
Am Fam Physician. 2020;101(12):740-747
Author disclosure: No relevant financial affiliations.
Foreign bodies may be introduced into the skin through lacerations and soft tissue wounds. Long-term complications of retained foreign bodies include chronic pain and neurovascular impairment. Wound exploration and initial imaging with radiography or ultrasonography should be considered before foreign body removal. Risks and benefits of removal should be discussed with the patient. Although some foreign bodies may be left in place, removal should be considered if the risk of complications is high. A cooperative patient and adequate wound visualization are important for successful foreign body removal. Adequate analgesia and judicious use of anxiolytics and sedation may be helpful. Wound irrigation with normal saline or tap water is recommended after foreign body removal. Antiseptic solutions for wound irrigation may impair healing and should be avoided. Although there is no consensus on the use of antibiotic prophylaxis, several indications exist. The patient’s tetanus immunization history should be reviewed, and vaccine should be administered if indicated.
Soft tissue wounds are common injuries. In 2016, wounds were the primary diagnosis in 6.8 million emergency department visits in the United States.1 Wounds can contain foreign bodies, which may cause long-term complications if inappropriately managed, including neurovascular deficits and chronic pain.
| Clinical recommendation | Evidence rating | Comments |
|---|---|---|
| Radiography with underpenetration and multiple views should be used to evaluate deep wounds.7 | C | Expert opinion in the absence of clinical trials |
| Ultrasonography should be used to localize radiolucent foreign bodies.8 | C | In-vitro animal study showing improved localization compared with computed tomography and plain radiography |
| Foreign body wounds should be cleaned with normal saline or tap water.18 | B | Consistent evidence from randomized controlled trials showing no difference in infection rates |
| Antiseptic solutions should not be used for cleaning foreign body wounds because they slow healing.19 | C | In-vitro studies showing cytotoxicity with several solutions |
| Antibiotic prophylaxis is not indicated for simple non-bite wounds in immunocompetent patients.36 | B | Consistent evidence from randomized controlled trials showing no benefit from treatment |
| Tetanus immunization history should be reviewed for patients who have wounds with foreign bodies.40 | C | Expert opinion and consensus guideline in the absence of clinical trials |
Evaluation and Localization
Patients may not express concern for foreign bodies after an injury. However, the patient history may suggest that further evaluation is needed. The sensation of foreign bodies and trauma secondary to high-velocity projectiles or sharp, fragile objects should increase suspicion for foreign bodies.2 Careful visual inspection is necessary to assess for the presence of foreign bodies. Palpation around wounds may reveal tenderness. Metal instruments may facilitate wound probing to avoid hand injury.
Foreign bodies may remain undetected despite wound examination. In one study, 38% of foreign bodies were missed on initial evaluation; in many cases, imaging was not obtained.3 Another study reported glass detection by radiography in 11 of 160 wounds (6.9%) that were deemed glass-free by clinicians after inspection.4 Imaging may aid detection and subsequently reduce long-term complications of retained foreign bodies (Table 1).5
| Modality | Foreign body types detected | Relative cost* | Availability† | Radiation exposure‡ | Advantages | Disadvantages |
|---|---|---|---|---|---|---|
| Computed tomography | Radiopaque (e.g., glass, metal) | $$ | ++ | High | Three-dimensional, quick, detects objects near bone | High radiation exposure |
| Fluoroscopy | Radiopaque | $ | + | Low | Real-time images, portable | Limited number of trained physicians |
| Magnetic resonance imaging | Radiolucent (e.g., wood, vegetation) | $$$ | + | None | Can be used for chronic or complex foreign bodies | Dangerous if metal is present, time consuming |
