
Am Fam Physician. 2020;101(11):654-664
This is part I of a two-part article on nerve blocks. “Part II, Lower Extremity,” appears in this issue of AFP.
Author disclosure: No relevant financial affiliations.
Procedural anesthesia is administered by family physicians for a variety of conditions, including neuropathies, fracture reduction, foreign body removals, and complex wound management. A nerve block may be preferred because it provides effective regional anesthesia with less anesthetic. Nerve blocks require a thorough understanding of relevant anatomy, aiding the physician in optimizing the anesthesia effect while minimizing complications. Nerve blocks can be guided by bony landmarks, peripheral nerve stimulation, or ultrasonography. Ultrasound-guided nerve blocks are superior in decreasing procedural complications and procedure time. Physicians should be aware of these techniques to appropriately counsel their patients on procedural options. Nerve blocks of the ulnar, median, and radial nerves at the wrist and elbow provide effective anesthesia for a wide range of medical procedures in the upper extremity.
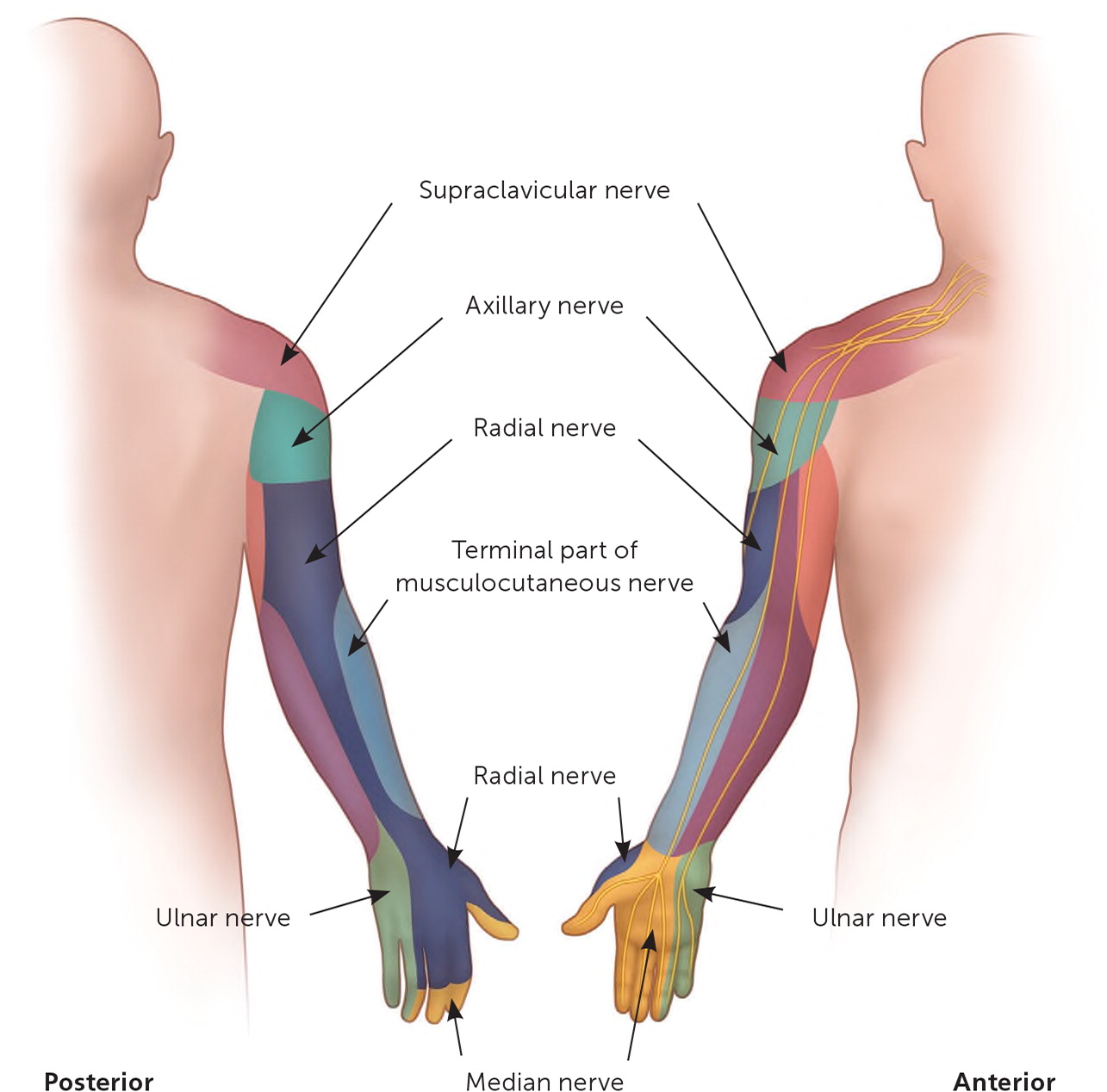
Family physicians use anesthesia via local, field, and nerve blocks to perform outpatient procedures. Local anesthesia is provided by infiltrating the anesthetic into the procedural field, whereas field blocks are performed by infiltrating the anesthetic around the procedural area leaving the procedural field undisturbed. A nerve block provides anesthesia to specific, innervated regions distal to the block. A nerve block may be preferred because it provides effective regional anesthesia with less anesthetic. Figure 1 illustrates cutaneous innervation of the upper extremity.1 This article, part I of a two-part series, discusses landmark and ultrasound-guided nerve blocks of the elbow and wrist. Part II, in this issue of American Family Physician, focuses on landmark and ultrasound-guided nerve blocks of the lower extremity.2
| Clinical recommendation | Evidence rating | Comments |
|---|---|---|
| For improved outcomes and fewer complications, nerve blocks should be performed under ultrasound guidance.3–5 | B | Consistent evidence from systematic reviews show ultrasound-guided nerve blocks are more effective with fewer complications compared with peripheral nerve stimulation guidance alone or with an anatomic landmark technique |
| Chlorhexidine should be used as a preoperative skin preparation before intact skin procedures.10 | B | Comprehensive Cochrane review illustrates lower rates of surgical site infections compared with povidone-iodine paint |
| Lidocaine should be augmented with epinephrine to prolong the duration of anesthesia and reduce the risk of bleeding during procedures.21 | B | Cochrane review of four low-quality randomized controlled trials |
Nerve blocks are used when managing neuropathies, fracture reduction, foreign body removals, and complex wounds. Table 1 lists conditions that warrant consideration for upper extremity nerve blocks. Additionally, a nerve block can be a diagnostic aid by helping to determine the source of a patient's pain. For instance, pain relief after an ulnar nerve block at the elbow confirms that the pain originates from the structures innervated by the ulnar nerve at or distal to the site of the nerve block, thus narrowing the differential diagnosis. Nerve blocks provide analgesia by blocking or inhibiting pain sensation via the perineural injection of anesthetics, allowing the patient to remain awake during invasive procedures that might otherwise necessitate centrally acting medications.
| Nerve | Elbow | Wrist |
|---|---|---|
| Median | Pronator teres syndrome | Carpal tunnel syndrome |
| Radial | Radial tunnel syndrome | Procedures of the dorsum of the hand |
| Ulnar | Cubital tunnel syndrome | Volar procedures of the little finger and ulnar half of the ring finger |
Nerve blocks require a thorough understanding of anatomy and the requisite training in the preferred technique to avoid complications, such as local anesthetic system toxicity. Nerve blocks can be guided by bony landmarks, peripheral nerve stimulation, or ultrasonography.
