
Am Fam Physician. 2021;103(10):625-627
Author disclosure: No relevant financial affiliations.
A 40-year-old patient presented with new-onset abdominal pain, nausea, and vomiting. The patient did not have fever, diarrhea, or changes in bowel movements. The medical history included hypertension, anxiety, obstructive sleep apnea, and recurrent pancreatitis complicated by pancreatic necrosis secondary to chronic alcohol abuse.
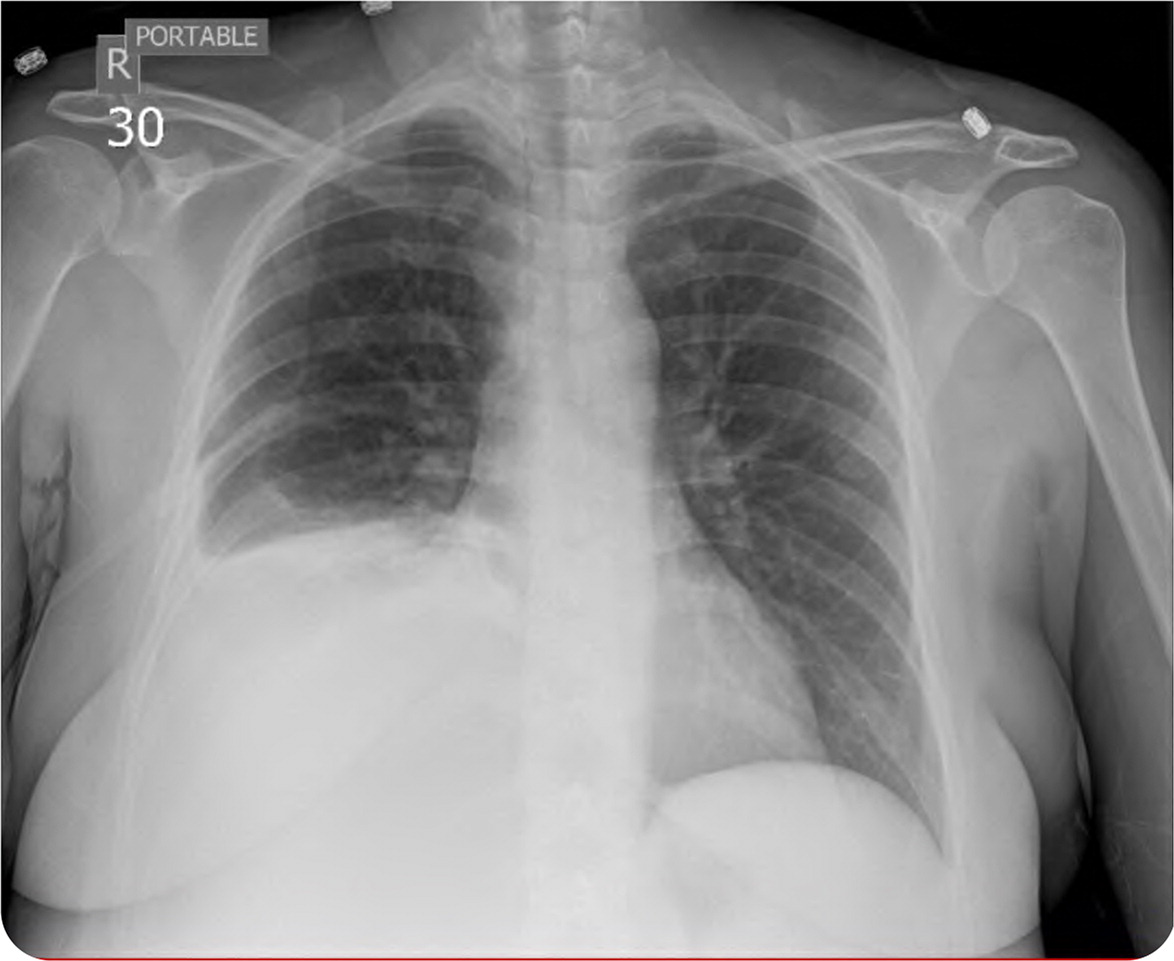
Initial laboratory findings included elevated lipase and mildly elevated triglyceride levels consistent with recurrent pancreatitis. The patient was admitted for initiation of intravenous fluids, nutritional support, and pain management but was transferred to a tertiary care center after developing a fever, shortness of breath, and a need for supplemental oxygen. Physical examination revealed diminished breath sounds at the right lung base. Chest radiography was obtained (Figure 1).