| Radiography | Radiopaque | $ | +++ | Low | Easy to interpret, quick | May not detect vegetative foreign bodies or objects behind or in bone |
| Ultrasonography | Radiolucent | $ | +++ | None | Real-time images, portable | Operator dependent |
Plain radiography is inexpensive and widely available, and it requires little exposure to radiation. It can detect radiopaque materials, including metal and glass (Figure 1). Vegetative materials (e.g., wood) cannot be seen because they absorb bodily fluids and become as dense as surrounding tissue.6 Underpenetrated radiography with multiple views, including oblique and tangential views, may reveal objects obscured by bone in other views.7 Besides direct visualization, signs of foreign bodies include surrounding air, radiolucent filling defects, and reactive bony changes.8

Ultrasonography is inexpensive and provides real-time visualization without radiation exposure. However, the quality of images is operator dependent. Ultrasonography can detect radiolucent materials (e.g., wood, vegetation) better than radiography and computed tomography.8,9 Hyperechoic areas of soft tissue injury or inflammation may suggest foreign bodies.8 Ultrasonography may facilitate targeted removal, thereby decreasing tissue destruction and subsequent patient discomfort.10
Computed tomography is typically not used for initial evaluation because of radiation exposure, low sensitivity for detecting radiolucent material, and cost.11 However, it may be helpful to visualize objects not visible on radiography, such as those obscured by bone. Computed tomography may also be used to evaluate suspected complications from retained foreign bodies and for preoperative preparation for foreign body excision8 (Figure 2).

Magnetic resonance imaging has limited utility in evaluation: it is expensive and time-consuming, and it has limited availability. It may be used to detect small foreign bodies through soft tissue contrast6 or to characterize complex and chronic foreign bodies.12 This modality should be avoided if metallic foreign bodies are suspected because these objects can shift and dislodge, causing neurovascular damage.
Fluoroscopy detects radiopaque objects, similar to radiography. Advantages include portability, low radiation exposure, and the ability to perform real-time imaging and precise approaches during foreign body removal.13 However, availability is limited, as are clinicians experienced in performing fluoroscopy.
Indications for Foreign Body Removal
Before foreign bodies are removed, informed consent discussions should be undertaken with patients. Risks include additional tissue injury, incomplete removal, and indications for additional procedures. Benefits include decreased risk of inflammatory reactions, decreased chronic pain, and faster healing. No data suggest decreased infection incidence with foreign body removal.
| Indications Close proximity to a fracture or open joint Cosmetic deformity Foreign body in the skin Highly reactive material Neurovascular or mechanical compromise Pain or persistent inflammation Contraindications Close proximity to a vital structure Inability to locate foreign body before or during the procedure Lack of knowledge of anatomic structures Patient unable to tolerate removal procedure |
Surgical referral is appropriate for difficult cases, including foreign bodies in the face or deep spaces of the hands or feet, multiple shards of broken glass, objects in joints, and neurovascular deficits. For patients who are unable to tolerate procedures, judicious use of sedation and anxiolytics may be beneficial. The physician should be willing to abort the procedure if the object cannot be removed in 15 to 30 minutes.3
Equipment and Preparation
A standard suture tray with gauze, forceps, scalpel, hemostats, and a needle driver should provide most procedure tools. Local anesthetic and tourniquets are commonly used. Lighting should be adequate, and comfortable seating should be available for the patient.