Peripheral nerve stimulation–guided blocks are anatomically based, with further localization using a specialized needle placed near the intended nerve. An electric stimulator sends a current from the needle to the desired distribution of the nerve, eliciting a muscle twitch to confirm correct localization. The same needle is then used to inject the anesthetic solution. A Cochrane review found moderate-quality evidence that ultrasound-guided blocks are superior to other techniques by providing sufficient and adequate anesthesia with a reduction in complications and procedure time.3 A systematic review and meta-analysis of randomized controlled trials demonstrated that compared with peripheral nerve stimulation guidance, ultrasound guidance reduces nerve block failures, neurovascular trauma, the time required for the procedure, and the time to onset of anesthesia while increasing the duration of adequate anesthesia.4 One study showed that ultrasound guidance reduces the local anesthetic dose by 30% compared with peripheral nerve stimulation guidance.5 Anatomic variation must always be considered, and the use of ultrasound guidance allows direct visualization not possible with landmark-based injections.
Ultrasound-Guided Technique
Procedure Setup
A standardized office protocol must be established for procedure setup, infection control, safety measures, and informed consent documentation.6 Patients should be counseled on the expected motor and sensory effects based on the known innervation of a target nerve and the expected duration of the recommended nerve block. Patients should be monitored for symptoms of toxicity, which include lightheadedness, tinnitus, metallic taste, visual disturbance, oral numbness, agitation, blood pressure and pulse changes, arrhythmias, and cardiac arrest.7,8
Equipment setup and patient positioning depend on the anatomic area involved and procedure choice. Ultrasound-guided procedures are best performed with patient positioning that allows for direct alignment of the injection site with the physician's line of sight to the ultrasound screen (Figure 2). A high-frequency linear array ultrasound transducer (i.e., a probe that has a frequency range of 5 to 12 MHz) is well suited for the superficial nerve blocks discussed in this article.

The use of sterile gloves is not superior to the use of nonsterile gloves when establishing a clean procedural area.9 A 2015 Cochrane review demonstrated lower rates of surgical site infections from intact skin procedures with a 0.5% chlorhexidine skin preparation compared with povidone-iodine paint.10 The American Institute of Ultrasound in Medicine provides guidelines for establishing office protocols for cleaning of ultrasound probes and the use of sterile vs. nonsterile ultrasound gel, as well as training resources.11
A 25- to 27-gauge, 1.5-inch needle is recommended, although some patients may require longer needles because of a larger body habitus, which will be readily apparent on ultrasonography. Ultrasound-guided nerve blocks can be administered using an in-plane or an out-of-plane injection method. With the in-plane (parallel) method, the transducer and needle are in the same plane, and the length of the needle is advanced in a visible field of view toward the target (Figure 3). With the out-of-plane (perpendicular) method, the needle passes through the visible plane of the transducer 12 (Figure 4). The choice of method depends on physician preference and the anatomic area.
