
Am Fam Physician. 2020;101(11):669-679
This is part II of a two-part article on nerve blocks. “Part I, Upper Extremity,” appears in this issue of AFP.
Author disclosure: No relevant financial affiliations.
Family physicians use anesthesia to provide diagnostic and procedural analgesia for conditions such as neuropathies, fracture reduction, foreign body removals, and complex wound management. Local infiltration of anesthetics is commonly used in this setting because of the ease of use, safety, and effectiveness of the procedure. Nerve blocks are a specific regional anesthesia technique that blocks nerve function distal to the injection site. An understanding of the sensory distribution of the peripheral nervous system is essential in determining the safest and most effective nerve block for the procedure. There are various nerve block techniques, including landmark-guided and ultrasound-guided. Ultrasound guidance increases the effectiveness of the nerve block while decreasing complications when compared with other techniques. Depending on the required area of anesthesia for the procedure, various points throughout the lower extremity can be used to block the lateral femoral cutaneous, common peroneal, saphenous, tibial, deep peroneal, superficial peroneal, and sural nerves.
Family physicians use various techniques to provide effective anesthesia in outpatient procedures, including local, field, or nerve blocks. Local infiltration of anesthetics is commonly used in this setting because of the ease of use, safety, and effectiveness of the procedure. Local anesthesia is provided by infiltrating the anesthetic into the procedural field, whereas field blocks are performed by infiltrating the anesthetic around the procedural area, leaving the procedural field undisturbed. Both of these procedures anesthetize branches of sensory nerves locally. This article, part II of a two-part series, focuses on nerve blocks of the lower extremity. Part I discusses the guiding principles of nerve block administration and nerve blocks of the elbow and wrist.1
| Clinical recommendation | Evidence rating | Comments |
|---|---|---|
| Preprocedural tibial nerve blocks effectively reduce the pain of plantar fascia injections.8,9 | B | Small, low-quality randomized controlled trials |
| The location for an ultrasound-guided superficial peroneal nerve block is different than that for a landmark-guided injection. The nerve is smaller at the landmark-guided location and challenging to identify with ultrasonography, whereas the nerve is larger at the ultrasound-guided location but has a variable position.12 | C | Expert clinical review |
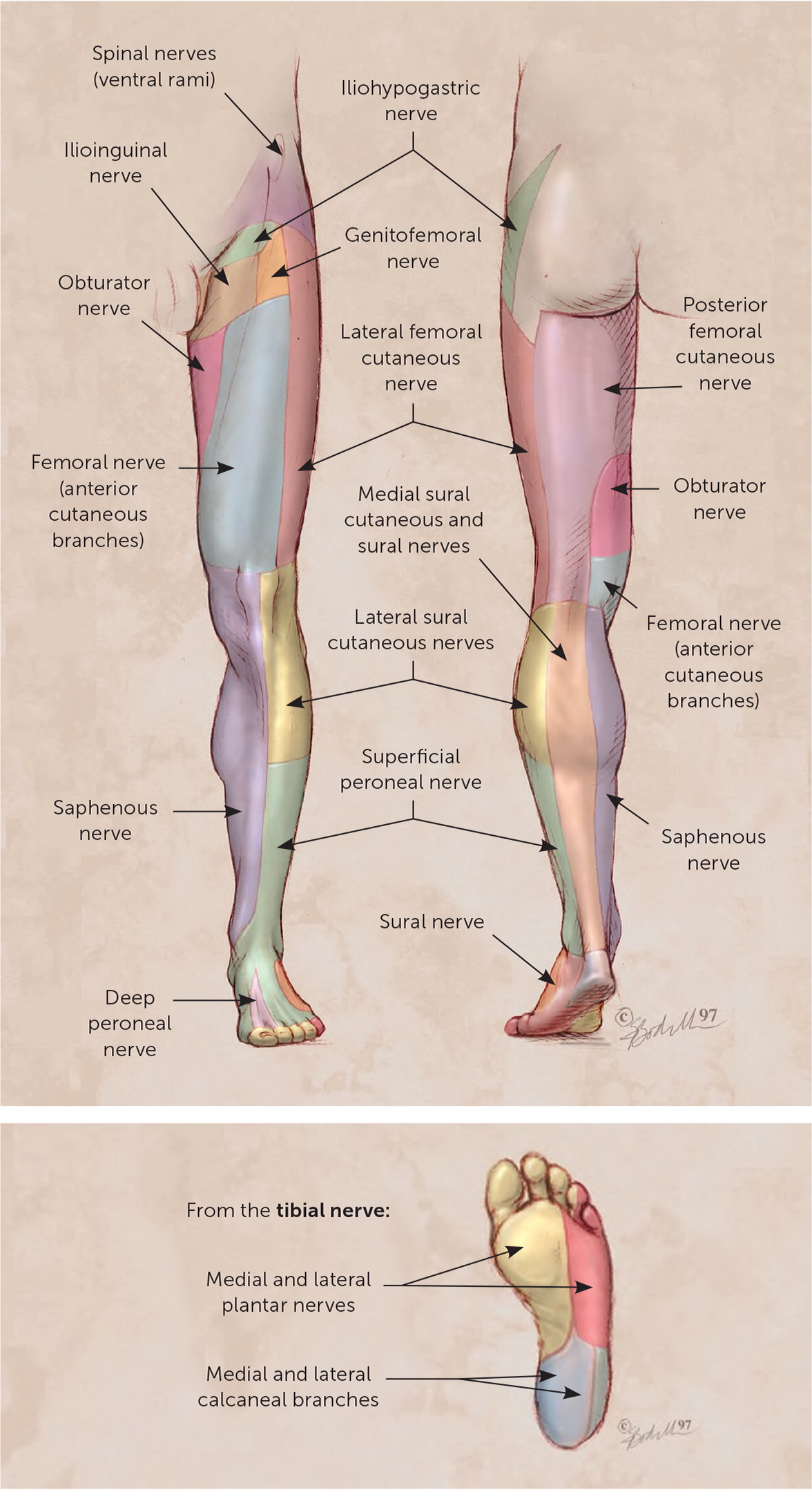
Nerve blocks are used in managing conditions such as neuropathies, fracture reduction, foreign body removals, and complex wounds. Table 1 lists conditions that warrant consideration for lower extremity nerve blocks. Nerve blocks are performed by infiltrating an anesthetic in the perineural space of the sensory nerves that innervate the procedural area. The nerve block is performed proximal to the site of the procedure, providing regional anesthesia distal to the block. Figure 1 illustrates cutaneous innervation of the lower extremity.2
| Nerve | Indication |
|---|---|
| Lateral femoral cutaneous nerve | Meralgia paresthetica or procedures on the anterior thigh |
| Distal sciatic nerve | Any procedure crossing multiple dermatomes of the lower leg |
| Ankle* | |
| Saphenous nerve | Procedures over the medial malleolus |
| Tibial nerve | Tarsal tunnel or plantar fascia injection |
| Deep peroneal nerve | Procedures around the first web space |
| Superficial peroneal nerve | Procedures on the dorsum of the foot |
| Sural nerve | Procedures on the posterior lateral calf or the dorsolateral little toe |
The nerves that are blocked and the anatomic location in which they are blocked determine the area of regional anesthesia. Therefore, a thorough understanding of the relevant anatomy is critical for physicians to perform nerve blocks via a landmark-guided or ultrasound-guided technique. Ultrasound guidance increases the effectiveness of the nerve block while decreasing complications when compared with other techniques.3 Depending on the required area of anesthesia for the procedure, various points throughout the lower extremity can be used to block the lateral femoral cutaneous, common peroneal, saphenous, tibial, deep peroneal, superficial peroneal, and sural nerves.
