
Am Fam Physician. 2020;101(9):530-540
Patient information: See related handout on protection from ticks, written by the authors of this article.
Author disclosure: No relevant financial affiliations.
Tickborne diseases that affect patients in the United States include Lyme disease, Rocky Mountain spotted fever (RMSF), ehrlichiosis, anaplasmosis, babesiosis, tularemia, Colorado tick fever, and tickborne relapsing fever. Tickborne diseases are increasing in incidence and should be suspected in patients presenting with flulike symptoms during the spring and summer months. Prompt diagnosis and treatment can prevent complications and death. Location of exposure, identification of the specific tick vector, and evaluation of rash, if present, help identify the specific disease. Lyme disease presents with an erythema migrans rash in 70% to 80% of patients, and treatment may be initiated based on this finding alone. RMSF presents with a macular rash starting on the wrists, forearms, and ankles that becomes petechial. RMSF has a higher rate of mortality than other tickborne diseases; therefore, empiric treatment with doxycycline is recommended for all patients, including pregnant women and children, when high clinical suspicion is present. Testing patient-retrieved ticks for infections is not recommended. Counseling patients on the use of protective clothing and tick repellents during outdoor activities can help minimize the risk of infection. Prophylactic treatment after tick exposure in patients without symptoms is generally not recommended but may be considered within 72 hours of tick removal in specific patients at high risk of Lyme disease.
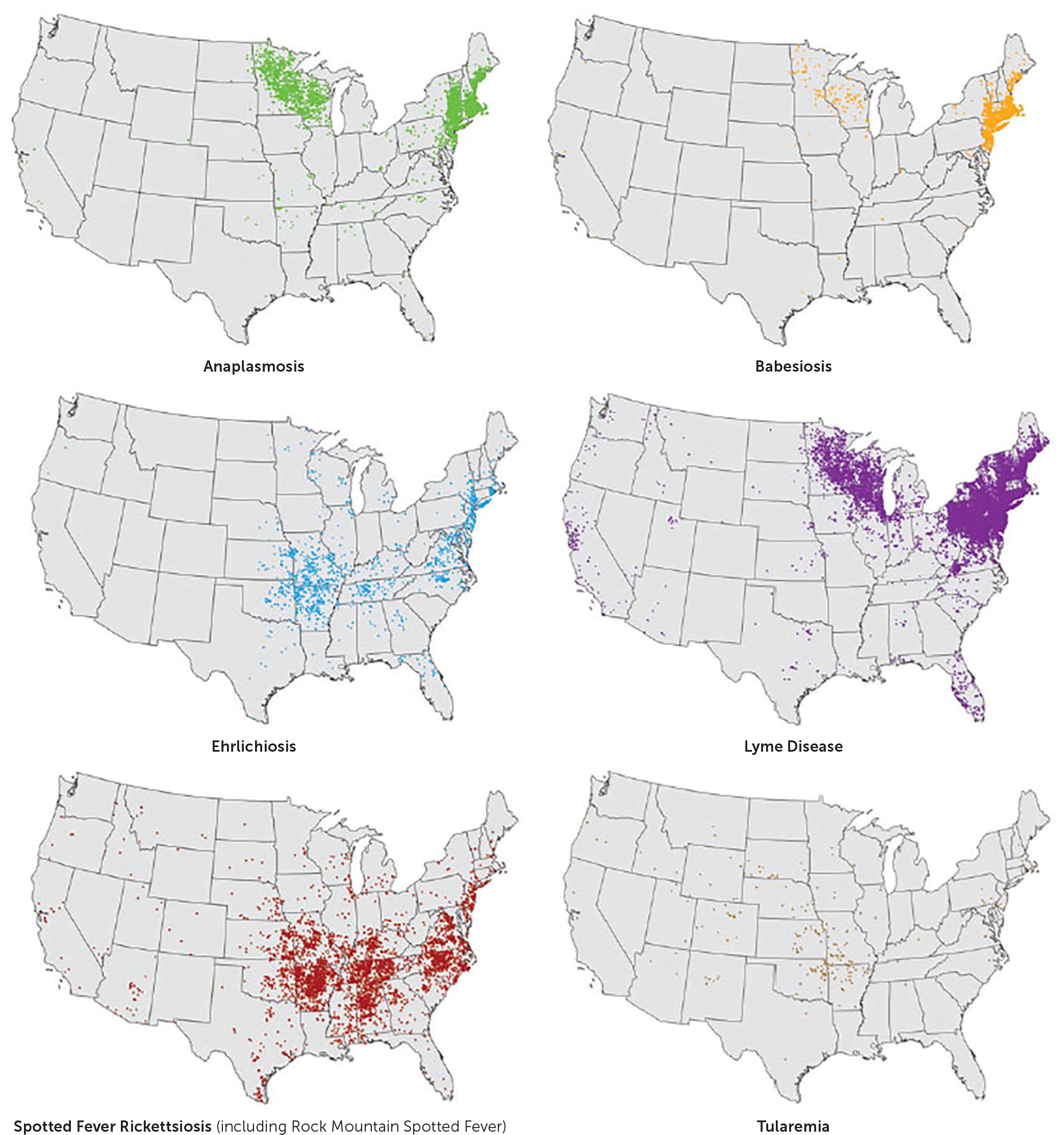
The incidence of tickborne diseases is increasing in the United States.1–3 Diagnosis can be challenging because most patients do not recall being bitten by a tick, initial symptoms are similar and nonspecific, and ticks transmit multiple diseases in the same geographic area. Available diagnostic tests are limited by poor sensitivity early in the disease course, making clinical suspicion and familiarity with common laboratory findings important. Empiric treatment is recommended for tickborne diseases that fit the clinical presentation and geographic distribution. Early doxycycline administration improves morbidity and mortality. Table 11,2,4–18 and Table 21,2,4,5,7–9,13,15–24 summarize the epidemiology and clinical characteristics of tickborne diseases in the United States. Figure 1 highlights tickborne disease geographic distributions.25 Ixodes scapularis (Figure 2) and Dermacentor variabilis (Figure 3) are the ticks that commonly transmit disease in the United States.26
| Recommendation | Sponsoring organization |
|---|---|
| Do not test for Lyme disease as a cause of musculoskeletal symptoms without an exposure history and appropriate examination findings. | American College of Rheumatology |
| Disease | Reported annual incidence | Causative agents | Vectors | Geographic distribution |
|---|---|---|---|---|
| Lyme disease | 30,000 | Borrelia burgdorferi | Black-legged/deer tick (Ixodes scapularis or Ixodes pacificus) | New England, mid-Atlantic states, upper Midwest, northern California |
| Rocky Mountain spotted fever and other spotted fever Rickettsioses: Rickettsia parkeri rickettsiosis, Pacific Coast tick fever, Rickettsial pox | 6,000 | Rickettsia rickettsia R. parkeri Rickettsia species 364D Rickettsia akari | Wood tick (Dermacentor andersoni) American dog tick (Dermacentor variabilis) Brown dog tick (Rhipicephalus sanguineus) | Southeastern and south-central states (Oklahoma, Arkansas, Missouri, Tennessee, and North Carolina account for more than 60% of cases), Arizona and New Mexico |
| Anaplasmosis | 5,000 | Anaplasma phagocytophilum | Black-legged/deer tick (I. scapularis or I. pacificus) | Northeast, Midwest, and West Coast |
| Ehrlichiosis | 1,500 | Ehrlichia chaffeensis Ehrlichia ewingii Ehrlichia muris eauclairensis | Lone Star tick (Amblyomma americanum) Black-legged/deer tick (I. scapularis) American dog tick (D. variabilis) | Southeastern and south-central states |
