
This is a corrected version of the article that appeared in print.
Am Fam Physician. 2022;105(1):39-49
Patient information: See related handout on orthostatic hypotension, written by the authors of this article.
Author disclosure: No relevant financial relationships.
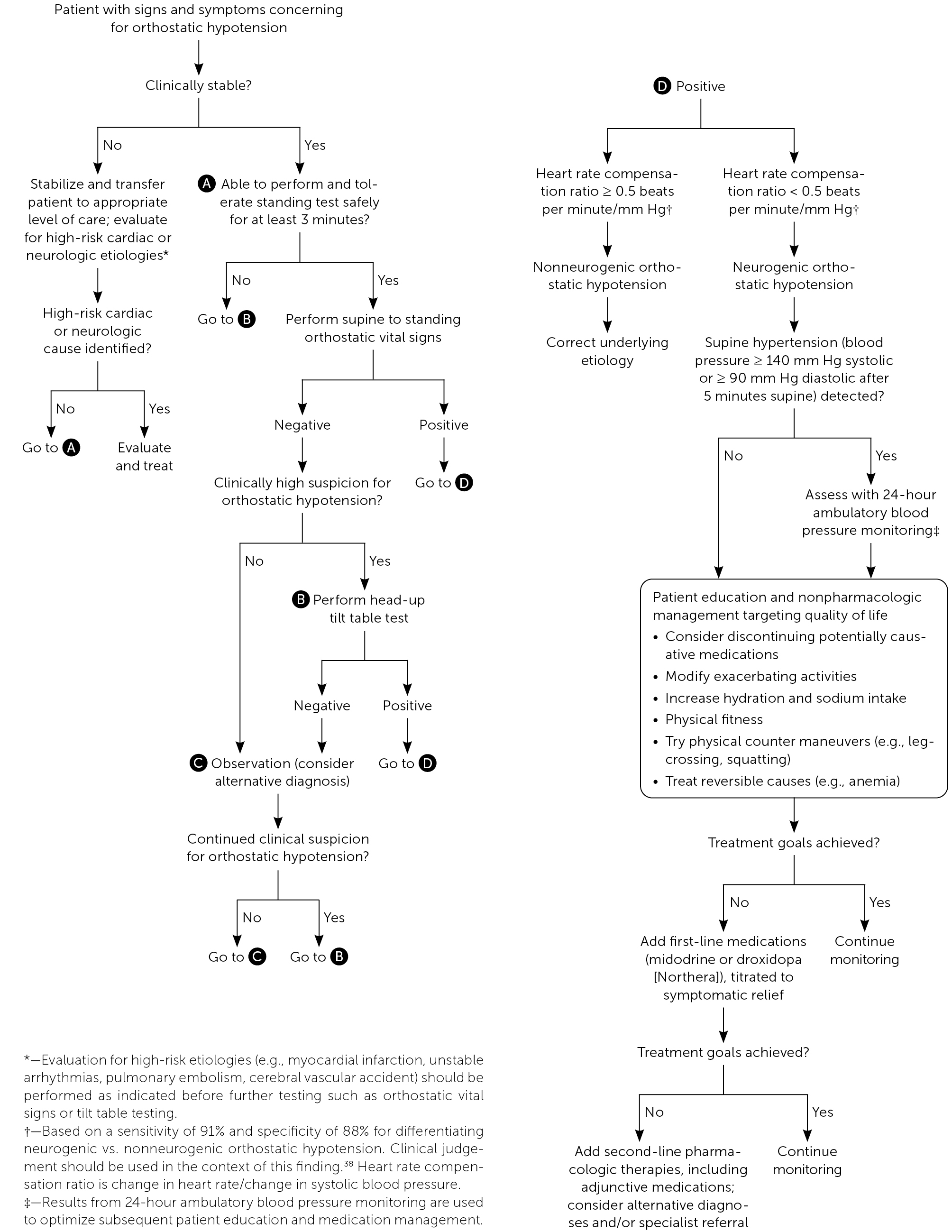
Orthostatic hypotension is defined as a decrease in blood pressure of 20 mm Hg or more systolic or 10 mm Hg or more diastolic within three minutes of standing from the supine position or on assuming a head-up position of at least 60 degrees during tilt table testing. Symptoms are due to inadequate physiologic compensation and organ hypoperfusion and include headache, lightheadedness, shoulder and neck pain (coat hanger syndrome), visual disturbances, dyspnea, and chest pain. Prevalence of orthostatic hypotension in the community setting is 20% in older adults and 5% in middle-aged adults. Risk factors such as diabetes mellitus increase the prevalence of orthostatic hypotension in all age groups. Orthostatic hypotension is associated with a significant increase in cardiovascular risk and falls, and up to a 50% increase in relative risk of all-cause mortality. Diagnosis is confirmed by measuring blood pressure and heart rate after five minutes in the supine position and three minutes after moving to a standing position. [corrected] If the patient is unable to stand safely or the clinical suspicion for orthostatic hypotension is high despite normal findings on the bedside test, head-up tilt table testing is recommended. Orthostatic hypotension is classified as neurogenic or nonneurogenic, depending on etiology and heart rate response. Treatment goals for orthostatic hypotension are reducing symptoms and improving quality of life. Initial treatment focuses on the underlying cause and adjusting potentially causative medications. Nonpharmacologic strategies include dietary modifications, compression garments, physical maneuvers, and avoiding environments that exacerbate symptoms. First-line medications include midodrine and droxidopa. Although fludrocortisone improves symptoms, it has concerning long-term effects.