Pain control may be achieved with local soft tissue injection or nerve block with lidocaine or bupivacaine (Marcaine), as well as topical anesthetic, such as lidocaine-epinephrine-tetracaine. Topical antiseptic may reduce contamination. Establishing a bloodless field can improve wound visualization; an elastic tourniquet may be secured proximal to an elevated extremity wound and tightened until blood flow ceases. Alternatively, a Penrose drain, sterile glove, or specialized tourniquet can be used at the base of a finger or toe. Ischemic tourniquets may remain secured for up to 30 minutes.14 In addition, lidocaine with epinephrine can minimize localized bleeding and is safe in digital blocks.15
Foreign Body Removal Techniques
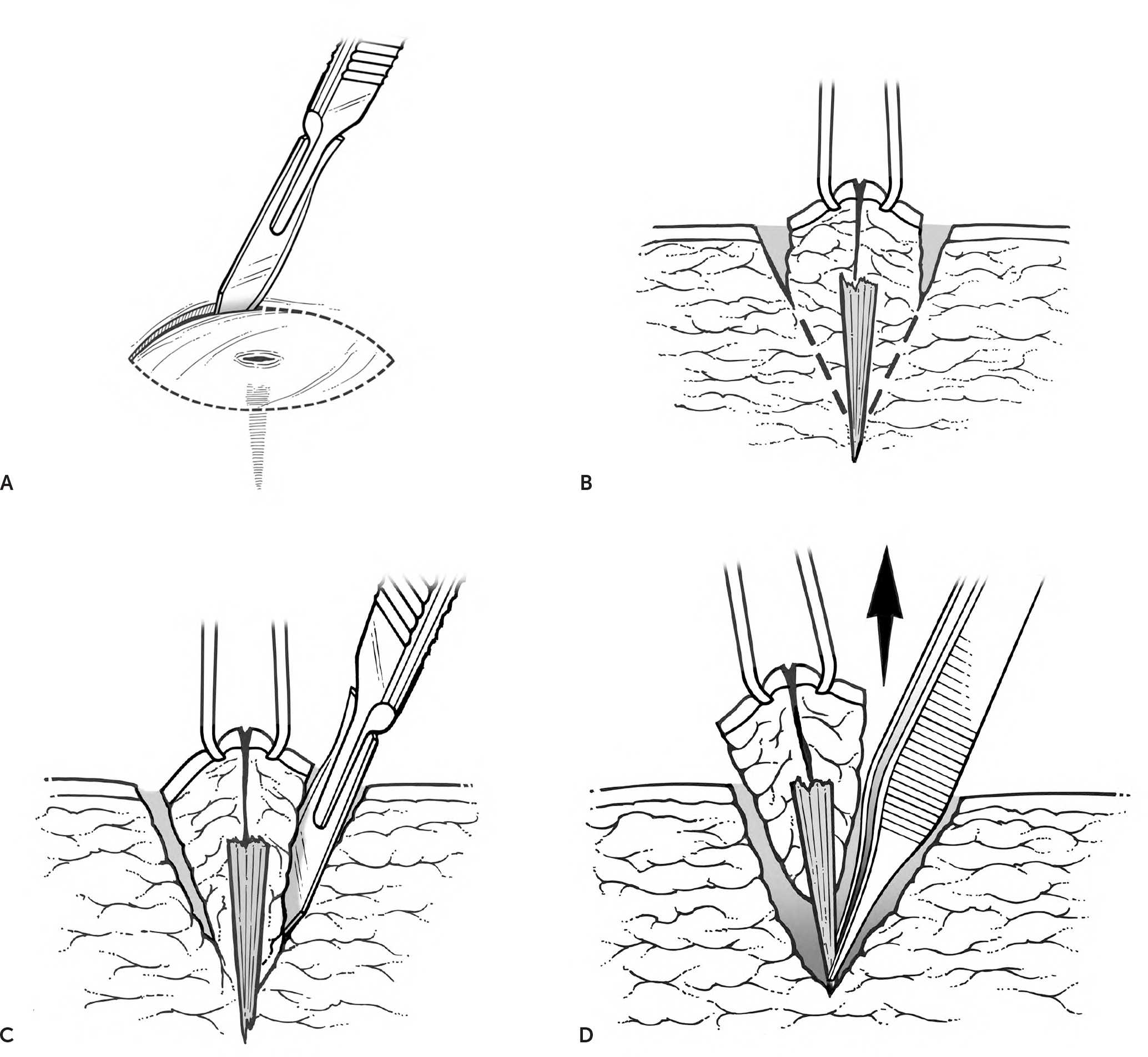
Direct wound visualization is recommended to minimize injury to vital structures. High-risk areas include hands, feet, neck, and face. A dermatoscope may assist with identification of superficial foreign bodies.16 For deeper foreign bodies, visualization may be improved with incisions to enlarge the wound (Figure 317). Probes or spread hemostats may facilitate wound exploration; foreign bodies may be felt or heard upon instrument contact. If a superficial foreign body is difficult to identify or is surrounded by contamination, a small block of tissue may be excised. However, given the increased risk of tissue injury, this should only be performed with knowledge of the underlying anatomy.7
Wound irrigation is recommended after foreign body removal. A 2012 Cochrane review found no difference in infection risk when either normal saline or tap water was used for irrigation.18 Antiseptic solutions should be avoided because of their cytotoxic effects on wound healing.19 Aggressive irrigation should be avoided because it can increase tissue injury through microdissection.20 Pressure with a syringe or intravenous solution bag may help moderate irrigation; however, ideal pressures are unknown.