Lateral Femoral Cutaneous Nerve Block
ANATOMY
The lateral femoral cutaneous nerve arises from the lumbar plexus and runs laterally along the psoas muscle toward the anterior superior iliac spine under the lateral inguinal ligament to the anterolateral thigh (Figure 24). The lateral femoral cutaneous nerve is a sensory nerve formed from the fibers of the L2–L3 nerve roots and provides sensation to the proximal two-thirds of the anterolateral thigh. Indications for a lateral femoral cutaneous nerve block include treating meralgia paresthetica and differentiating the source of anterior upper thigh pain.5
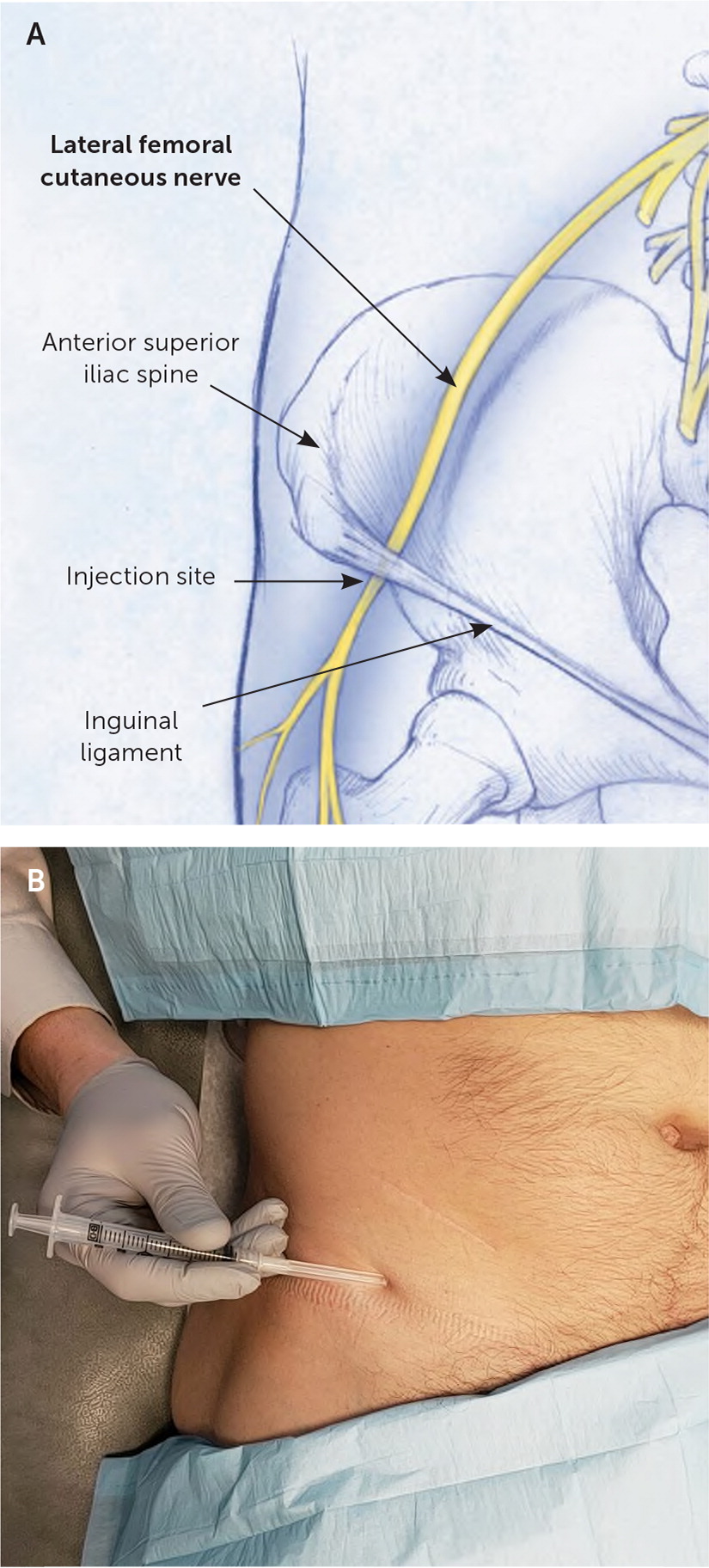
LANDMARK-GUIDED INJECTION
The patient is in the supine position, and the physician palpates the anterior superior iliac spine. Starting 2 cm medial and 2 cm caudal to the anterior superior iliac spine, the needle is advanced toward the midline at a 30- to 45-degree angle, approximately 1 cm deep, where the agent is injected (Figure 24).
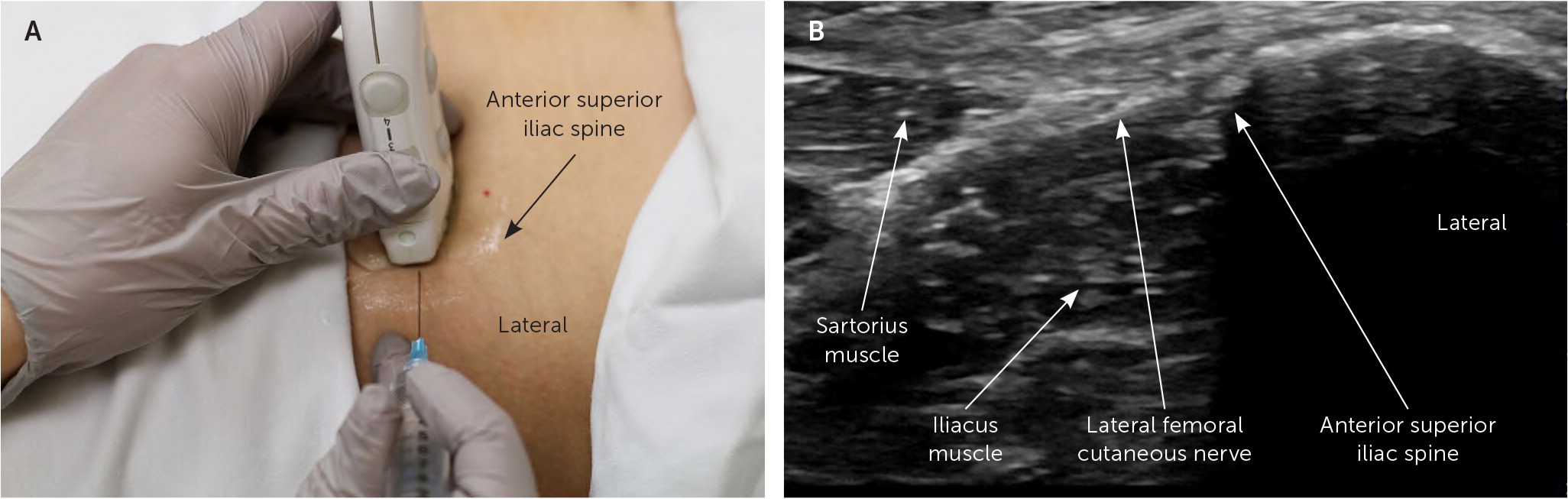
ULTRASOUND-GUIDED INJECTION
The patient is in a supine position, and the lateral portion of the transducer is placed transversely over the inguinal ligament just medial to the anterior superior iliac spine. From this location, the lateral femoral cutaneous nerve is visualized below the inguinal ligament in between the sartorius muscle and the anterior superior iliac spine. The agent is injected into the perineural space by advancing the needle from lateral to medial in plane with the ultrasound transducer6 (Figure 3). If the nerve is difficult to visualize because of its small size, the agent may be injected into the plane of connective tissue between the sartorius muscle and the anterior superior iliac spine.