| Babesiosis | 1,000–2,000 | Babesia microti Babesia duncani | Black-legged/deer tick (I. scapularis or I. pacificus) | Northeast, upper Midwest, few cases in Washington and California |
| Tularemia | Few hundred | Francisella tularensis | Lone star tick (A. americanum) Wood tick (D. andersoni) Dog tick (D. variabilis) | South-central states (Oklahoma, Arkansas, Missouri, and Kansas) |
| Colorado tick fever | 200–300 | Colorado tick fever virus (double-stranded RNA arbovirus) | Wood tick (D. andersoni) | Rocky Mountain region |
| Tickborne relapsing fever | 20–30 | Borrelia species: Borrelia hermsii, Borrelia parkerii, Borrelia turicatae | Ticks of Ornithodoros genus | Rocky Mountain region |
| Disease | Signs and symptoms | Diagnosis | Treatment |
|---|---|---|---|
| Lyme disease | Early localized: EM rash at site of inoculation, flulike symptoms Early disseminated: secondary EM lesions, neurologic (meningitis, facial palsy), musculoskeletal (arthralgias and myalgias), and cardiovascular symptoms (temporary atrioventricular block) Late disseminated: encephalomyelitis, polyarticular arthritis, Lyme carditis | Clinical diagnosis for early localized disease Enzyme-linked immunosorbent assay followed by Western blot assay for unclear or later stage diagnosis | Doxycycline 100 mg twice per day or 4 mg per kg in two divided doses for children > 8 years Amoxicillin 500 mg three times per day or 50 mg per kg in three divided doses for children Cefuroxime axetil (Ceftin) 500 mg twice per day or 30 mg per kg in two divided doses for children Azithromycin (Zithromax) 500 mg once per day or 10 mg per kg per day for children IV ceftriaxone (Rocephin) 2 g per day or 50 to 75 mg per kg per day for children used for neurologic manifestations of late disease Duration of therapy: Early localized: 14 days Early disseminated: 14 to 21 days Late disseminated: 14 to 28 days |
| Rocky Mountain spotted fever | Flulike symptoms with macular rash starting on wrists, forearms, and ankles, becomes petechial | Clinical signs and symptoms including thrombocytopenia and hyponatremia, elevated transaminases, and hyperbilirubinemia IFA is confirmatory but should not delay treatment | Doxycycline 100 mg twice per day or 4 mg per kg for children in two divided doses Chloramphenicol if contraindication to doxycycline Duration of therapy: seven to 10 days |
| Anaplasmosis and ehrlichiosis | Flulike symptoms with gastrointestinal predominance Rash in up to one-third of patients with ehrlichiosis, particularly children | Clinical signs and symptoms including thrombocytopenia, leukopenia, and elevated transaminases IFA is confirmatory but should not delay treatment | Doxycycline 100 mg twice per day or 4 mg per kg for children in two divided doses Rifampin or chloramphenicol if contraindication to doxycycline Duration of therapy: minimum of 10 days, continue for at least three days after fever subsides |
| Babesiosis | Nonspecific flulike symptoms; jaundice may be present | Laboratory findings of hemolytic anemia, thrombocytopenia, elevated transaminases Thin blood smear with characteristic “Maltese cross” pattern or PCR | Atovaquone (Mepron) 750 mg twice per day or 40 mg per kg in two divided doses for children plus azithromycin 500 mg on day one followed by 250 mg per day or 10 mg per kg on day one followed by 5 mg per kg per day for children Duration of therapy: seven to 10 days IV clindamycin plus oral quinine and/or exchange transfusion for severe disease |
| Tularemia | Flulike symptoms, cutaneous eschar at site of inoculation, and painful regional lymphadenopathy | History of exposure to rabbits and other rodents or ticks, leukocytosis Culture is the dianostic standard for diagnosis of tularemia, but has biosafety concerns; PCR or paired serologies may also be used | Intramuscular streptomycin 2 g in two divided doses or 15 mg per kg in two divided doses for children Intramuscular gentamicin or IV 5 mg per kg in two divided doses Duration of therapy: seven to 10 days |