Question
Based on the patient's findings, which one of the following is the most likely diagnosis?
A. Chylothorax.
B. Hemidiaphragm paralysis.
C. Lobar pneumonia.
D. Pleural effusion.
E. Subphrenic pancreatic pseudocyst.
Discussion
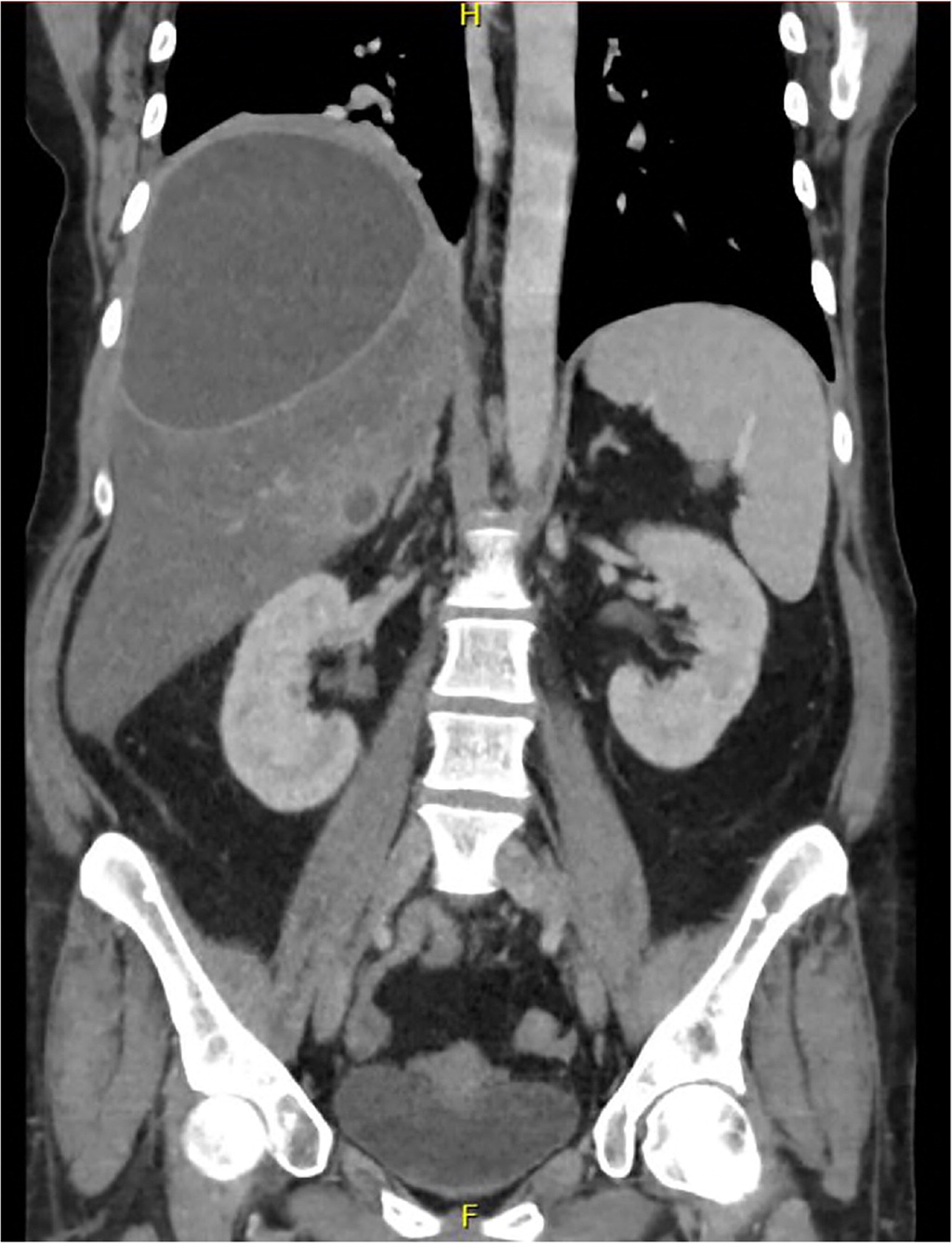
The answer is E: subphrenic pancreatic pseudocyst. The chest radiograph showed a large right-sided pleural effusion and blunting of the costophrenic angle. Point-of-care ultrasonography performed in preparation for thoracentesis did not reveal any appreciable pleural effusion. A subsequent computed tomography (CT) scan of the chest, abdomen, and pelvis (Figure 2) demonstrated a loculated, complex, proteinaceous fluid collection measuring 14 cm × 13 cm × 12 cm (estimated volume = 1,100 mL) in the right subphrenic space, which was compressing the right liver lobe and surrounding structures. Fluid obtained through fine-needle aspiration guided by endoscopic ultrasonography showed very high amylase content and a low carcinoembryonic antigen level, which are consistent with a pancreatic pseudocyst.
