiency | History of diabetes mellitus, cystic fibrosis, chronic pancreatitis19 | CT, fecal elastase-1, further testing by level of clinical suspicion19 |
| Inflammatory diarrhea | Bloody or purulent stool1 | Presence of fecal leukocytes, blood, lactoferrin, or calprotectin1 |
| Colorectal cancer | Family history, abdominal pain, abdominal mass, weight loss20 | Colonoscopy20 |
| Inflammatory bowel disease | Fever, weight loss, fatigue, skin and joint symptoms, family history13; dermatitis, anal fissures, rectal ulcerations | CBC, fecal calprotectin, colonoscopy with biopsies and ileoscopy13 |
| Invasive bacterial infection (e.g., tuberculosis, yersiniosis) | Pulmonary symptoms, night sweats12 | Colonoscopy with biopsy, chest radiography, serology for specific pathogens12 |
| Invasive parasitic infection (e.g., Entamoeba) | Travel history12 | Stool examination for ova and parasites, stool polymerase chain reaction, serum antibodies12 |
| Ischemic colitis (usually acute but can be chronic) | History of atherosclerotic disease or risk factors | Abdominal CT, colonoscopy4 |
| Pseudomembranous colitis (Clostridioides difficile) | History of antibiotic use, health care environment, immunocompromise10,21; abdominal distension | Nucleic acid amplification tests for toxin genes21 |
| Radiation colitis | History of radiation1 | Colonoscopy or sigmoidoscopy1 |
| Ulcerating viral infections (e.g., herpes simplex, cytomegalovirus) | Vesicular skin lesions, fever, fatigue, lymphadenopathy12 | Colonoscopy with biopsy, serology for specific pathogens, viral culture or polymerase chain reaction test of skin lesions for herpes simplex virus12 |
Physical Examination
A thorough physical examination, including abdominal examination, visual inspection of the anus and perianal skin, and a digital rectal examination, is indicated for any patient who reports chronic diarrhea. Office anoscopy can be helpful in suspected inflammatory disorders.
Diagnostic Approach
The initial laboratory workup should include a complete blood count, C-reactive protein (CRP) level, anti-tissue transglutaminase immunoglobulin A (IgA) level, total IgA level, and a basic metabolic panel.1,8,22 The diagnostic evaluation should be guided by history and physical examination. Alarm features such as anemia, unintentional weight loss, and persistent blood in the stool warrant further investigation.1,2,4 A patient who meets Rome IV diagnostic criteria (Table 33 ) for IBS, has routine physical examination and initial laboratory results, and has no alarm features may be diagnosed with IBS.3
Recurrent abdominal pain, with onset more than 6 months ago, occurring on average at least 1 day per week in the past 3 months associated with two or more of the following criteria:
|
Magnetic resonance imaging or computed tomography imaging with enterography may be performed for patients with alarm features, abnormal laboratory values, or suspected structural disease.4 Colonoscopy should also be performed for patients with alarm features or for whom a reasonable initial workup has failed to yield a diagnosis. When colonoscopy is performed to evaluate chronic diarrhea, multiple mucosal biopsies should be taken, even if the endoscopic mucosal appearance is normal.23
When the initial evaluation fails to narrow the differential diagnosis, testing for fecal occult blood (i.e., fecal immunochemistry test), fecal calprotectin (i.e., leukocytes or lactoferrin), and fecal fat (i.e., Sudan stain) may be helpful to categorize diarrhea as watery, fatty, or inflammatory.1,4 Although this can help narrow the differential diagnosis, it is important to understand that some disorders can cause more than one type of diarrhea.
These three categories can be subdivided further based on a comprehensive fecal analysis including a 24-hour stool mass for the quantification of diarrhea and calculation of fecal components, quantitative fecal fat test (i.e., 24- to 48-hour chemical analysis or quantitative Sudan microscopy), and fecal chemistry test (i.e., pH level, osmolality, electrolytes, and phosphate).24,25 However, these tests are not always readily available and usefulness varies.1,2 When available, they can be helpful in diagnosing a factitious disorder and surreptitious laxative use.25
Watery diarrhea is a loose stool that does not contain leukocytes, lactoferrin or calprotectin, blood, or elevated levels of fecal fat. It can be separated into secretory, osmotic, and functional types. Secretory diarrhea is caused by reduced water absorption, and results in high stool volumes; symptoms persist at night and during fasting. Osmotic diarrhea is caused by water retention in the intestine because of the presence of poorly absorbed solutes; stool analysis revealing high stool osmotic gaps can help distinguish it from other watery diarrheas.7 Functional disorders lack a clear organic etiology and are diagnosed using Rome IV diagnostic criteria. The predominance of pain differentiates between IBS and functional diarrhea.