Orthostatic hypotension is defined as a decrease in blood pressure of 20 mm Hg or more systolic or 10 mm Hg or more diastolic within three minutes of standing from the supine position or on assuming a head-up position of 60 degrees during tilt table testing.1 It is classified as neurogenic or nonneurogenic based on etiology and heart rate response.
With increasing age, there is a normal decline in baroreceptor sensitivity and increase in autonomic neurodegenerative disease.2 Orthostatic hypotension occurs in only 5% of middle-aged adults but affects approximately 20% of those 60 years and older.3–5 Prevalence in nursing homes and geriatric wards is as high as 50% and 68%, respectively.1,6
Orthostatic hypotension is associated with significant morbidity and mortality, with the greatest risk in those who have comorbidities. Several large meta-analyses reported that orthostatic hypotension is associated with up to a 50% increase in relative risk of all-cause mortality (relative risk [RR] = 1.50; 95% CI, 1.24 to 1.81).7–9 In middle-aged, community-dwelling patients, it is associated with an increased risk of death (hazard ratio = 1.19 [95% CI, 1.09 to 1.30] to 1.70 [95% CI, 1.40 to 2.00]) after adjustment for other risk factors.10,11
Orthostatic hypotension is also associated with increased rates of coronary heart disease, myocardial infarction, heart failure, stroke, and falls.3,8–10 Older people especially are at risk of myocardial infarction and recurrent falls.12,13 Patients with diabetes mellitus are more likely to develop orthostatic hypotension and have an increased risk of mortality, microvascular and macrovascular complications, and cardiovascular events.14–18 In the United States, the rate of hospitalizations related to orthostatic hypotension is 36 per 100,000 adults and increases to 233 per 100,000 adults for those 75 years and older.19
Pathophysiology
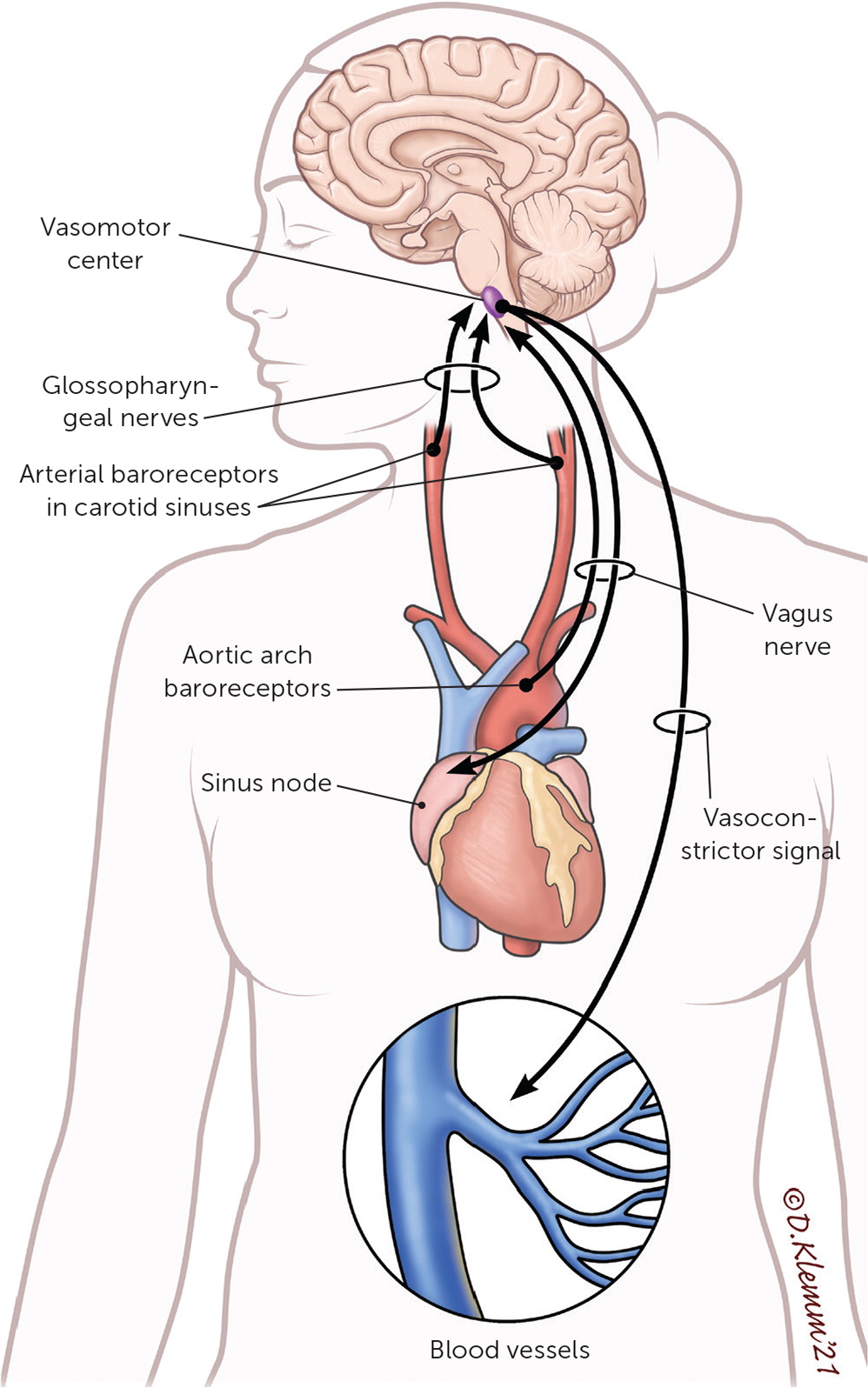
Approximately 500 to 1,000 mL of blood pools in the splanchnic circulation and lower extremities when a person stands, causing a decrease in venous return and cardiac output.2,20–22 Baroreceptors detect decreased stretch and activate the sympathetic nervous system, which elevates the heart rate, bolsters contractility, and increases peripheral resistance through vasoconstriction.2,21 Baroreceptors also sense decreased blood volume, prompting upregulation of renin release, sodium reabsorption, and vasopressin activity, resulting in enhanced water retention.2,21 Orthostatic hypotension occurs when there is inadequate intravascular volume or when sympathetic nervous system–mediated vasoconstriction is unable to compensate for gravitational pooling, leading to decreased organ perfusion and associated symptoms 20,23 (Figure 1).
Clinical Presentation and Evaluation
Symptoms of orthostatic hypotension appear while assuming a standing or upright position and are relieved by returning to a supine position (Table 1).2,22,24 These symptoms are due to organ hypoperfusion compensation, but they do not have to be present for a diagnosis.2,5 A history and physical examination aimed at identifying underlying causes of orthostatic hypotension should be performed. Risk factors for orthostatic hypertension are outlined in Table 2.19,24,25