| Colorado tick fever | Triad of high fever (up to 104°F [40°C]), severe myalgias, and headache; fever is often biphasic; “saddle-back” pattern | Common laboratory findings of leukopenia and thrombocytopenia Reverse-transcriptase PCR or paired sample serologic testing | Supportive care only |
| Tickborne relapsing fever | Flulike symptoms with high fever in relapsing or remitting pattern | Detection of spirochetes in blood using dark field microscopy or specific staining | Doxycycline 100 mg twice per day or tetracycline 500 mg every 6 hours for adults Erythromycin 500 mg four times per day for pregnant women or 30 to 50 mg per kg in four divided doses for children IV ceftriaxone or penicillin G for patients with central nervous system involvement Duration of therapy: seven to 10 days Jarisch-Herxheimer reactions common with treatment |


Lyme Disease
EPIDEMIOLOGY
Lyme disease is the most common tickborne disease in the United States. It continues to be most prevalent in New England and the mid-Atlantic region, with increasing cases in the Midwest and northern California. It is caused by the spirochete Borrelia burgdorferi and is transmitted by the blacklegged tick (I. scapularis or Ixodes pacificus). The tick must be attached for 36 to 48 hours to transmit disease.1,4
SIGNS AND SYMPTOMS
Early localized symptoms include fever, chills, fatigue, headache, and myalgias. An erythema migrans (EM) rash occurs in 70% to 80% of patients.1 The rash begins at the site of the tick bite after three to 30 days.1,4 EM is characterized by an expanding erythematous patch that initially appears homogenous and may exhibit partial central clearing over a few days (Figure 427). It typically fades in three to four weeks.1

Early disseminated symptoms occur days to weeks after the initial rash appears and include neurologic, musculoskeletal, and cardiovascular symptoms, and possibly multiple EM lesions.19 Late disseminated symptoms include encephalomyelitis, polyarthritis, and persistent atrioventricular block (Lyme carditis).1,4
DIAGNOSIS
Obtain serologic tests in patients with suggestive symptoms that do not include EM rash. The currently accepted testing algorithm is a two-tiered test with enzyme-linked immunosorbent assay (ELISA) or indirect immunofluorescence assay (IFA) for B. burgdorferi antibodies, followed by Western blot if either of the other test results are positive.1,4,20 Sensitivity of two-tiered testing is less than 50% in early localized disease compared with 90% or greater in subsequent stages.28,29
In July 2019, the U.S. Food and Drug Administration approved the use of new serologic tests for Lyme disease. The Centers for Disease Control and Prevention now recommend that a modified algorithm using a second ELISA test instead of a Western blot is also acceptable to diagnose Lyme disease; therefore, avoiding the confusion of interpreting immunoblot results.30
TREATMENT
Doxycycline, amoxicillin, or cefuroxime axetil (Ceftin) are recommended as first-line treatments for Lyme disease. Doxycycline is preferred in the absence of contraindications but should be avoided in pregnant women and children younger than eight years.4,21 Macrolides are an alternative for patients who are allergic to penicillins or unable to take tetracyclines. People with late neurologic symptoms require intravenous ceftriaxone (Rocephin) or penicillin G benzathine. Treatment should be continued for 14 to 28 days, depending on the stage of infection (Table 21,2,4,5,7–9,13,15–24). Patients with persistent Lyme arthritis after treatment may be treated with a second course of antibiotics. Patients with neurologic disease may have sequelae after treatment, but additional antibiotics are not recommended unless there is objective evidence of relapse or reinfection.1,4