Fatty diarrhea, characterized by elevated levels of fecal fat, is broken down into malabsorptive and maldigestive types, based on etiology.7
Common Causes
IRRITABLE BOWEL SYNDROME (WATERY – FUNCTIONAL)
Current studies indicate that IBS has a prevalence of 9% to 23% worldwide. If a patient meets Rome IV diagnostic criteria (Table 3; https://www.mdcalc.com/rome-iv-diagnostic-criteria-irritable-bowel-syndrome-ibs) and does not have any alarm features, an extensive workup is not typically recommended.3 It is reasonable to order a complete blood count, CRP (or stool calprotectin), basic metabolic panel, and celiac serology, based on expert opinion and American College of Gastroenterology guidelines for the evaluation of celiac disease.3,4,8 IBS symptoms may sometimes be the presentation of other medical causes of chronic diarrhea, including nonallergic food intolerance and bile acid malabsorption.4 Patients who do not respond to typical IBS treatments may benefit from evaluation for additional diagnoses. There may be an association between small intestinal bacterial overgrowth and IBS; however, there is no definitive evidence that small intestinal bacterial overgrowth causes IBS symptoms. If there is a clinical concern, a glucose breath test can provide additional insight.26
FUNCTIONAL DIARRHEA (WATERY – FUNCTIONAL)
Functional diarrhea is distinct from IBS. Rome IV diagnostic criteria for functional diarrhea are “loose or watery stools, without predominant abdominal pain or bothersome bloating, occurring in greater than 25% of stools” for the past three months, with the onset of symptoms at least six months before diagnosis. Patients who meet the criteria for IBS cannot receive a diagnosis of functional diarrhea. The prevalence of functional diarrhea in adults may be as high as 17%. Functional diarrhea should be diagnosed after a reasonable effort at evaluating for organic disease. Lack of improvement with empiric loperamide (Imodium) should prompt reconsideration of the diagnosis.3
BILE ACID MALABSORPTION (WATERY – SECRETORY)
Bile acid malabsorption is the failure of enterohepatic reabsorption of bile acids in the terminal ileum. It has been found in up to 35% of patients with IBS and microscopic colitis, and it is the underlying reason for diarrhea in ileal disease such as Crohn disease.11 Diarrhea commonly seen after cholecystectomy is attributed to bile acid malabsorption.1 The selenium homotaurocholic acid test is used to diagnose bile acid malabsorption in other countries but is not approved by the U.S. Food and Drug Administration. Where available, serum 7α-hydroxy-4-cholesten-3-one (elevated in bile acid malabsorption) and fibroblast growth factor 19 (low in bile acid malabsorption) have shown promise as initial tests.27 Diagnosis can be made by starting patients on bile acid binders (i.e., cholestyramine [Questran]) and monitoring for improvement.
MICROSCOPIC COLITIS (WATERY – SECRETORY)
Microscopic colitis is estimated to cause 10% to 15% of all secretory diarrheas and is also present in 5% to 10% of patients who are diagnosed with IBS.4,14 Typically, this disease presents in women around 60 years of age, although 25% of occurrences are in women younger than 45 years. The underlying mechanism is unclear; however, it has been associated with celiac disease, suggesting an autoimmune component. Medications such as proton pump inhibitors and nonsteroidal anti-inflammatory drugs have also been implicated. Symptoms include watery diarrhea, abdominal pain, weight loss, arthralgias, and fatigue. A diagnosis is made by colonoscopy with random biopsies because the gross appearance is typically normal.15
INFLAMMATORY BOWEL DISEASE (INFLAMMATORY, WATERY – SECRETORY)
IBD encompasses the diagnoses of Crohn disease and ulcerative colitis. Onset is typically between 10 and 40 years of age.13 The prevalence in North America is 249 per 100,000 people for ulcerative colitis and 319 per 100,000 people for Crohn disease.28 First-degree relatives of patients with IBD are at a 10-fold increased risk of developing IBD themselves.29 Although IBD is usually associated with inflammatory diarrhea, Crohn disease can cause secretory diarrhea. Crohn disease also is commonly associated with extraintestinal manifestations such as arthralgias and erythema nodosum.13 Patients with IBS symptoms and a CRP level less than 0.5 mg per L (4.76 nmol per L) or fecal calprotectin level less than 40 mcg per g have a less than 1% chance of having IBD.30 However, neither CRP nor fecal calprotectin can rule out IBD when clinical suspicion is high or alarm features are present.13
CELIAC DISEASE (FATTY – MALABSORPTIVE, WATERY – OSMOTIC)