Pancreatic pseudocysts occur in 30% to 40% of patients with chronic pancreatitis.1 They consist of fluid containing pancreatic enzymes, blood, and necrotic tissue. Symptoms include abdominal pain, early satiety, weight loss, and jaundice. Alcohol-related pancreatitis accounts for up to 78% of all pseudocysts.1 Most pseudocysts occur in the head and body of the pancreas, but up to 22% are extrapancreatic.2–4 Hepatic involvement is rare with pseudocysts.3–5
Chylothorax is the accumulation of chyle, which is composed of fat droplets and lymph fluid, in the pleural cavity. This can be due to damage or dysfunction of the thoracic duct from congenital abnormalities of the lymphatic system, malignancies such as lymphoma and leukemia, infections such as tuberculosis, and trauma. Chylothorax is most commonly a result of postoperative injury to the thoracic duct. Lymphocyte- and lipid-rich fluid on thoracentesis confirms the diagnosis.7
Hemidiaphragm paralysis may be asymptomatic and found incidentally on chest radiography, or it may present as dyspnea and diminished exercise capacity. Chest radiography shows elevation of the affected hemidiaphragm with associated atelectasis. There are various causes, including trauma, injury from surgery or mechanical ventilation, metabolic and inflammatory conditions, myopathies, neuropathies, mediastinal masses, and obstructive lung diseases. Prognosis is based on pulmonary function testing.8
Lobar pneumonia typically presents as cough, fever, dyspnea, and pleuritic chest pain. Streptococcus pneumoniae is the most common cause in adults. Diagnosis is confirmed with a chest radiograph demonstrating consolidation in the affected lobe. Chest CT can be used for further evaluation if alternative diagnoses are suspected. Blood and sputum cultures should be obtained to direct antibiotic therapy.9
Pleural effusion is fluid collection between the parietal and visceral lung pleura and can present as cough, chest pain, dyspnea, and pleurisy. Effusions may be transudative from heart failure, liver failure with ascites, or nephrotic syndrome or exudative from infection or malignancy. Chest radiography shows dense fluid accumulation forming a meniscus at the costophrenic angle. Ultrasonography and chest CT are more sensitive for detecting pleural effusion. Thoracentesis can be diagnostic and therapeutic.10
| Condition | Characteristics |
|---|---|
| Chylothorax | Accumulation of chyle in the pleural cavity, most commonly from postsurgical injury to the thoracic duct |
| Hemidiaphragm paralysis | Dyspnea and diminished exercise capacity, if symptomatic; various causes |
| Lobar pneumonia | Cough, fever, dyspnea, and pleuritic chest pain; radiography shows consolidation in the affected lobe; Streptococcus pneumoniae is the most common cause in adults |
| Pleural effusion | Fluid collection between the parietal and visceral lung pleura; cough, chest pain, dyspnea, and pleurisy; may be transudative from heart failure, liver failure with ascites, or nephrotic syndrome or exudative from infection or malignancy |
| Subphrenic pancreatic pseudocyst | Collection of fluid containing pancreatic enzymes, blood, and necrotic tissue; symptoms include abdominal pain, early satiety, weight loss, and jaundice; common complication of chronic pancreatitis |