Up to 10% to 20% of patients infected with Lyme disease are symptomatic despite receiving appropriate antibiotic therapy. The Centers for Disease Control and Prevention and the Infectious Disease Society of America use the term “post-Lyme disease syndrome” to describe vague symptoms that persist for greater than six months after completion of antibiotic therapy.1,4 The etiology of these symptoms is unclear. Some patients may have an untreated coinfection with another tickborne disease, such as babesiosis. Others may have another medical condition that explains their symptoms. Studies have found insufficient evidence that patients with post-Lyme disease syndrome have ongoing objective clinical signs of Lyme disease.4 Antibiotic use should not be extended in these patients as studies have shown no benefit in improving symptoms.4,31–35
Rocky Mountain Spotted Fever
EPIDEMIOLOGY
Rocky Mountain spotted fever (RMSF) is the most lethal tickborne disease in the United States with a mortality rate of 5% to 10%.2 As of January 2010, cases of RMSF are reported under a new category called spotted fever rickettsiosis. Spotted fever rickettsiosis encompasses similar Rickettsial infections spread by ticks and mites (Table 11,2,4–18). Most cases occur in adults older than 40 years, but mortality is highest in children younger than 10 years.2,5
SIGNS AND SYMPTOMS
RMSF causes a rapidly progressing small vessel vasculitis. Initial signs and symptoms include fever, headache, rash, nausea and vomiting, and myalgias. Symptom onset is typically five to seven days after inoculation.2,22 Although 90% of patients eventually develop a rash, less than 50% present with rash initially. The rash starts as macules on the wrists, forearms, and ankles. It spreads to the trunk, and sometimes the palms and soles, and ultimately becomes petechial (Figure 537).5,22 Late complications include pulmonary hemorrhage and edema, acute respiratory distress syndrome, myocarditis, acute renal failure, and cerebral edema.5

DIAGNOSIS
RMSF should be high on the differential diagnosis list for patients with flulike symptoms in the spring and summer in endemic areas. Treatment should not be delayed if clinical suspicion for the disease is high.5 Laboratory results that are found with an untreated disease include thrombocytopenia, hyponatremia, elevated transaminases, and hyperbilirubinemia.2
TREATMENT
The first-line treatment for RMSF is doxycycline. Typical antibiotic duration is seven to 10 days, or for at least three days after the fever resolves. Early administration of doxycycline is the most important factor influencing the survival of patients with RMSF.5,6,38 Doxycycline should be given to all patients with suspected RMSF, including children younger than eight years and pregnant women. Although tetracyclines have historically been avoided in young children and pregnant women because of concerns about teratogenicity and dental staining of permanent teeth, data suggests that these risks are low in patients treated specifically with doxycycline for the short duration required for RMSF.5,6,38–40
Chloramphenicol is the only other antibiotic effective against R. rickettsia but is associated with a higher mortality rate than treatment with tetracyclines. Oral chloramphenicol is not available in the United States, and supplies of the intravenous formulation are limited. It should only be used in patients with a contraindication to doxycycline.2,5
Ehrlichiosis and Anaplasmosis
EPIDEMIOLOGY
SIGNS AND SYMPTOMS
Signs and symptoms of ehrlichiosis and anaplasmosis include fever, chills, headaches, and myalgias. Gastrointestinal symptoms, including nausea and vomiting, may be prominent. Symptoms appear five to 14 days after exposure. Rash—ranging from maculopapular to petechial to diffuse erythema—occurs in up to one-third of people infected with Ehrlichia chaffeensis and presents more often in children than adults.2 Anaplasmosis rarely presents with a rash. Late manifestations of untreated illness include meningoencephalitis, respiratory failure, uncontrolled bleeding, and organ failure. The fatality rate is 3% with ehrlichiosis and less than 1% with HGA.2,7,40
DIAGNOSIS