The wound should be closed as soon as feasible. Wound closure has been associated with decreased pain and healing time, and improved cosmetic results.21,22 Indications for delaying closure include gross contamination and significant tissue injury. In these cases, the wound may be left open and packed for three to five days. If no signs of inflammation or infection are noted at follow-up, delayed primary closure can be performed.7
Types of Foreign Bodies
METALLIC FRAGMENTS AND PROJECTILES
Metallic foreign bodies often become embedded after blasts or projectile weapon injuries. They are generally found in superficial tissue after low-velocity injuries; at higher velocities, they can perforate skin and bone.23 Superficial material that is not embedded near vital structures can be easily removed. Methylene blue injection guided by C-arm (a mobile imaging unit that obtains fluoroscopic imaging during surgical procedures) near metallic foreign bodies aids in detection and removal. One study reported increased success rates, shorter operative time, reduced radiation from decreased C-arm use time, and smaller incisions compared with direct excision guided by C-arm alone.24 Additionally, magnets may help with localization by adhering to embedded metallic material25 or tenting overlying skin,26 and with subsequent removal of ferrous foreign bodies by reducing anesthetic requirement, incision size, and scar tissue.27
FISHHOOKS
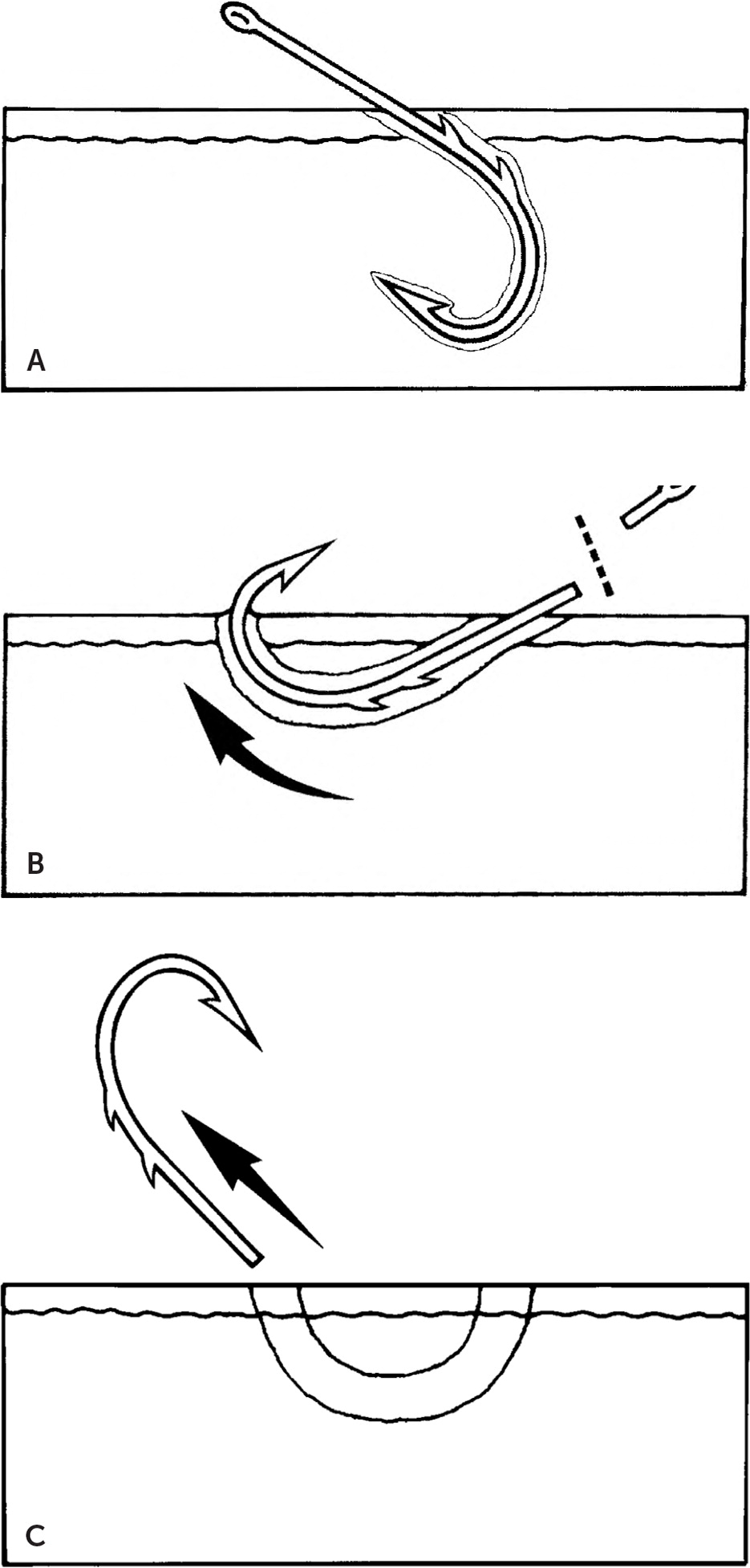
Challenges with fishhook injuries often stem from removal of the barbed end of the hook. Ideally, the hook is removed without causing additional trauma as the hook is withdrawn. If more than one barb is present on the hook, the barbs external to the skin should be taped or clipped to avoid injuring the patient or clinician during removal. Other items attached to the hook, such as lures or string, should be removed. Several methods exist for removing hooks, but the advance and cut method (Figure 428) is reported to have the highest success rate.29 Whichever method is used should be based on the type of fishhook and the location and depth of the injury.30
WOODEN SPLINTERS AND PLANT SPINES