Distal Sciatic Nerve Block
ANATOMY
The sciatic nerve is the largest nerve in the body. It originates from the lumbosacral plexus and enters the lower extremity through the greater sciatic notch.5 After exiting the pelvis, it traverses lateral to the ischial tuberosity and below the piriformis and gluteus maximus muscles. In the thigh, it courses anterior to the hamstring muscles and divides in the popliteal fossa into the tibial and common peroneal nerves (Figure 4).
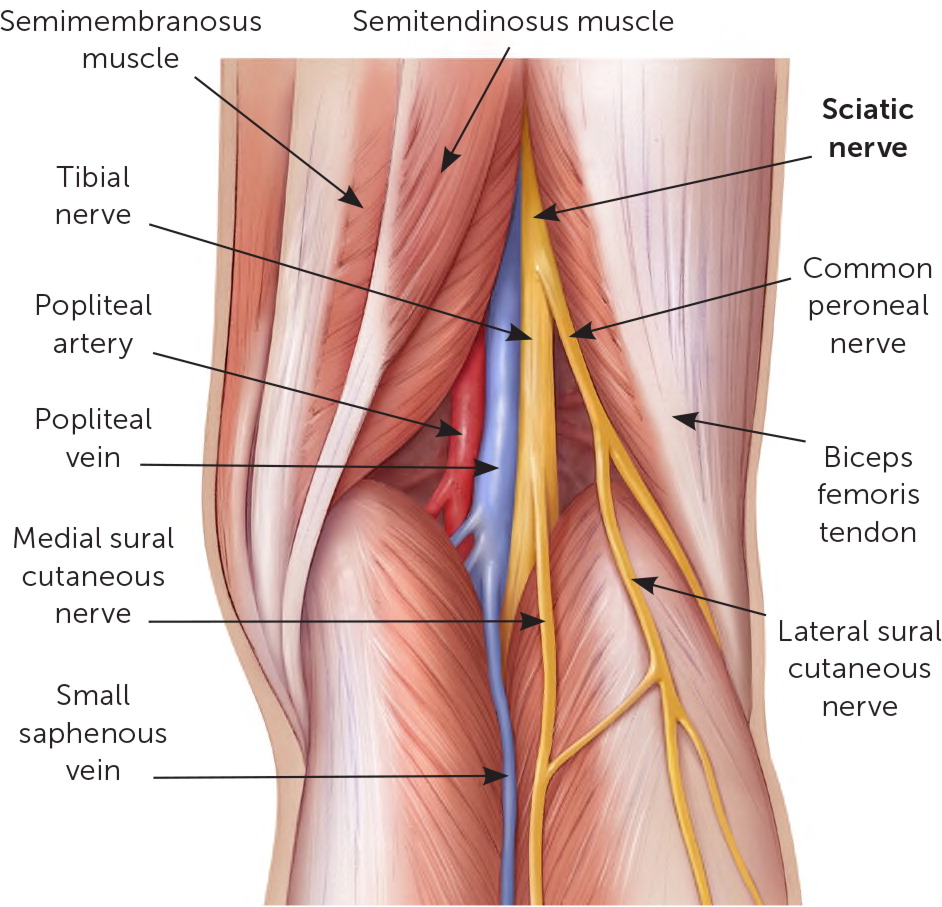
The sciatic nerve is a mixed sensory and motor nerve formed from the fibers of the L4-S3 nerve roots. A distal sciatic nerve block proximal to the bifurcation in the popliteal fossa provides anesthesia for the common peroneal nerve and tibial nerve distributions while sparing the hamstrings.
A distal sciatic nerve block can be especially helpful for procedures that cross multiple dermatomes or for managing large lesions that would require a large amount of anesthesia for a field block. Because of the close proximity of vascular structures and uncertainty of the level of bifurcation, a landmark-guided injection is not recommended for this procedure.
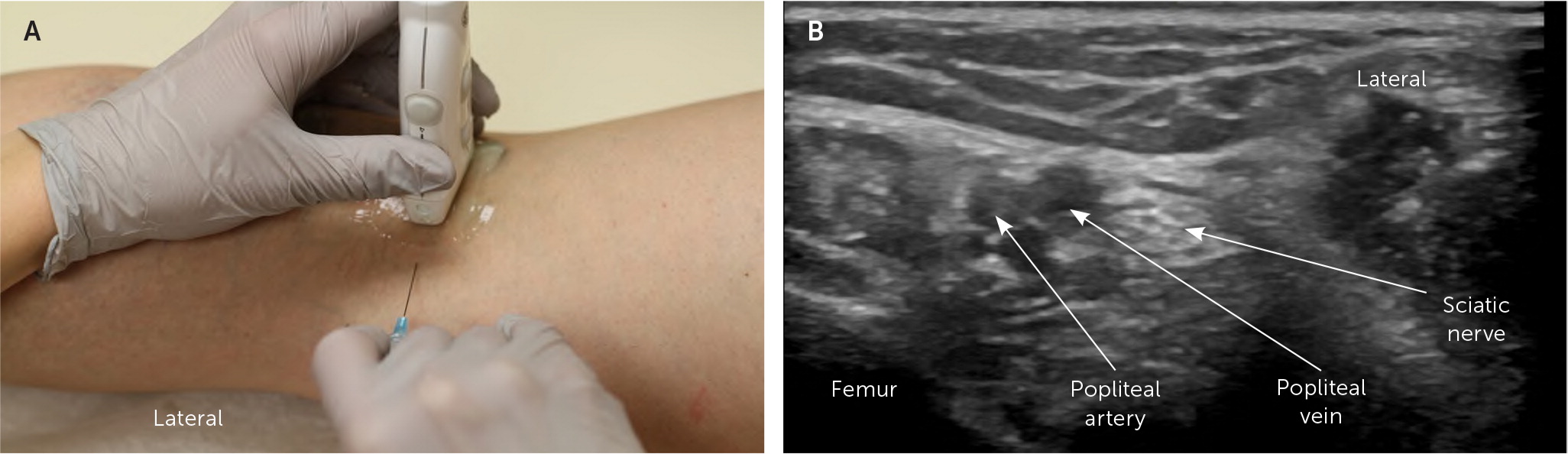
To perform an ultrasound-guided distal sciatic nerve block, the patient is in a prone position with the transducer placed transversely on the posterior thigh, approximately 5 cm above the femoral condyles. The nerve is identified lateral to the popliteal artery and vein.
The agent is injected into the perineural space by advancing the needle from medial to lateral in plane with the transducer (Figure 5). This injection may require a longer needle. A 22-gauge or 25-gauge, 3.5-inch needle is recommended.
Saphenous Nerve Block (Ankle)
ANATOMY
The saphenous nerve is a terminal branch of the femoral nerve and passes through the adductor canal medial to the vastus medialis muscle. Distal to the knee, it traverses superficially along the anteromedial lower leg traveling with the great saphenous vein. At the ankle, the nerve continues to the medial foot anteromedial to the medial malleolus (Figure 6).