The diagnosis of erhlichiosis and HGA should be considered in patients with flulike symptoms with gastrointestinal predominance and associated laboratory findings of leukopenia, thrombocytopenia, and elevated transaminases.2 Confirmative testing should not delay treatment.4 Polymerase chain reaction (PCR) or the presence of morulae on blood smear are helpful if positive; however, negative results do not rule out disease. The preferred method for confirming either disease is IFA. Similar to the evaluation of RMSF, paired acute and convalescent serologies should be obtained two to four weeks apart. A fourfold increase in IgG titers is diagnostic.7,8
TREATMENT
The treatment of choice for ehrlichiosis and anaplasmosis is doxycycline for a minimum of 10 days, continuing for at least three days after resolution of the fever. The benefits of doxycycline outweigh the risks, even in pregnant women and children. Early treatment is imperative.2,4,23 Patients who cannot tolerate tetracyclines can be treated with a seven- to 10-day course of rifampin.2,4,23
Babesiosis
EPIDEMIOLOGY
The epidemiology of babesiosis, caused by the parasite Babesia microti, has changed from a few isolated cases to the establishment of endemic areas in the past 15 to 20 years4,9–12 (Table 11,2,4–18). In addition to being transmitted by I. scapularis tick bites, babesiosis can also be transmitted through a blood transfusion.4,9
SIGNS AND SYMPTOMS
DIAGNOSIS
Microscopic identification of Babesia with the characteristic “Maltese cross” on Giemsa stain of thin blood smears is diagnostic but has poor sensitivity because of the high parasite burden required for visualization.4,9 PCR allows diagnosis when parasitemia is low and does not require microscopy expertise. Serology can detect antibabesial antibodies but may be negative early on.9,41 Laboratory evaluation may reveal hemolysis, thrombocytopenia, proteinuria, and elevated transaminases.4,9
TREATMENT
Tularemia
Tularemia is caused by the bacterium Francisella tularensis and is transmitted to humans in numerous ways including tick and other insect bites, handling infected tissue, ingesting undercooked meat of other infected mammals, and, rarely, by inhalation of bacteria.13
SIGNS AND SYMPTOMS
Tularemia may present as one of several clinical syndromes, including ulceroglandular, oropharyngeal, pneumonic, and typhoidal tularemia, depending on the route of infection.13 Tickborne cases of tularemia result in ulceroglandular disease, with painful regional lymphadenopathy and a cutaneous eschar at the site of the tick bite.22 Other symptoms include fever, chills, malaise, headache, vomiting, and diarrhea.13
DIAGNOSIS
A culture of the infected tissue should be obtained to diagnose tularemia.13 Appropriate biosafety standards are necessary when handling samples to prevent aerosolization and the spread of disease. Most laboratories in the United States do not have this capability.22 Alternative testing (PCR, immunohistochemistry staining, or serology) is often used to minimize this risk.13
TREATMENT
Colorado Tick Fever
SIGNS AND SYMPTOMS
Symptoms of CTF typically start three to five days after inoculation and last seven to 10 days. High fever, severe myalgias, and headache are common symptoms. The classic biphasic fever is referred to as a “saddle-back” pattern. Other symptoms include pharyngitis, conjunctival injection, photophobia, retro-orbital pain, and nonspecific rash. Uncommon complications include encephalitis, myocarditis, pneumonitis, hepatitis, and disseminated intravascular coagulation.15
DIAGNOSIS
Serologic testing may be used to diagnose CTF, but antibodies are often not detected for two or more weeks after the illness presents.15 Reverse-transcriptase PCR, if available, can confirm the diagnosis in the first few days of illness.16 Common laboratory findings include leukopenia and thrombocytopenia.15
TREATMENT
There is no specific treatment for CTF. Supportive care is appropriate.15
Tickborne Relapsing Fever
EPIDEMIOLOGY
Unlike other ticks that live in tall brush and grass, the Ornithodoros tick species that spread tickborne relapsing fever live in rodent burrows. Most people are infected while staying in rodent-infested cabins.17