The anesthetic is chosen based on the expected duration of the procedure, distribution, and location of the intended effect.13–20 For example, a shorter-lasting anesthetic such as lidocaine may be selected because of its faster onset of action and a shorter procedure time, whereas the longer-lasting ropivacaine (Naropin) may be chosen for a longer procedure, bearing in mind that its onset of action will be slower. Local anesthetics can also be combined to take advantage of their different properties. Table 2 lists the characteristics of common anesthetics.8,13–21
| Agent | Drug class | Concentration (%)* | Onset | Duration | Maximum dose (mg per kg) |
|---|---|---|---|---|---|
| Lidocaine | Amide | 1, 2, 4 | Rapid | 30 to 60 minutes | 4 |
| Mepivacaine | Amide | 1 | Moderate | 45 to 90 minutes | 4 |
| Bupivacaine (Marcaine) | Amide | 0.25 to 0.5 | Slow | 2 to 4 hours | 3 |
| Ropivacaine (Naropin) | Amide | 0.2 to 1.0 | Moderate | 6 to 14 hours | 2.5 (for 0.5%) |
| Tetracaine (Pontocaine) | Ester | 0.25 | Slow | 2 to 3 hours | 1.5 |
| Chloroprocaine (Nesacaine) | Ester | 1 to 2 | Slow | 30 to 60 minutes | 6 |
Beyond the anesthetic agents used in nerve blocks, various adjuvant therapies are available. Adjuvants may be beneficial in lengthening the duration of anesthesia, decreasing procedural bleeding, and reducing postoperative pain. A 2015 Cochrane review demonstrated that lidocaine augmented with epinephrine may prolong the duration of anesthesia and reduce bleeding during the procedure.21 A 2017 Cochrane review concluded that dexamethasone may prolong the duration of sensory blocks and is effective in reducing postoperative pain intensity and opioid consumption in upper extremity procedures. There was not enough evidence to determine the benefits of dexamethasone in lower extremity procedures.22
The volume of the injected agent varies by location and approach. Landmark-based injections commonly require 5 to 10 mL to bathe and anesthetize the nerve, whereas an ultrasound-guided injection usually requires only 2 to 5 mL.
Potential risks of a nerve block include soft tissue and neurovascular injury and vascular injection of the agent. A common practice to avoid inadvertent vascular injection is to aspirate before injection and reorient the needle out of the blood vessel if any blood is aspirated. Ultrasound guidance greatly reduces inadvertent vascular injection.
Median Nerve Block
ANATOMY
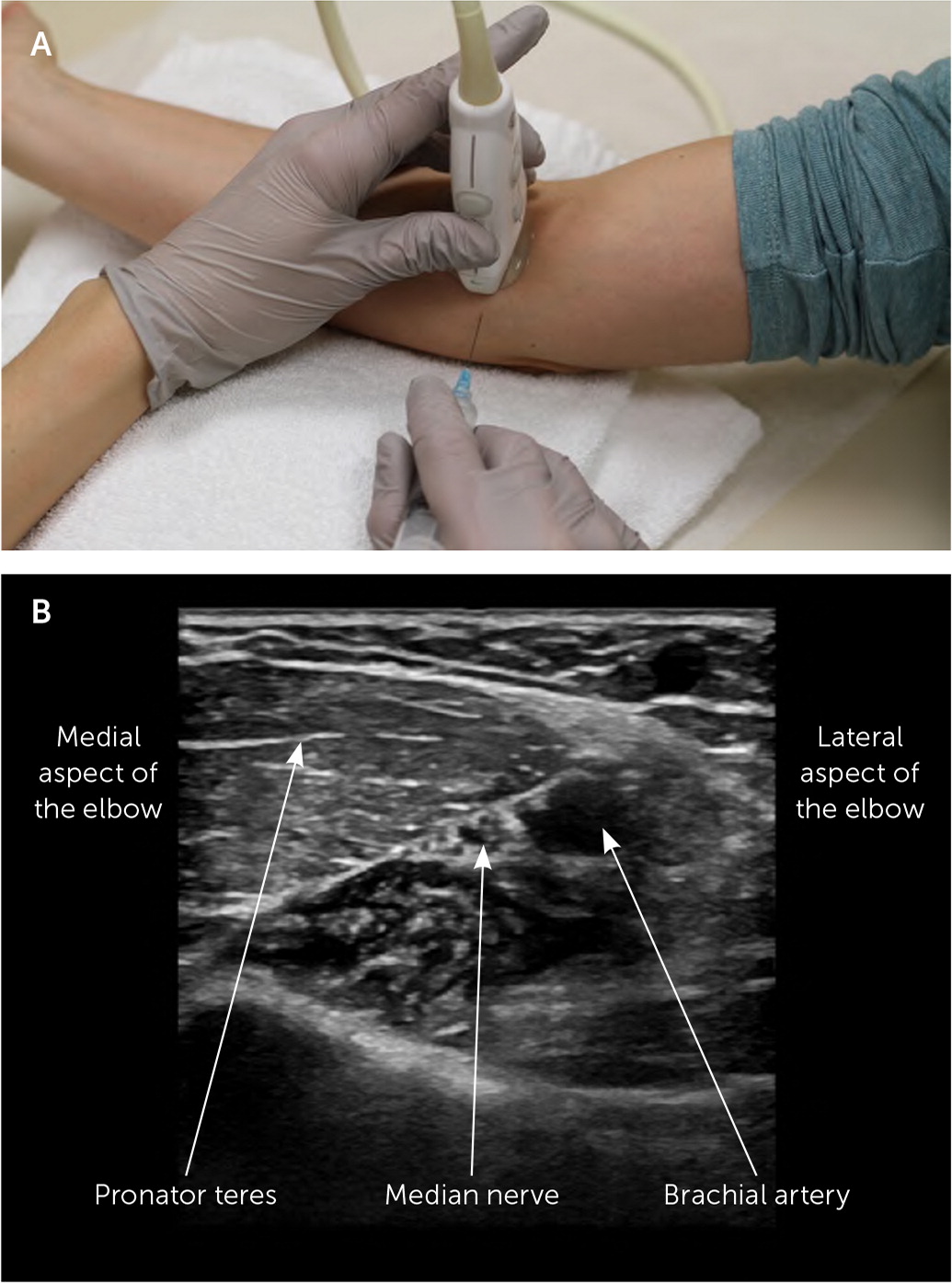
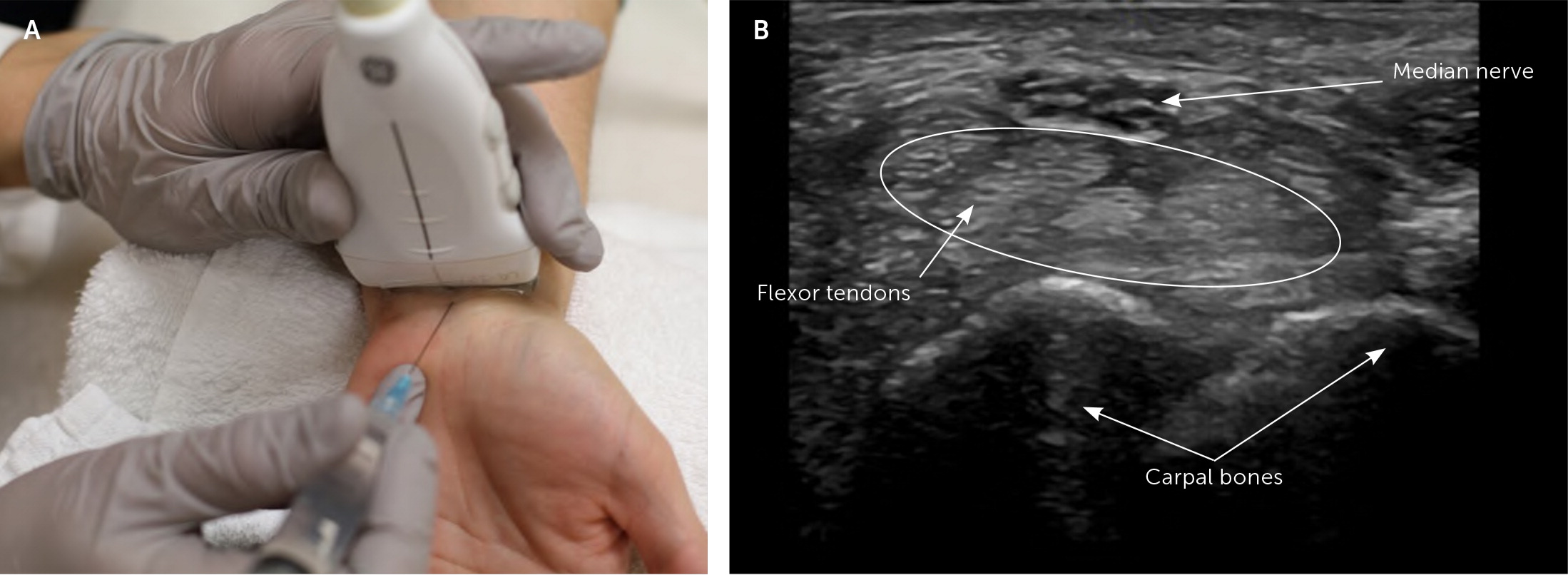
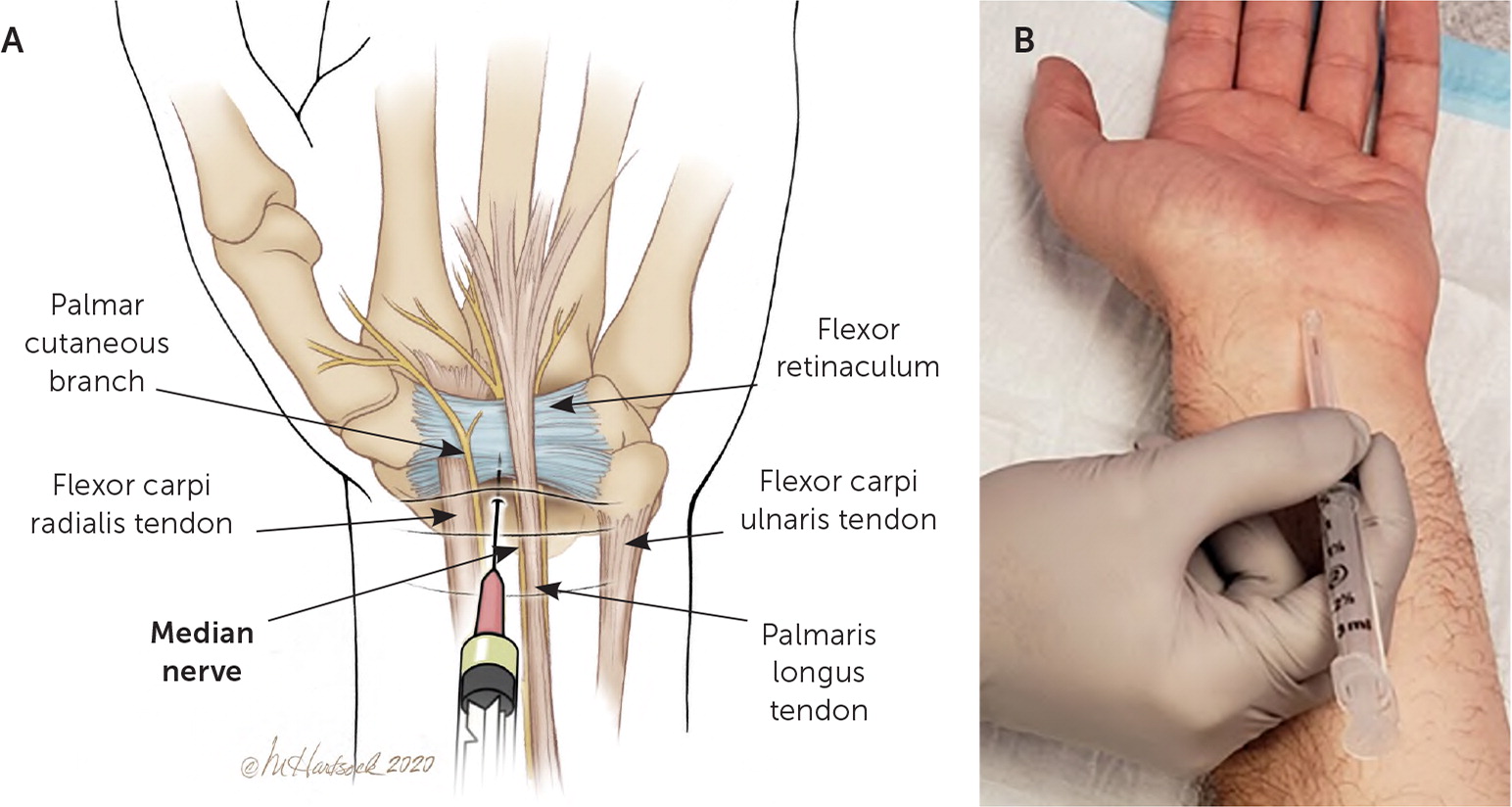
The median nerve enters the cubital fossa just medial to the brachial artery between the two heads of the pronator teres and traverses distally between the flexor digitorum superficialis and flexor digitorum profundus muscles.23 At the wrist, the median nerve is between the flexor carpi radialis and palmaris longus tendons.