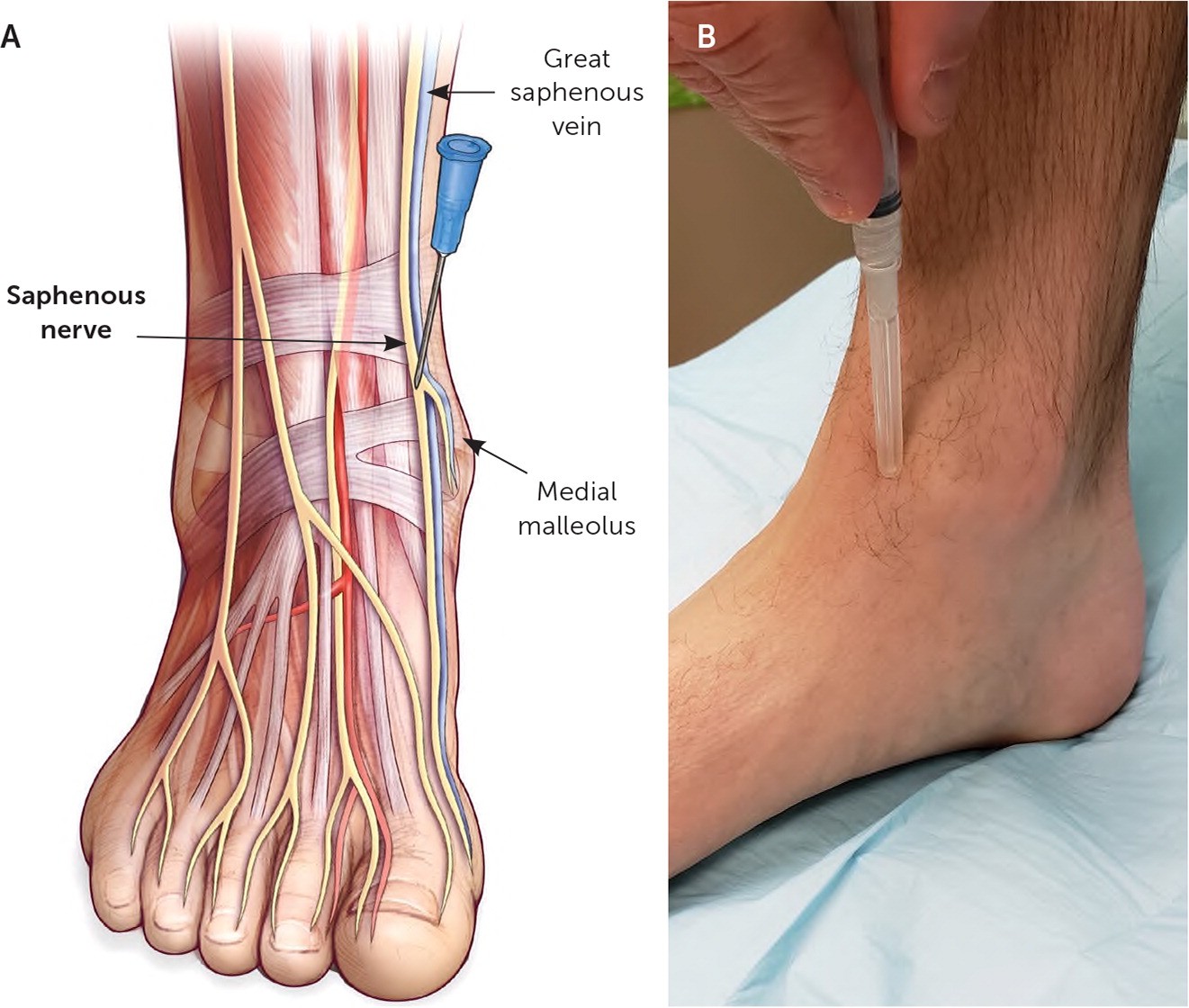
The saphenous nerve is a sensory nerve formed from the fibers of the L2–L4 nerve roots. It provides sensation to the anteromedial thigh and lower leg, as well as the medial ankle and medial foot.
LANDMARK-GUIDED INJECTION
The patient is in a supine position with the knee flexed and the foot resting on the table. The needle enters the subcutaneous tissue just proximal and anterior to the medial malleolus. It is advanced posteromedially at a 45-degree angle, depositing a track of anesthesia for about 3 to 4 cm in the subcutaneous tissue toward the great saphenous vein (Figure 6).
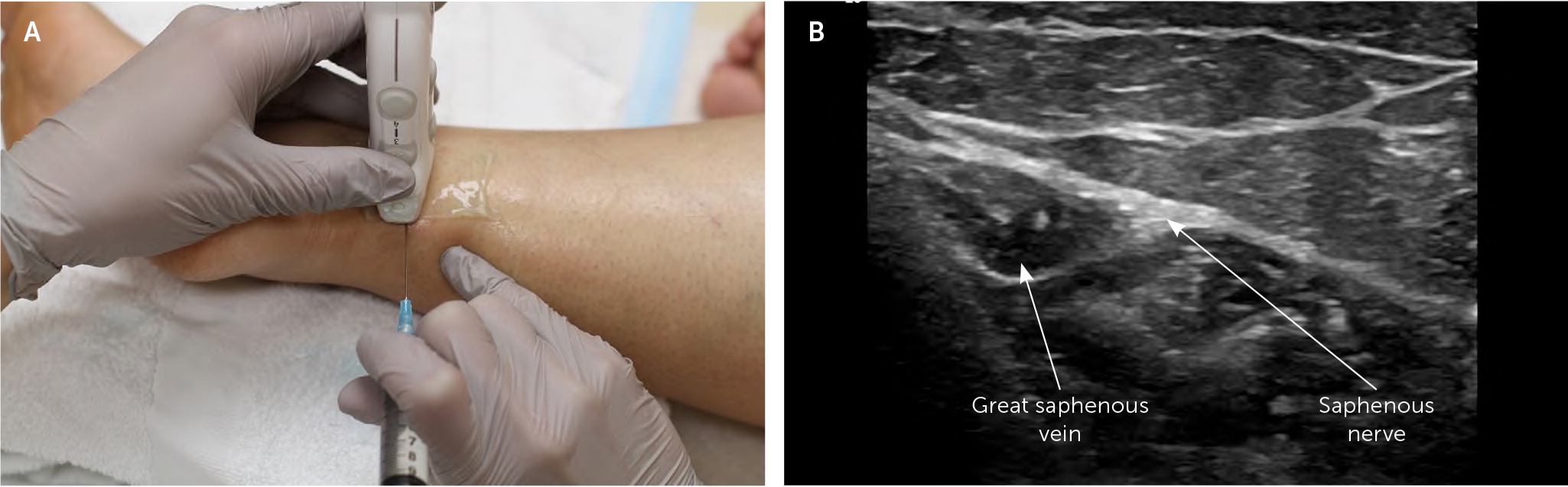
ULTRASOUND-GUIDED INJECTION
The patient is in the lateral recumbent position on the affected side to expose the medial ankle. The transducer is placed transversely over the malleolus. The saphenous nerve is located adjacent to the great saphenous vein at the level of the medial malleolus. The agent is injected into the perineural space by advancing the needle from posterior to anterior in plane with the transducer (Figure 7).