Vegetative foreign bodies embedded in skin are often easily visualized; however, objects in deeper punctures may be challenging to detect. These materials should be removed to reduce inflammatory reactions. Dermoscopy can aid in detection and removal.16 Splinters and spines are generally radiolucent; ultrasonography or magnetic resonance imaging may be used for further evaluation.31 Many plant spines are barbed, which may complicate removal and result in retained material. To minimize this risk, spines should be removed with tweezers, and polyvinyl acetate glue and a mesh pad should be applied to the puncture site. The pad can be removed after the glue has dried, effectively removing remaining material.31
GLASS, GRAVEL, AND PLASTIC
Skin abrasions may contain embedded glass, gravel, or plastic. These are typically superficial and easily removed; however, wound exploration can ensure that additional material is not retained in deeper soft tissue. These materials are often radiopaque and may be visualized with underpenetrated radiography.32 However, plastics vary in composition and may not be detected.6
TRAUMATIC TATTOOING
Particulate matter such as asphalt, gunpowder, or graphite from pencils may be deposited into skin and soft tissue after a traumatic injury. If the debris is not removed from the dermis before reepithelialization, tissue tattooing occurs. Piecemeal removal is not feasible. Hydrosurgical techniques using high-pressure tangential fluid jets are effective for immediate debridement,33 whereas laser therapy is effective for established tattoos.34
MARINE FOREIGN BODIES
Common marine foreign bodies include sea urchin spines, jellyfish nematocysts, coral reef fragments, and catfish barbs. These may trigger severe inflammatory reactions and bacterial infections. Most wounds are superficial, with foreign bodies removed by debridement and gentle washing with water of similar salinity. Sharp, rigid barbs and spines may embed more deeply and require radiography or ultrasonography for localization. Puncture wounds in stagnant freshwater are at high risk of infection, particularly by Aeromonas. Wounds in saltwater are less likely to become infected but should be evaluated frequently for Vibrio infection.35 Venom or toxin exposures may complicate these injuries.