The median nerve is a mixed sensory and motor nerve formed from the fibers of C5-T1 nerve roots. Its sensory distribution is depicted in Figure 11 and is generally from the palmar, or volar, aspect of the thumb to the radial aspect of the ring finger, and on the dorsal side includes the tip of the index finger, middle finger, and radial aspect of the ring finger. The anatomy of the median nerve is illustrated in Figure 5 and Figure 6.24
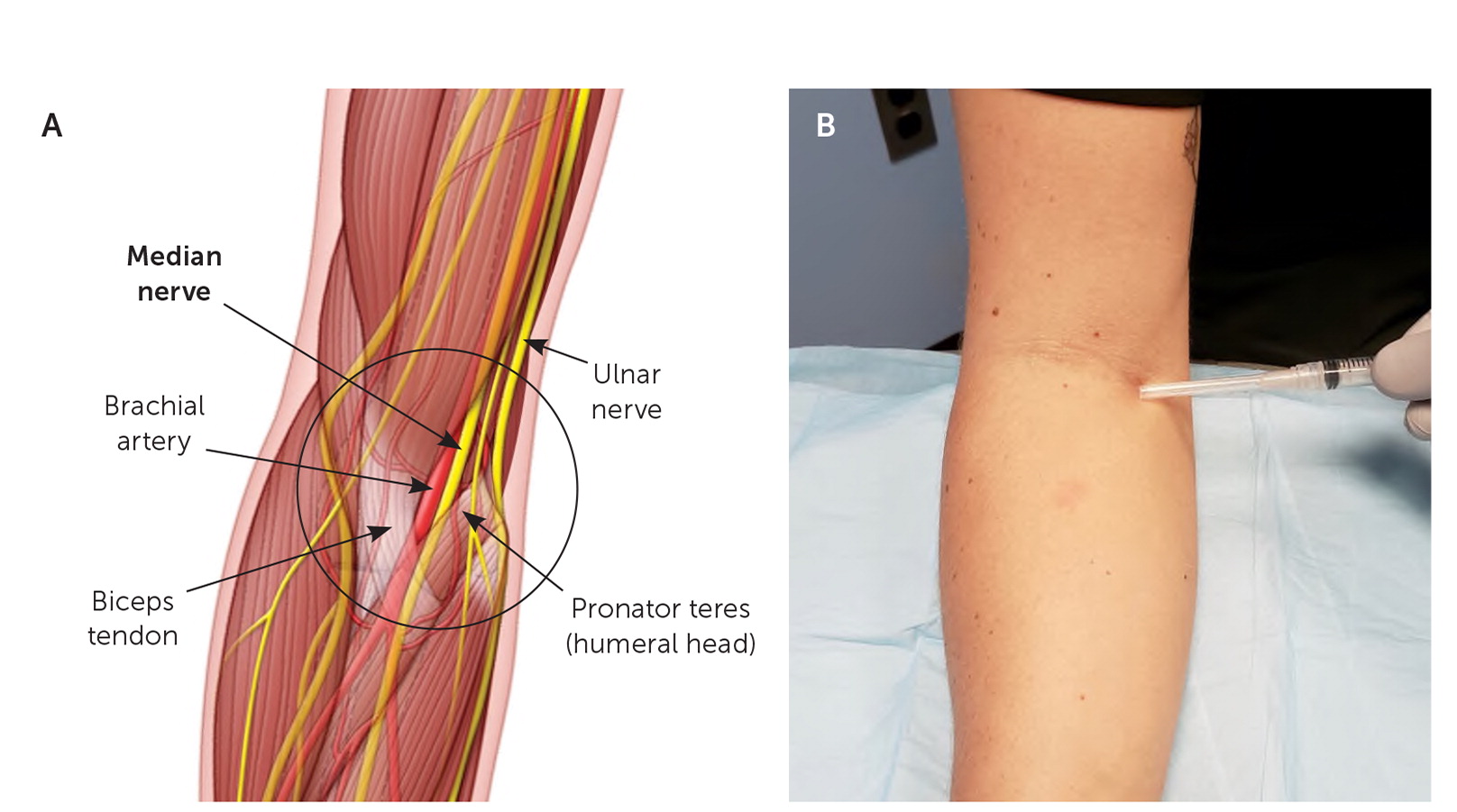
LANDMARK-GUIDED INJECTION
The patient's forearm is placed in a supinated position, and the needle is advanced at a 30-degree angle (Figure 5). The agent is injected approximately 1 cm medial to the palpable brachial artery within the antecubital crease. At the wrist, the patient's forearm is placed in a supinated position, and the needle is advanced at the wrist crease between the palmaris longus and the flexor carpi radialis tendons, aimed distally at a 45-degree angle (Figure 624). If the palmaris longus tendon is absent, which is the case in 15% of the population, the needle is inserted at the palmar crease 1 cm medial to the flexor carpi radialis tendon.25 As the needle is advanced through the flexor retinaculum, there will be a decrease in resistance where the agent is injected.
ULTRASOUND-GUIDED INJECTION
The patient is seated, and the forearm is placed in a supinated position with the elbow extended. The transducer is placed transversely to the length of the forearm in the cubital fossa to visualize the median nerve next to the vascular structures (Figure 3). Real-time visualization of pulsating arteries and compressible veins allows for distinction under ultrasound guidance. When the nerve is visualized on ultrasonography in short axis, the nerve has a characteristic honeycomb pattern, which is a result of hypoechoic nerve fibers embedded in a hyperechoic background of connective tissue.12,26 Advancing the needle medial to lateral, in plane with the transducer, the agent is injected in the perineural space of the median nerve.
An ultrasound-guided median nerve block at the wrist begins with the patient seated and the forearm in a supinated position. The transducer is placed transversely to the length of the forearm at the wrist crease (Figure 4), which is at the level of the proximal carpal bones in the carpal tunnel. The median nerve can be differentiated from the flexor tendons by its relative honeycomb appearance and minimally affected by loss of echogenicity (anisotropy) compared with nearby tendons. Additionally, if the patient actively moves the fingers while the transducer is across the wrist crease, the flexor tendons in the carpal tunnel will glide in the longitudinal plane while the median nerve slides in the carpal tunnel between the tendons. One way to perform this injection is using an out-of-plane technique, advancing the needle distal to proximal at the level of the wrist crease and injecting the agent in the perineural space of the median nerve.