Tibial Nerve Block (Ankle)
ANATOMY
The tibial nerve originates from the sciatic nerve in the popliteal fossa. It traverses underneath the soleus muscle in the deep posterior compartment distal to the knee. At the ankle, it travels in the tarsal tunnel posterior to the posterior tibial artery 7 (Figure 8). The tibial nerve is a mixed sensory and motor nerve formed from the fibers of the L4-S2 nerve roots and provides sensation to the heel and plantar surface of the foot. A 2017 Cochrane review and a 2003 randomized controlled trial demonstrated that preprocedural tibial nerve blocks effectively reduce the pain of plantar fascia injections.8,9
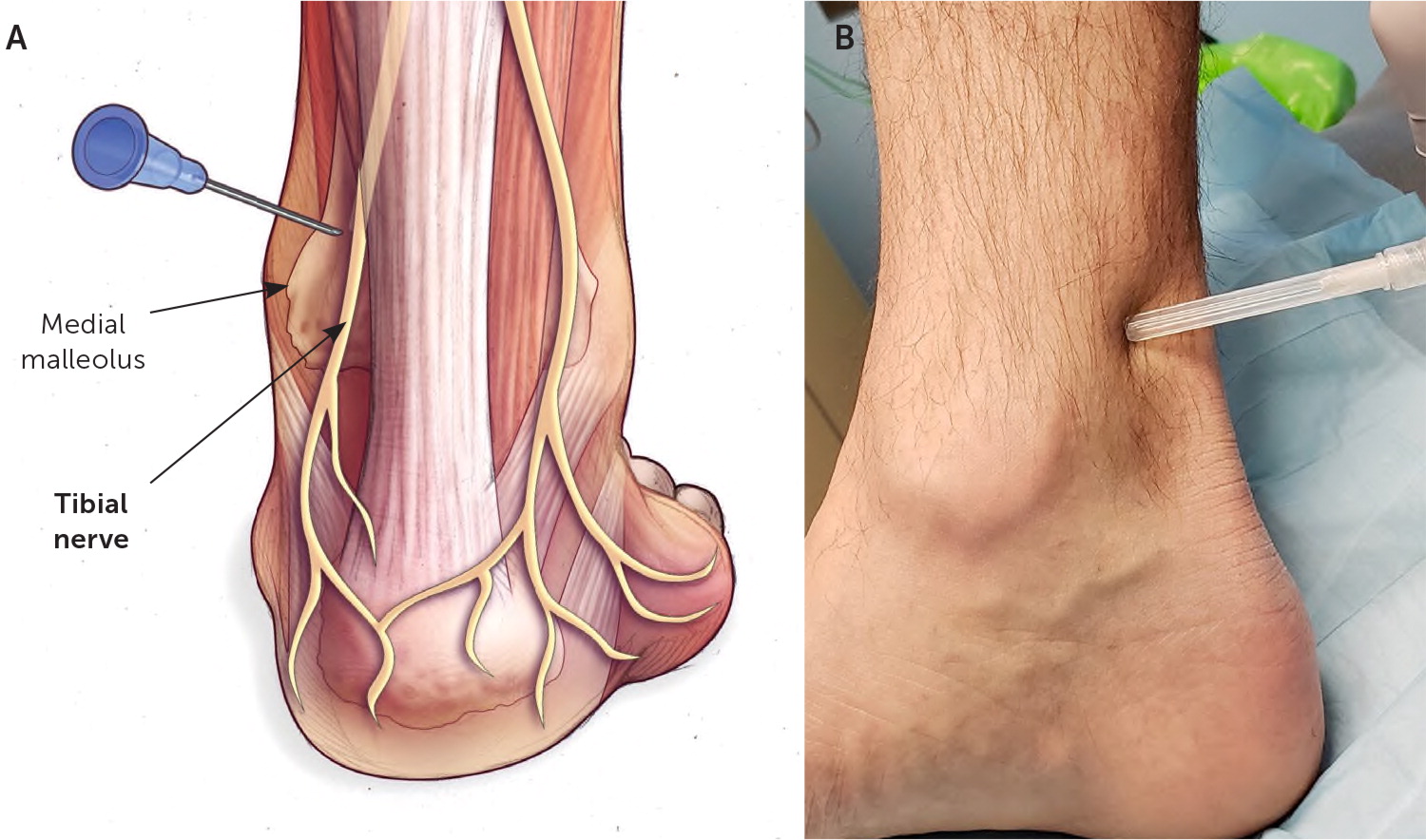
LANDMARK-GUIDED INJECTION
The patient is in the prone, supine, or lateral recumbent position on the affected side to expose the medial ankle. The needle is advanced in the subcutaneous tissue toward the posteromedial tibia at a 45-degree angle, through the retinaculum 1 to 2 cm above the medial malleolus anteromedial to the Achilles tendon. Once the needle contacts the tibia, the needle is withdrawn a few millimeters where the agent is injected (Figure 8).
Ultrasound-Guided Tibial Nerve Block
The patient is in a lateral recumbent position on the affected side to expose the medial malleolus. The transducer is placed at the level of the medial malleolus perpendicular to the Achilles tendon, and the tibial nerve is visualized posterior to the posterior tibial artery.10 The agent is injected into the perineural space by advancing a needle from posterior to anterior in plane with the transducer (Figure 9). See a video of this technique.
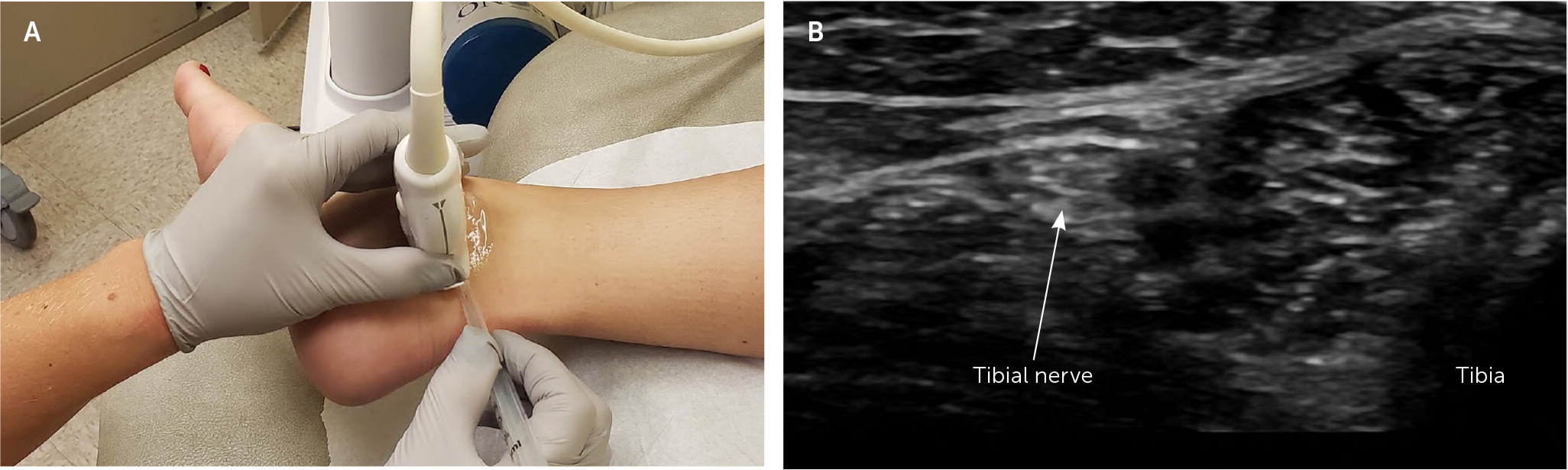
Ultrasound-Guided Tibial Nerve Block
Deep Peroneal Nerve Block (Ankle)
ANATOMY
The deep peroneal nerve originates from the common peroneal nerve and traverses to the ankle below the tibialis anterior and extensor hallucis longus muscles in the anterior compartment. It crosses the ankle below the flexor retinaculum and lateral to the anterior tibial artery terminating in the first web space11 (Figure 10). The deep peroneal nerve is made up of sensory and motor fibers from the L4-S2 nerve roots and provides sensation to the first web space.