HUMAN AND ANIMAL BITES
Human, dog, and cat bites are common presenting injuries; occasionally, fragments of teeth may be embedded, especially in deep puncture wounds from cat bites. Injuries typically involve the hands, head, and face. Wound exploration may be needed for further evaluation.7 Animal bites are reportable in many states.
Disposition
ANTIBIOTICS
| Bite or oral wound Delayed presentation (> 18 hours) Gross contamination with inadequate cleaning Joint, tendon, or cartilage involvement Puncture wounds, crush injuries, open fractures Retained foreign body Significant immunocompromise |
Antibiotic selection should be based on the bacterial flora likely present at the time of trauma. For most wounds, a first-generation cephalosporin (cephalexin [Keflex] or cefazolin) or penicillinase-resistant penicillin (dicloxacillin or nafcillin) is appropriate. Most infections are unlikely to be associated with methicillin-resistant Staphylococcus aureus, but trimethoprim/sulfamethoxazole, clindamycin, or tetracyclines (minocycline [Minocin] or doxycycline) may be selected if increased risk is suspected.37,38
Wounds with embedded teeth should be treated based on pathogenic oral flora common to the offending species. Doxycycline is often preferred because of its excellent coverage against Pasteurella multocida (cats and dogs) and Eikenella (human).38 When treating wounds occurring in saltwater or brackish water, doxycycline plus ceftriaxone (Rocephin) or cefotaxime (Claforan) should be considered to target Vibrio.38 For wounds occurring in fresh water, doxycycline plus ciprofloxacin or ceftriaxone should be considered to cover Aeromonas.38 Plantar puncture wounds through foot-wear may allow Pseudomonas transfer through the sole; these wounds should be treated with fluoroquinolones.39
TETANUS IMMUNIZATION
Administration of tetanus toxoid–containing vaccine and tetanus immune globulin may be warranted after an injury depending on the patient’s age and vaccination history, the time since the last tetanus toxoid–containing vaccine was given, and whether the wound is clean and minor or at high risk of tetanus40 (eTable A). Wounds not considered clean and minor include those contaminated with dirt, feces, soil, or saliva; puncture wounds; avulsions; and wounds resulting from projectiles, crush injuries, burns, or frostbite.
| Tetanus vaccination history | Type of wound | Tetanus vaccine booster* | Tetanus immune globulin |
|---|---|---|---|
| 3 or more doses Fewer than 5 years since previous dose | All wounds | No | No |
| 5 to 10 years since previous dose | Clean, minor wounds | No | No |
| All other wounds | Yes | No | |
| More than 10 years since previous dose | All wounds | Yes | No |
| Fewer than 3 doses or uncertain vaccination history | Clean, minor wounds | Yes | No |
| All other wounds | Yes | Yes |
Data Sources: PubMed and the Cochrane database were searched using terms such as foreign bodies, wounds, soft tissue, injuries, and lacerations. The search included randomized controlled trials, meta-analyses, clinical trials, and clinical reviews. Search dates: March and April 2019, and February 2020.
The authors thank the medical care team at the 455th Expeditionary Medical Operations Squadron, Craig Joint Theater Hospital, Bagram Airfield, Afghanistan; imaging was obtained during patient care. Image request for this article underwent review by the U.S. Army Medical Research and Material Command IRB office before manuscript submission.
The authors assume full responsibility for the ideas and opinions expressed in this article, which should not be considered the opinions of the U.S. Air Force or the Department of Defense.