Ultrasound-Guided Median Nerve Block
Radial Nerve Block
ANATOMY
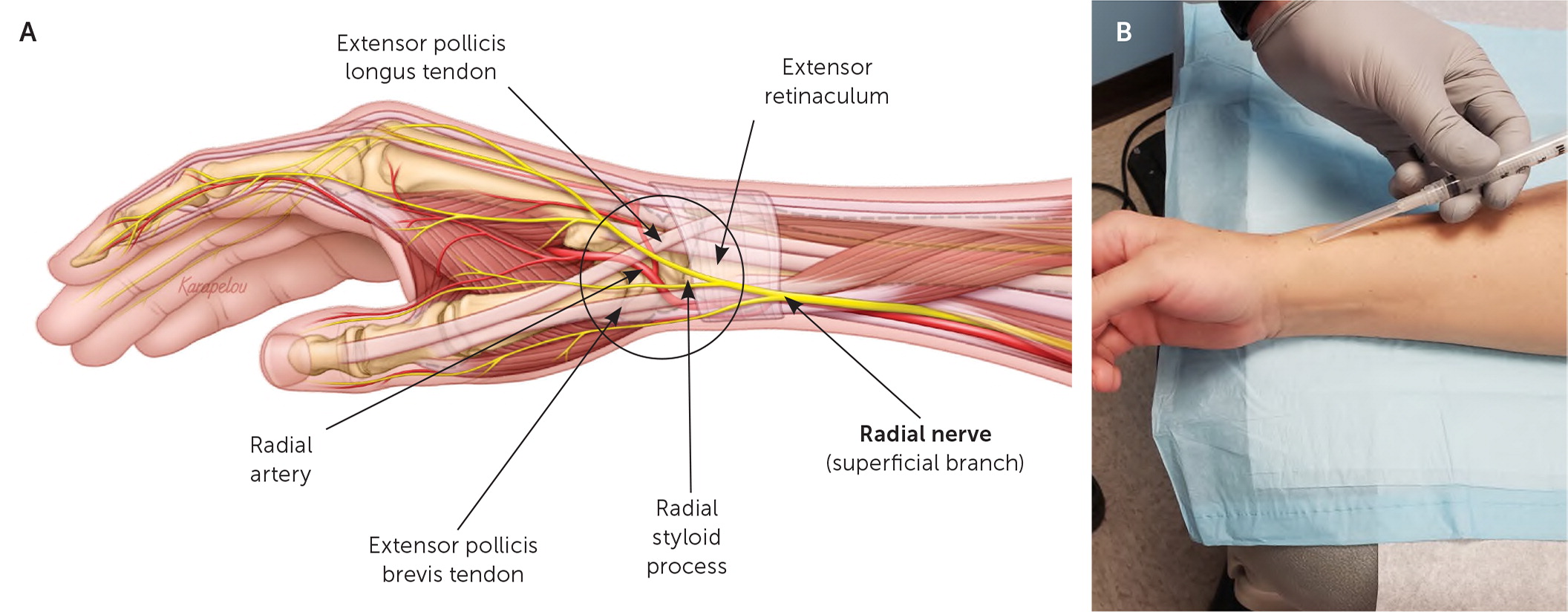
The radial nerve enters the forearm just volar to the lateral epicondyle and quickly divides into deep and superficial branches. The deep branch traverses through the two heads of the supinator muscle where it emerges as the posterior interosseous nerve. The superficial branch stays just below the brachioradialis muscle as it courses distally toward the wrist, dividing proximal to the radial styloid process into the dorsal and palmar branches. The anatomy of the radial nerve is illustrated in Figure 7 and Figure 8.
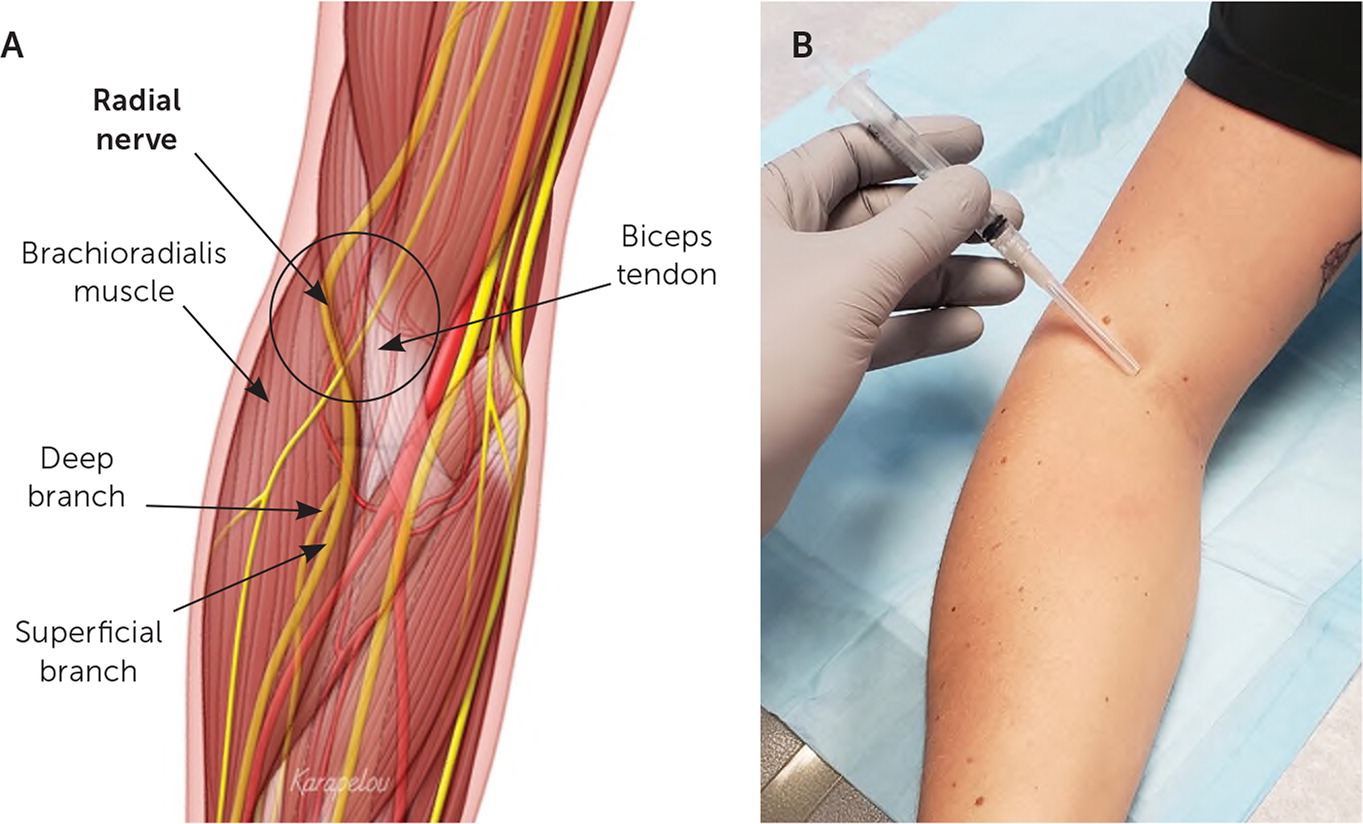
The radial nerve is a mixed motor and sensory nerve formed from the fibers of the C5-T1 nerve roots and provides sensation to the central portion of the dorsal aspect of the forearm; the dorsal aspect of the thumb, index, and middle fingers; and the radial half of the ring finger. It spares the distal dorsal surface of the index, middle, and ring fingers' nail beds, which are innervated by sensory branches of the median nerve27 (Figure 11).