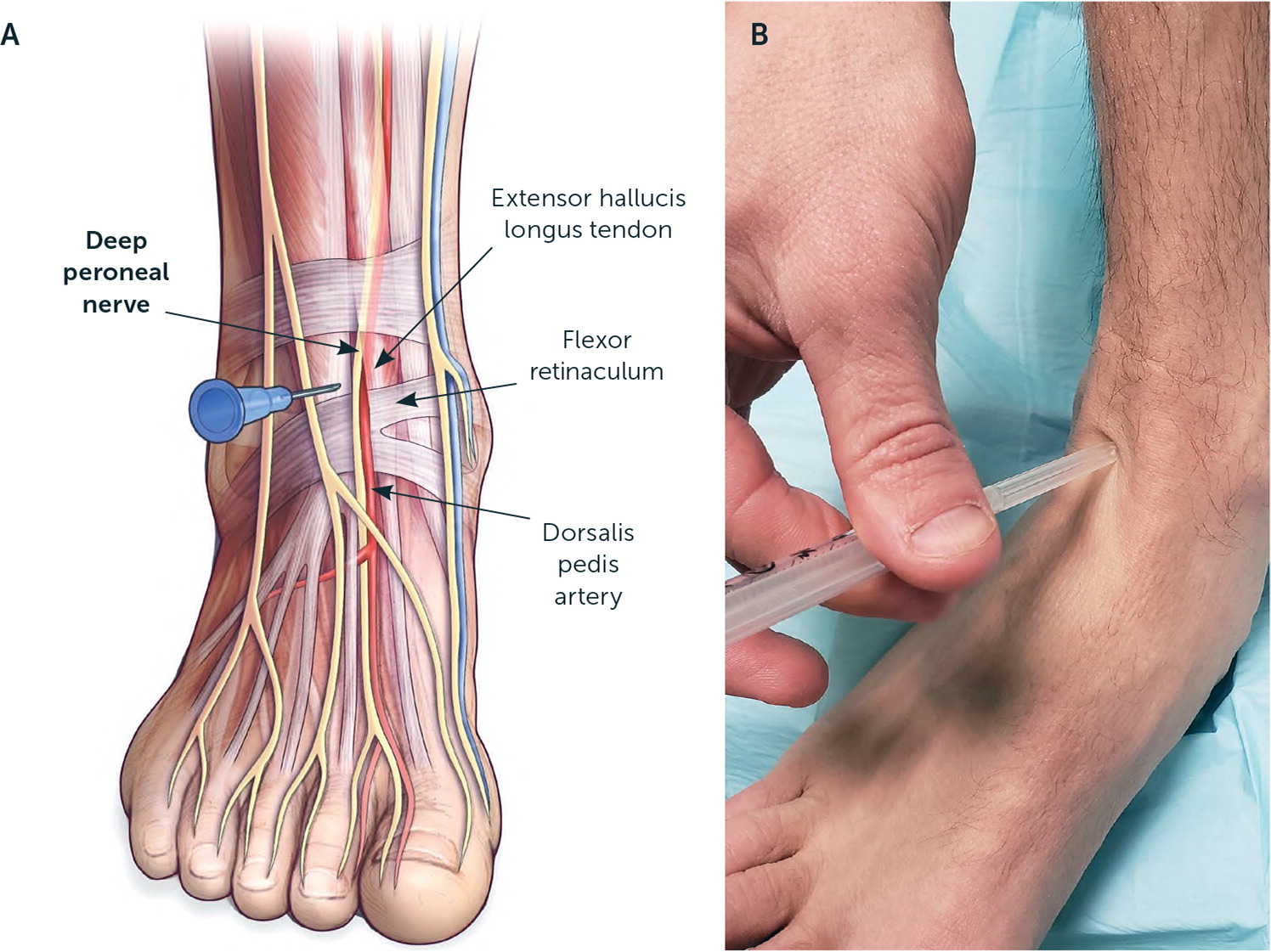
LANDMARK-GUIDED INJECTION
The patient is in a supine position with the knee flexed and the foot resting on the table. The extensor hallucis longus tendon is identified by dorsiflexing the great toe against resistance. The needle is advanced perpendicular to and toward the tibia, 0.5 cm lateral to the extensor hallucis longus tendon. Once the needle contacts the tibia, it is withdrawn a few millimeters, and the agent is injected below the extensor retinaculum (Figure 10).
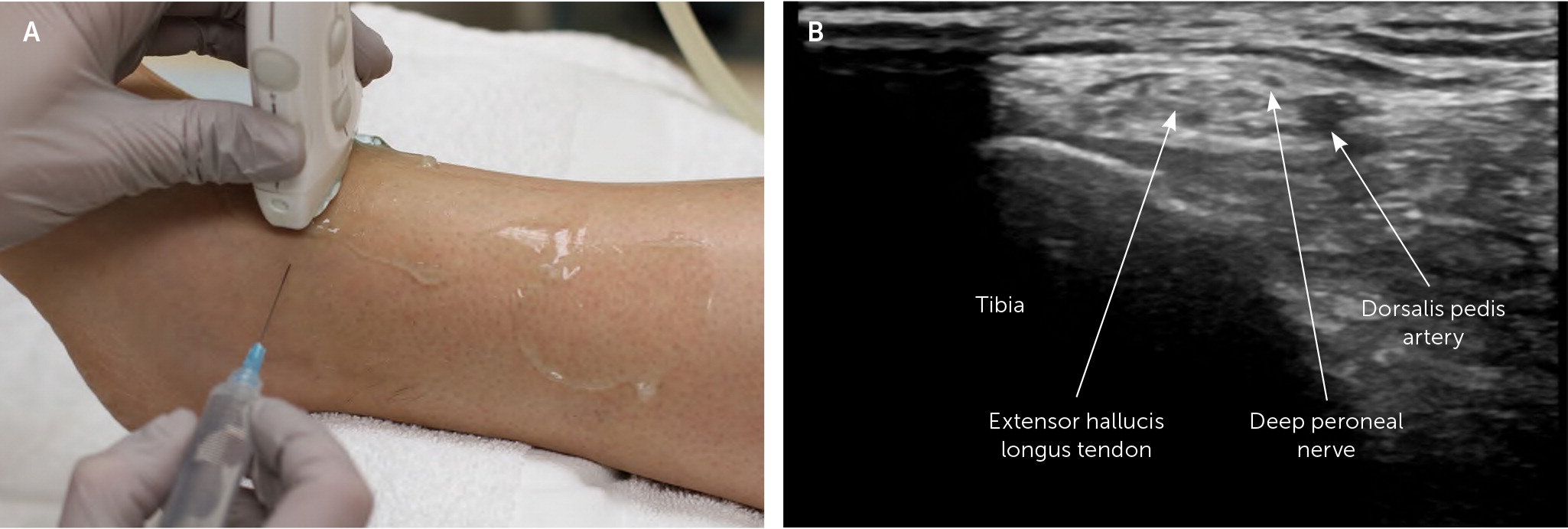
ULTRASOUND-GUIDED INJECTION
The patient is in a supine position. The transducer is placed transversely over the anterior ankle. The deep peroneal nerve is located next to the anterior tibial artery and below the superior extensor retinaculum. The agent is injected into the perineural space of the nerve by advancing the needle in plane with the transducer (Figure 11).
Superficial Peroneal Nerve Block (Ankle)
ANATOMY
The superficial peroneal nerve originates from the common peroneal nerve and traverses in the lateral compartment of the leg anterior to the peroneus longus muscle. It penetrates the crural fascia approximately 10 cm proximal to the lateral malleolus. After emerging from the lateral compartment, it runs subcutaneously to the dorsum of the foot (Figure 12). The superficial peroneal nerve is a mixed sensory and motor nerve made up of fibers from the L4-S2 nerve roots and provides sensation to the anterolateral lower leg and the dorsal foot.