Celiac disease, also known as celiac sprue or gluten-sensitive enteropathy, usually causes malabsorptive fatty diarrhea, but it can also cause osmotic diarrhea through bile acid malabsorption.4 It has a prevalence of 0.71% in the United States, is more common among whites and women,31 and the prevalence among those with chronic diarrhea may be as high as 5%.4 Prevalence in first- and second-degree relatives is 5% to 20%.8 Extraintestinal manifestations include dermatitis herpetiformis, neurologic symptoms, iron deficiency anemia, and metabolic bone disease.32 Clinicians should obtain serum anti-tissue transglutaminase and total IgA levels for all patients with chronic diarrhea for whom an apparent alternative diagnosis does not exist,8 including patients meeting criteria for IBS or functional diarrhea.1,4
The diagnosis is confirmed with an upper gastrointestinal endoscopy with duodenal biopsies. When there is a high index of suspicion, duodenal biopsies should be obtained despite normal serology. Patients who are already following a gluten-free diet may have negative antibodies and normal biopsies.8 For those patients, celiac disease can be ruled out if genetic testing for human leukocyte antigen class II DQ2 and DQ8 molecules are negative.8 Celiac disease should be differentiated from nonceliac gluten sensitivity, a disorder with similar symptoms but no celiac-specific antibodies, intestinal structure changes, or evidence of malabsorption.9 A diagnosis of celiac disease carries serious health consequences for even small amounts of gluten consumption and considerations for family members; therefore, all efforts should be made to distinguish actual celiac disease from clinically similar disorders.8
CLOSTRIDIOIDES DIFFICILE COLITIS (INFLAMMATORY)
Most infectious diarrhea is acute and self-limited, but some infections can cause chronic symptoms. One of the most notable of these in resource-rich geographic areas is C. difficile infection, which is commonly associated with antibiotic use and health care environments. Asymptomatic C. difficile colonization is common and found in up to 15% of healthy adults, and not all strains produce toxins.10,21 When antibiotics alter normal gut flora, toxigenic strains of C. difficile can overgrow and produce toxins A and B. These toxins cause inflammatory diarrhea and can lead to the formation of bacterial pseudomembranes.10 Diagnosis is best made with a stool nucleic acid amplification test. Clinicians should only test diarrheal stools to avoid false positives.21
OTHER INFECTIONS (PRIMARY INFLAMMATORY)
Travel to resource-poor environments is a risk factor for many other infectious causes, and so is the consumption of untreated water, unwashed produce, raw dairy, and undercooked meat. In these instances, parasites are more likely than bacteria or viruses to cause chronic diarrhea in immunocompetent patients. Giardiasis is a waterborne, noninvasive, small bowel protozoal infection that leads to malabsorptive diarrhea. If infection is suspected, a stool antigen test is more sensitive than stool examination for ova and parasites. Entamoeba histolytica causes an invasive protozoal infection, usually acquired through the fecal-oral route, that leads to inflammatory diarrhea. Diagnosis is initially made through stool examination for ova and parasites, but this can be falsely positive for nonpathogenic Entamoeba species. Diagnosis can be confirmed with serology or tissue biopsy. Cryptosporidium and Cyclospora are common causes of travelers' diarrhea but can be acquired domestically. Helminth infections, such as Trichuris trichiura (i.e., whipworm) and Ascaris lumbricoides (i.e., roundworm), can usually be diagnosed with stool examination, but specific serologies can increase diagnostic yield when clinical suspicion is high. Eosinophilia is a common laboratory finding. When using stool ova and parasites for diagnosis, testing more than one sample increases the diagnostic yield.12
Chronic bacterial diarrhea is uncommon. Some known pathogens include Tropheryma whippelii (i.e., Whipple disease), Yersinia enterocolitica, and Mycobacterium tuberculosis. Diagnosis requires a high index of suspicion.12
ENDOCRINE DISORDERS (SECRETORY)
Endocrine disorders such as hyperthyroidism, Addison disease, and diabetes mellitus should be suspected as underlying pathologies in disordered gut motility or auto-immune enteropathy when other signs or symptoms of these disorders are present. Endocrine tumors such as carcinoid, VIPomas, and gastrinomas (i.e., Zollinger-Ellison syndrome) are rare. Levels of serum peptides (e.g., gastrin, calcitonin, vasoactive intestinal) should be obtained for patients with images of an endocrine tumor or for patients whose watery diarrhea is undiagnosed despite an appropriate evaluation.4
This article updates a previous article on this topic by Juckett and Trivedi.6
Data Sources: A PubMed search was completed in Clinical Queries using the key terms chronic diarrhea evaluation, chronic diarrhea guidelines, and diagnosis (conditions listed in Table 2). The searches included meta-analyses, randomized controlled trials, clinical trials, and reviews. Also searched were the Cochrane database, UpToDate, the Trip database, and Essential Evidence Plus. Search dates: September 2018 to January 2019, and December 2019.
The opinions or assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the Department of Defense, the U.S. Army Medical Corps, or the U.S. Army at large.