LANDMARK-GUIDED INJECTION
The patient's forearm is placed in a supinated position, and the needle is inserted 1 to 2 cm proximal to the antecubital crease. It is advanced at a 45-degree angle toward the humerus between the lateral border of the biceps tendon and the brachioradialis muscle, where the agent is injected (Figure 7). At the wrist, the patient is positioned with the radial (thumb) side up and the ulnar side resting on the table. The needle is advanced into the subcutaneous tissue at a 10- to 20-degree angle, approximately 1 to 2 cm proximal and lateral to the radial styloid process (Figure 8). The agent is injected into the subcutaneous tissue.
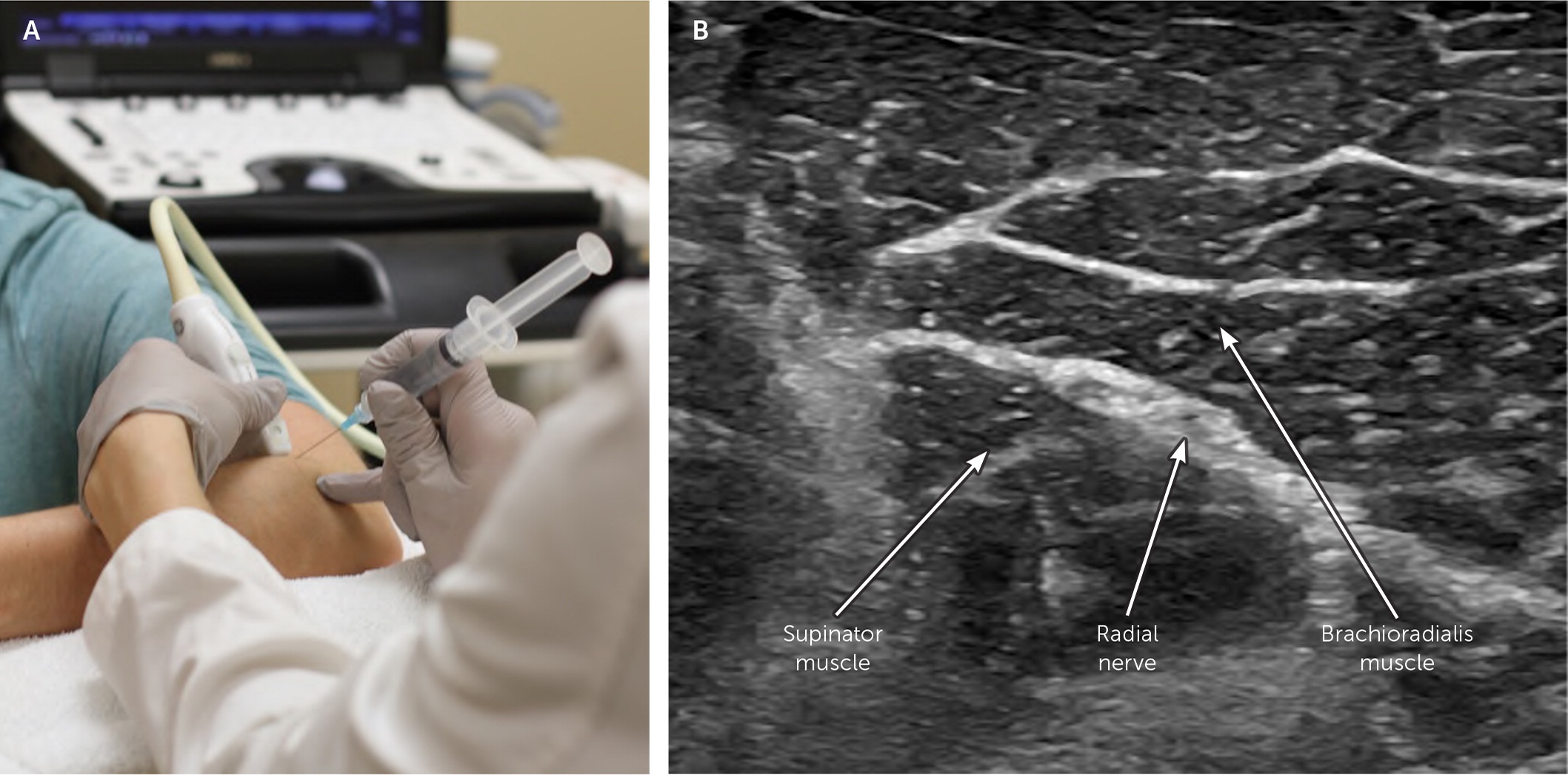
ULTRASOUND-GUIDED INJECTION
The patient is seated with the forearm pronated and elbow flexed at 90 degrees. The transducer is placed transversely to the length of the forearm over the extensor muscle mass (Figure 9). The radial nerve is visualized in the short axis 3 to 4 cm distal to the lateral epicondyle. It should be noted that there is great variability in the location of the radial nerve branching deep and superficially. The transducer may need to be moved proximally or distally to optimize visualization of the radial nerve. The agent is injected in the perineural space of the radial nerve by advancing the needle lateral to medial in plane with the transducer.
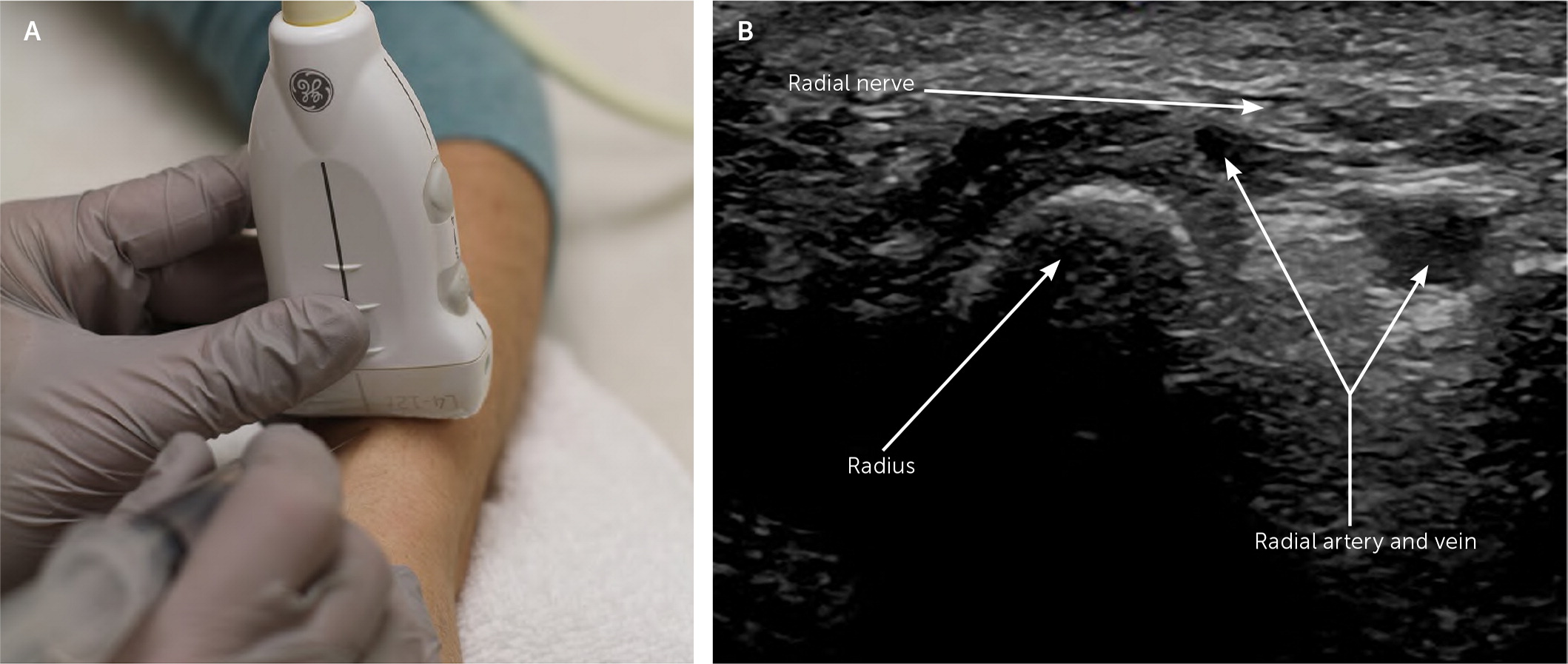
An ultrasound-guided radial nerve block at the wrist begins with the patient seated and the radial side of the wrist facing up. The transducer is placed transversely over the radius about 2 cm proximal to the radial styloid process (Figure 10). The radial nerve is visualized in the short axis proximal to the radial styloid process before the bifurcation. The radial nerve is identified, and the needle is advanced out of plane with the transducer. The agent is injected in the perineural space.