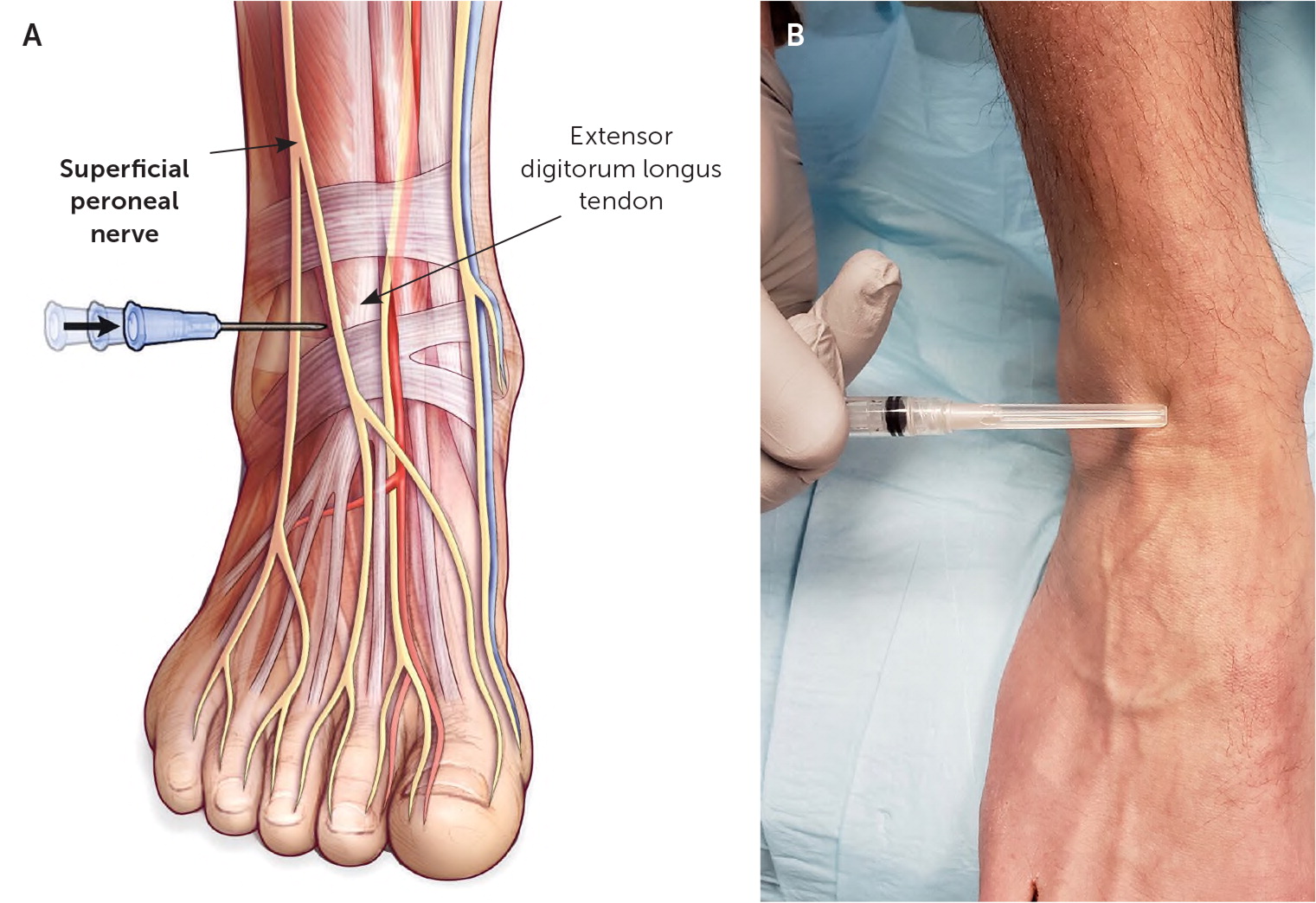
LANDMARK-GUIDED INJECTION
The patient is in a supine position with the knee flexed and the foot resting on the table. The needle is advanced in the subcutaneous space at a 10- to 15-degree angle anterior to the lateral malleolus. The agent is injected in the subcutaneous tissue from the lateral malleolus to the extensor digitorum longus (Figure 12).
ULTRASOUND-GUIDED INJECTION
The patient is in the lateral recumbent position on the unaffected side with the lateral ankle exposed. The transducer is placed perpendicular to the length of the lower leg, 3 to 4 cm proximal to the lateral malleolus. The superficial peroneal nerve is visualized where it penetrates the crural fascia just between the peroneus brevis and extensor digitorum longus muscle. The agent is injected in the perineural space of the nerve by advancing the needle in plane with the transducer (Figure 13).
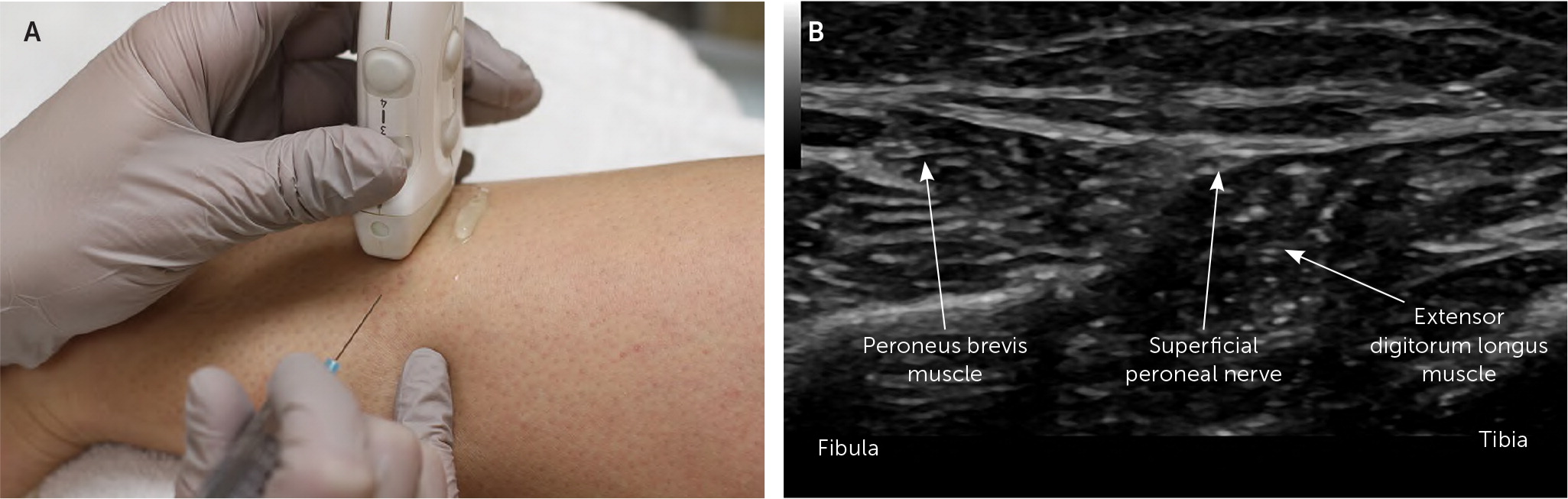
It should be noted that the location is different from that described for landmark-guided injection. The superficial peroneal nerve is larger in the area described for ultrasound-guided injection but has a variable position. The location described for landmark-guided injection is more consistent but can be challenging to identify on ultrasonography because of the small size of the nerve at this location.12
Sural Nerve Block (Ankle)
ANATOMY
The sural nerve distal to the knee traverses superficial to the gastrocnemius muscle and behind the fibula. At the ankle, it runs anterolateral to the Achilles tendon adjacent to the small saphenous vein and passes posterior to the lateral malleolus13 (Figure 14). The sural nerve is a sensory nerve with fibers from the S1–S2 nerve roots, which provides cutaneous sensation to the posterior lateral lower leg, lateral ankle, and the lateral aspect of the heel and foot.