SIGNS AND SYMPTOMS
Symptoms of tickborne relapsing fever begin about seven days after exposure and include high fever, headache, myalgias, arthralgias, and nausea.17 Fever lasts about three days and ends with rigors, tachycardia, and hypertension, followed by profuse sweating and defervescence. Symptoms dissipate for about seven days, and then the cycle repeats.18 Uncommon complications include meningitis, acute respiratory distress syndrome, iritis, uveitis, and myocarditis.17
DIAGNOSIS
TREATMENT
Tetracyclines are the preferred treatment for adults with tickborne relapsing fever. Children younger than eight years and pregnant women should be treated with erythromycin. Patients with central nervous system involvement should be treated with intravenous ceftriaxone or penicillin G. Duration of therapy is seven to 10 days.18 Jarisch-Herxheimer reactions—attributed to large cytokine release and characterized by fever, rigors, and hypotension—are common with the initiation of treatment. Patients with a reaction may require hospitalization for supportive care including cooling blankets, fluids, and antipyretics.17,18
Emerging Conditions
Southern tick-associated rash illness is an emerging infection in the southeastern United States and is spread by the Lone Star tick. The infectious etiology is unknown, and it causes a rash similar to EM and is often treated with doxycycline.46,47 Additionally, the bite of a Lone Star tick can lead to the development of alpha-gal (galactose-alpha-1,3-galactose), an anaphylactic mammalian meat allergy.48,49
Powassan virus is a rare but serious cause of encephalitis in the United States, with increased incidence in the past 15 years.50,51 It is transmitted by Ixodes ticks in northeastern and north-central states. The fatality rate is 10% to 15%, and more than 50% of survivors have ongoing cognitive sequelae.52 There is no known treatment.50,52
Tick Analysis
Patients may bring in a tick for analysis after a bite. Although commercial tests are available, there is currently no recommended role for testing ticks for infection. The presence of a pathogen in a tick does not predict disease in the patient that has been exposed, and negative testing may provide false reassurance. Patients should be monitored for symptoms and treatment initiated if a disease develops.1,4
Prevention
Protective clothing and tick repellents are effective in reducing the risk of tickborne diseases.56,57 Long-sleeved shirts tucked into pants and pants tucked into socks limit exposed skin for ticks to bite.3,4 Repellents containing N,N-diethyl-m-toluamide (DEET), Picardin, and IR3535 provide effective protection against ticks.58 DEET is safe in the second and third trimester of pregnancy and for children older than two months of age.4,19 IR3535 is the most effective agent against I. scapularis.59 Permethrin can be sprayed on clothing to also repel ticks.3
Checking for ticks after outdoor activities is recommended. Use blunt forceps to remove ticks manually (tick removal was discussed in a previous issue of American Family Physician60). Alternative methods of tick removal are ineffective and may lead to retention of part of the tick in the skin, causing infection or granuloma formation.19
This article updates previous articles on this topic by Bratton and Corey19 and by Gayle and Ringdahl.61
Data Sources: A PubMed search was completed using the key terms tickborne disease, Lyme disease, Rocky Mountain spotted fever, ehrlichiosis, anaplasmosis, tularemia, Colorado tick fever, tickborne relapsing fever, Southern tick-associated rash illness, alpha-gal, Powassan virus, Borrelia miyamotoi, and tick paralysis. The search included meta-analyses, randomized controlled trials, clinical trials, and reviews. Also searched were the Cochrane database, DynaMed, and Essential Evidence Plus. Search dates: August 5, 2019, and March 4, 2020.
The views expressed in this article are those of the authors and do not reflect the official policy of the U.S. Navy, the U.S. Department of Defense, or the U.S. government.