Ulnar Nerve Block
ANATOMY
The ulnar nerve enters the forearm posteriorly as it courses through the cubital tunnel. It exits the cubital tunnel and traverses distally between the flexor carpi ulnaris and flexor digitorum profundus muscles. At the wrist, the ulnar nerve enters the hand through the Guyon canal. The ulnar nerve is a mixed motor and sensory nerve formed from the fibers of the C8-T1 nerve roots and occasionally C7 nerve roots. It provides palmar and dorsal sensation to the little finger and the ulnar aspect of the ring finger 28 (Figure 11). The anatomy of the ulnar nerve is illustrated in Figure 1129 and Figure 12.30
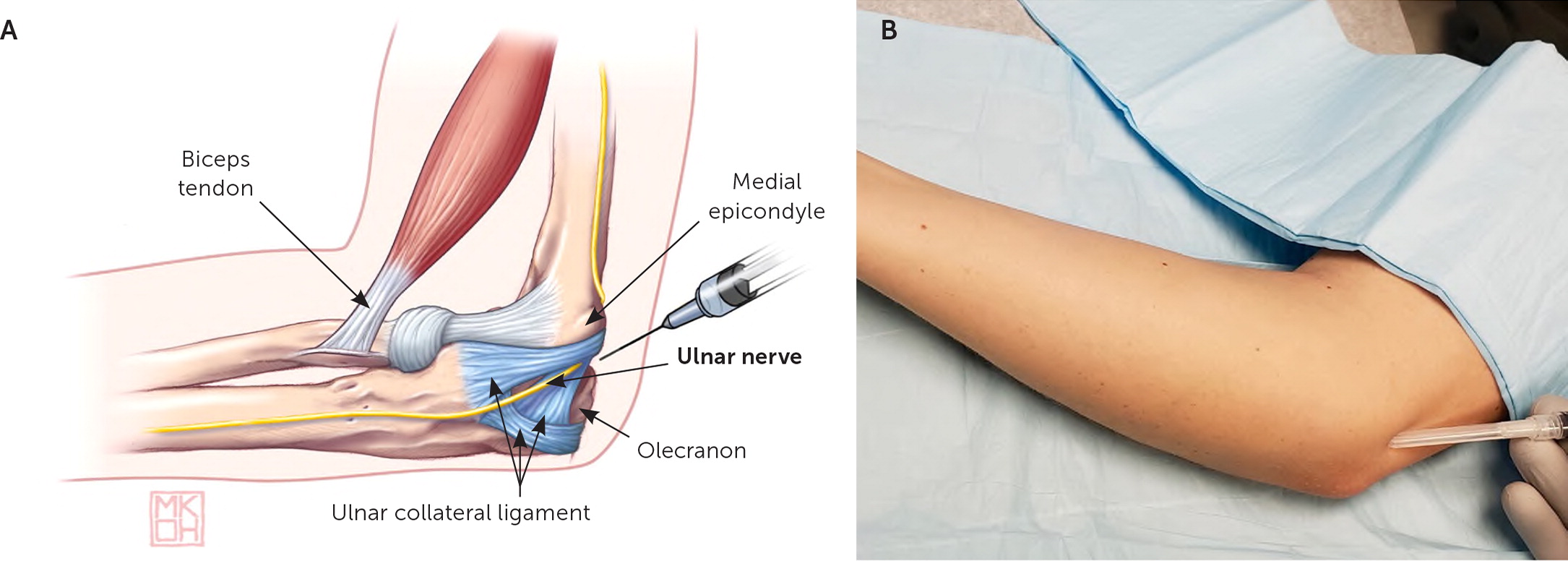
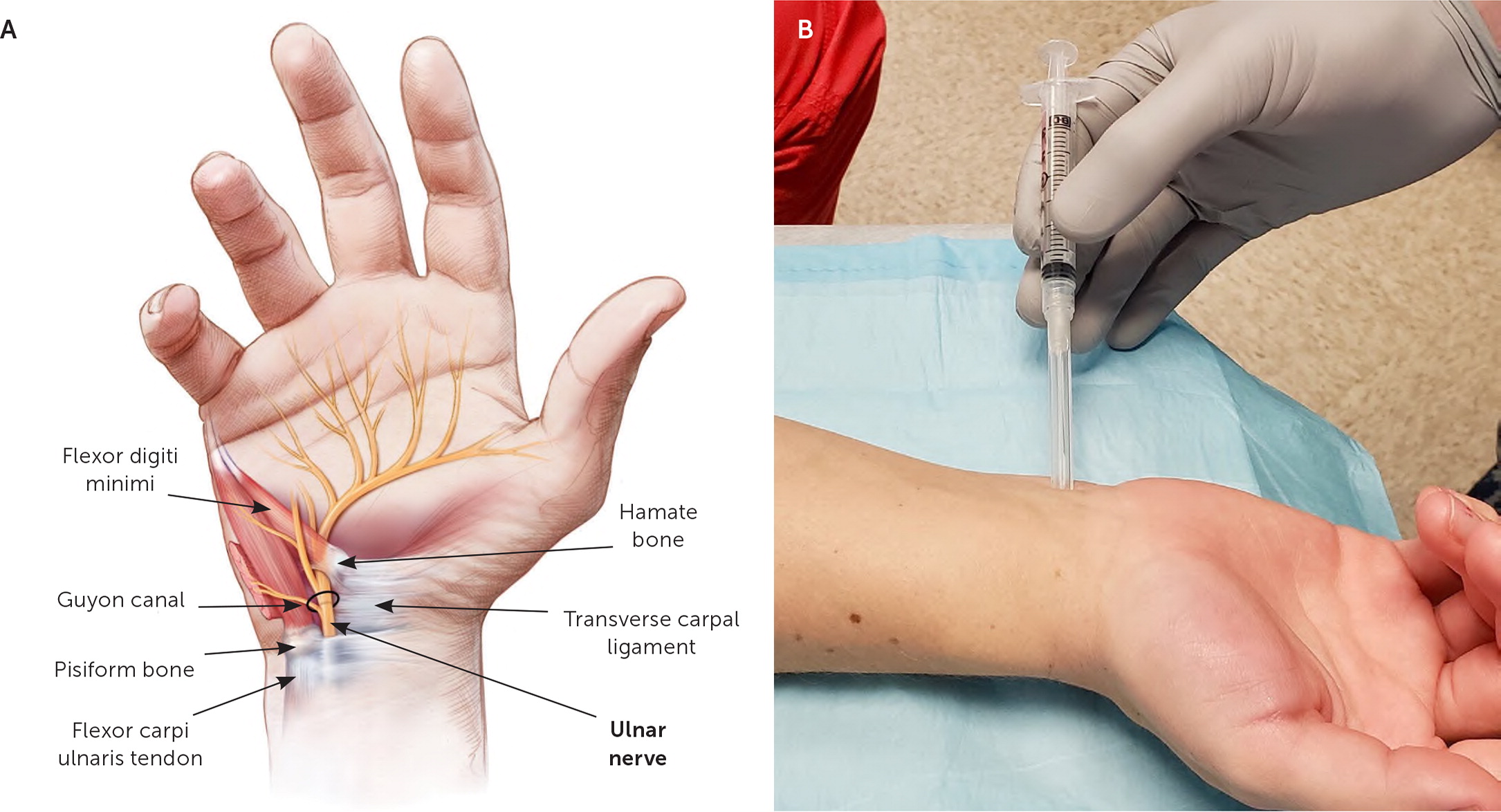
LANDMARK-GUIDED INJECTION
The patient is in a supine position with the arm resting overhead. The elbow is flexed to 90 degrees, and the forearm is supinated. The needle is advanced at a 30-degree angle approximately 0.5 cm deep, midway between the olecranon and medial epicondyle, where the agent is injected (Figure 1129). At the wrist, the forearm rests on the table with the palm up. The needle is inserted at a 45-degree angle 2 cm proximal to the medial wrist crease and radial to the flexor carpi ulnaris tendon (Figure 1230). The agent is injected in this area just proximal to the ulnar styloid process.