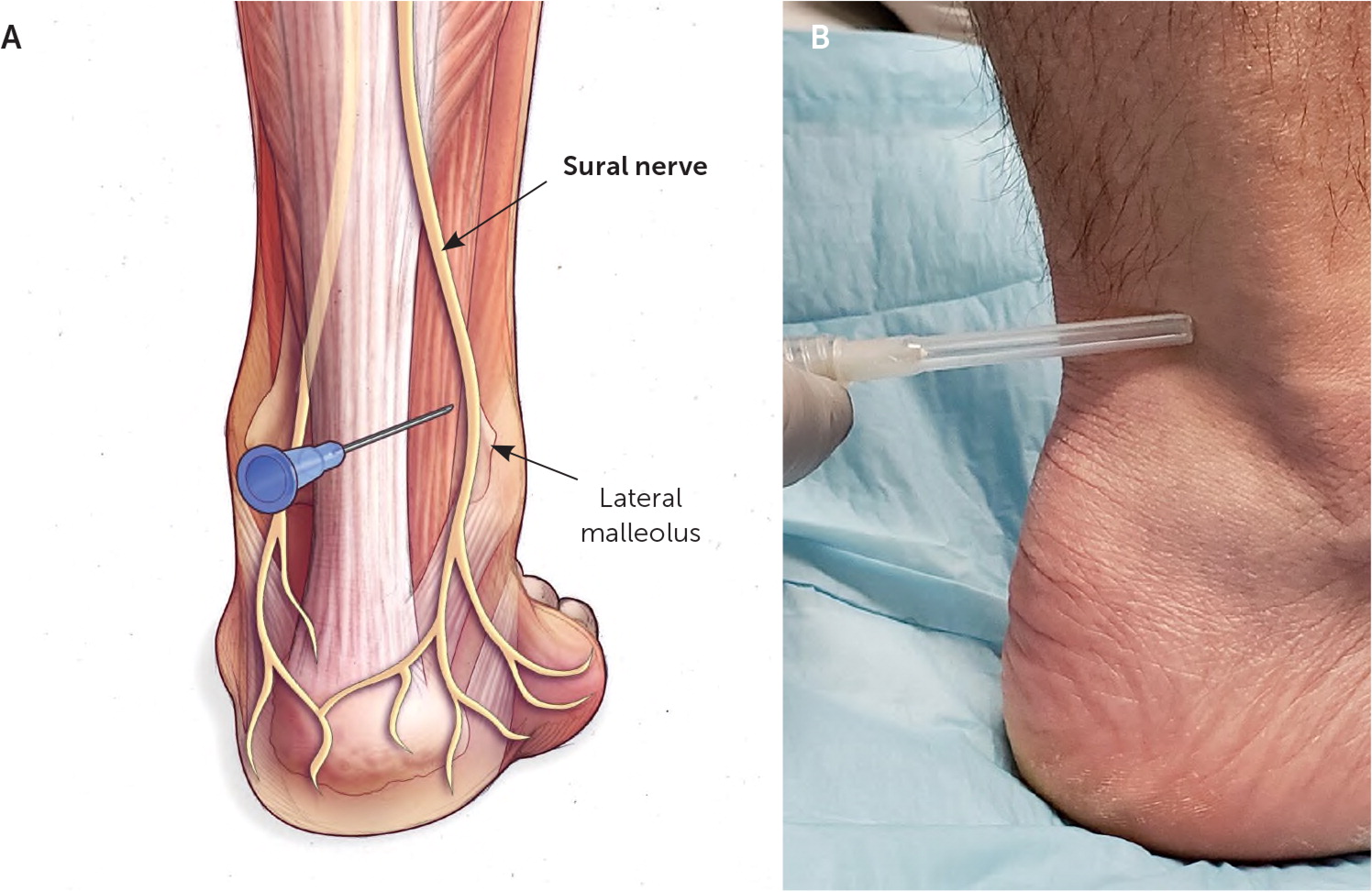
LANDMARK-GUIDED INJECTION
The patient is supine with the foot resting flat in a neutral position on the table. The needle is advanced lateral and perpendicular to the long axis of the Achilles tendon, 1 to 2 cm above the distal tip of the lateral malleolus. Once the needle contacts the posterior fibula, it is withdrawn a few millimeters so that it is just off the bone, and the agent is injected in a track between the fibula and Achilles tendon (Figure 14).
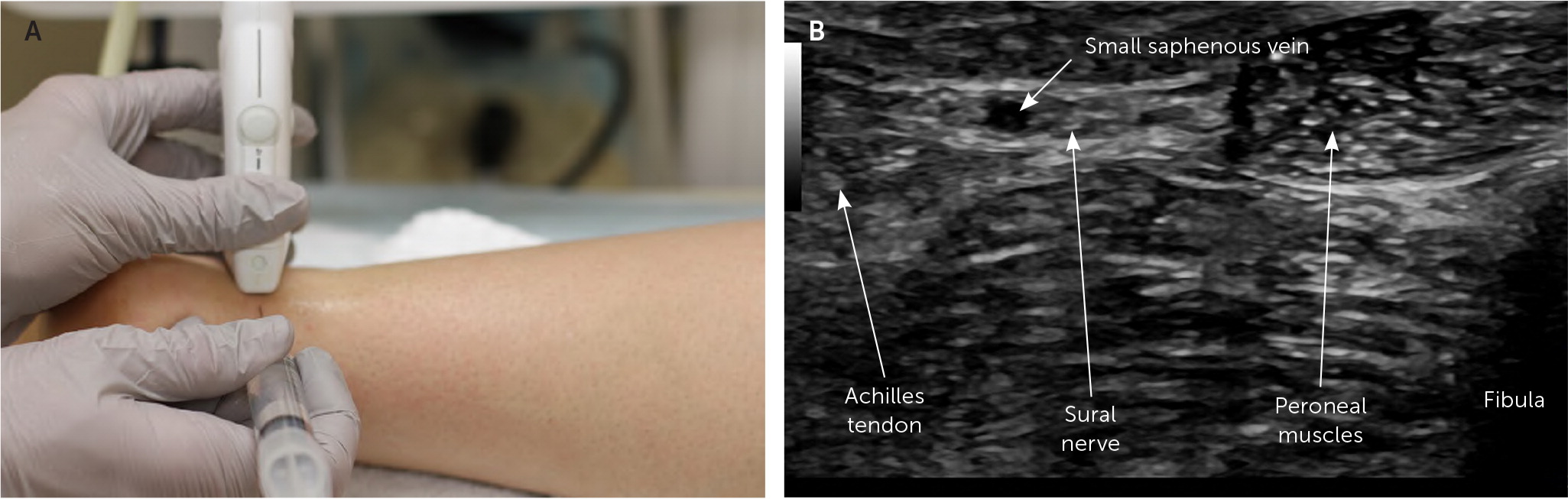
ULTRASOUND-GUIDED INJECTION
The patient is in a lateral recumbent position on the unaffected side to expose the lateral malleolus. The transducer is placed transversely 1 to 2 cm above the lateral malleolus and perpendicular to the Achilles tendon to visualize the sural nerve adjacent to the small saphenous vein.13 The agent is injected in the perineural space by advancing the needle from the Achilles tendon toward the lateral malleolus in plane with the transducer (Figure 15).
Data Sources: A PubMed search was completed in Clinical Queries using the key terms peripheral, nerve, and block. The search included meta-analyses, randomized controlled trials, systematic reviews, and evidence-based guidelines. Also searched were the Agency for Healthcare Research and Quality Effective Healthcare reports, U.S. Preventive Services Task Force guidelines, the Cochrane database, and Essential Evidence Plus. Search dates: November 26, 2018, to June 25, 2019; and February 19, 2020.
The views expressed in this publication are those of the authors and do not reflect the official policy or position of the Departments of the Army or Air Force, the Department of Defense, or the U.S. government.