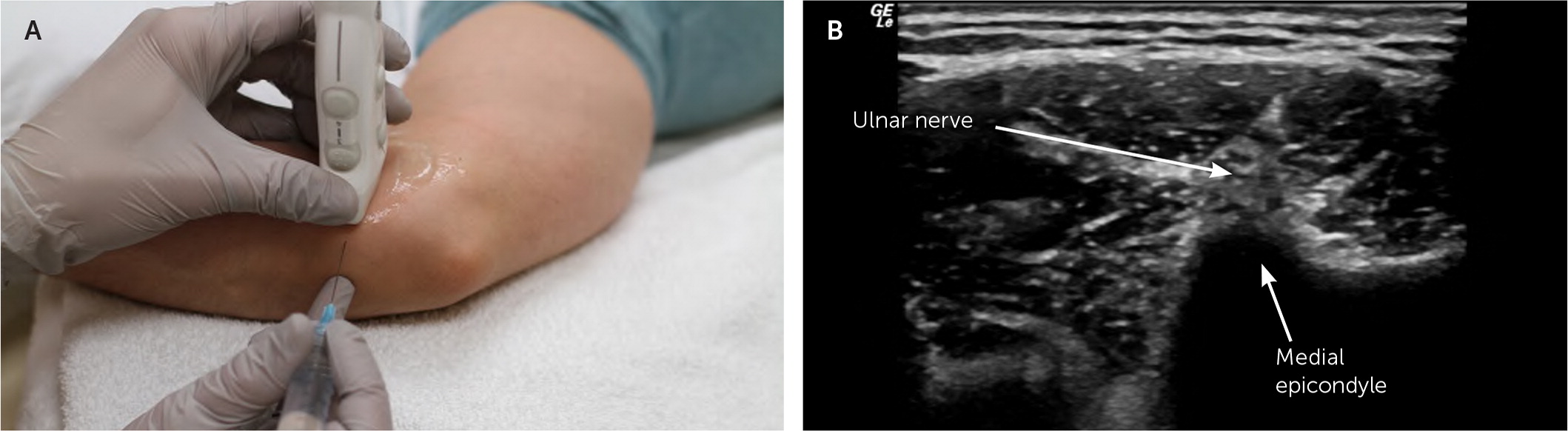
ULTRASOUND-GUIDED INJECTION
The patient is in a supine position with the arm abducted to 90 degrees, the elbow flexed to 90 degrees, and the forearm supinated. The transducer is placed transversely to the length of the forearm over the flexor mass (Figure 13). The ulnar nerve is visualized in the short axis approximately 3 to 4 cm distal to the medial epicondyle. The ulnar nerve is identified, and the needle is advanced via an in-plane approach with the transducer. The agent is injected into the perineural space.
An ultrasound-guided ulnar nerve block at the wrist begins with the patient in a seated position, with the palm up and forearm resting on the table. The transducer is placed transversely to the length of the forearm over the wrist crease (Figure 14). The ulnar artery and nerve are visualized in the short axis at the level of the pisiform bone. The ulnar nerve is identified, and the needle is advanced out of plane with the transducer. The agent is injected into the perineural space.
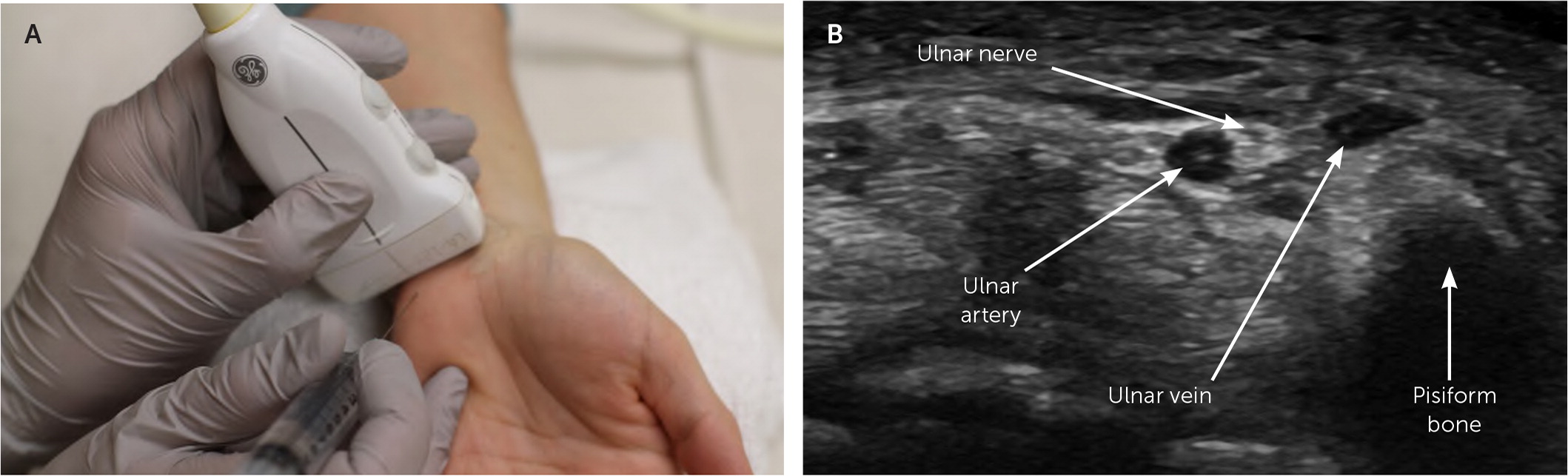
Ultrasound-Guided Ulnar Nerve Block
This article updates some aspects of a previous article on this topic by Salam.13
Data Sources: A PubMed search was completed in Clinical Queries using the key terms peripheral, nerve, and block. The search included meta-analyses, randomized controlled trials, systematic reviews, and evidence-based guidelines. Also searched were the Agency for Healthcare Research and Quality Effective Healthcare reports, U.S. Preventive Services Task Force guidelines, the Cochrane database, and Essential Evidence Plus. Search dates: November 26, 2018; March 13, 2019; and February 19, 2020.
The views expressed are those of the authors and do not reflect the official policy or position of the Departments of the Army or Air Force, the Department of Defense, or the U.S. government.