| Cardiovascular Chest pain Palpitations Cerebral Cognitive slowing Lightheadedness Syncope and presyncope Vertigo Gastrointestinal Nausea Hematologic Pallor Weakness | Pulmonary Dyspnea (hypoperfusion of apices) Fatigue Platypnea (ventilation perfusion mismatch with upright positioning) Retina Blurry vision Dimmed vision Upper body muscles Neck and shoulder pain (coat hanger syndrome) |
| A syncopal episode or an unexplained fall |
| Neurodegenerative disorders known to be associated with autonomic dysfunction (dementia with Lewy bodies, multiple system atrophy, Parkinson disease, pure autonomic failure) |
| Older adults (≥ 70 years of age) who are frail or taking multiple medications |
| Peripheral neuropathies known to be associated with autonomic dysfunction (amyloidosis, diabetes mellitus, HIV) |
| Postural (orthostatic) dizziness or nonspecific symptoms that occur only when standing |
Orthostatic hypotension is diagnosed by measuring blood pressure and heart rate after five minutes in the supine position and three minutes after moving to a standing position.26 [corrected] There is no standard timing of measurements (e.g., one-minute intervals, one-minute and three-minute intervals) or positioning (e.g., supine to sitting, supine to standing, sitting to standing, all three).19,24,26,27 Supine to standing measurements evoke the greatest hemodynamic changes and are more sensitive.27,28 A sustained decrease in blood pressure of 20 mm Hg or more systolic or 10 mm Hg or more diastolic within three minutes of standing is diagnostic of orthostatic hypotension.1,26
Variations in the time it takes for blood pressure to fall allow orthostatic hypotension to be classified as classic (within three minutes), initial (within 15 seconds), and delayed (after three minutes).2,22,26 Although the clinical significance of these variants is not completely understood, it suggests that orthostatic hypotension is a spectrum of disordered physiology.1,29–31 A large prospective study reported an association with adverse events (e.g., fall, fracture, syncope, death) in patients 45 to 64 years of age if orthostatic hypotension occurred within one minute of standing.32
Orthostatic hypotension is further classified as neurogenic or nonneurogenic2,4,6,22,24,33 (Table 32,4,6,20–22,24,33). Neurogenic orthostatic hypotension is caused by an intrinsic failure of the autonomic nervous system to create a normal physiologic response (baroreflex dysfunction). The differential diagnosis includes neurodegenerative disorders, pure autonomic failure, small fiber neuropathies, and acquired disorders.2,4,6,22,24 Nonneurogenic orthostatic hypotension is secondary to external factors (often medication use) inhibiting the body's normal compensatory pattern.
| Neurogenic Acquired Spinal cord injury Traumatic brain injury Autonomic alpha-synucleinopathies Dementia with Lewy bodies Multiple system atrophy Parkinson disease Pure autonomic failure Idiopathic immune-mediated autonomic neuropathy Paraneoplastic autonomic neuropathy Peripheral autonomic disorders Diabetes mellitus Hereditary amyloidosis Primary amyloidosis Sjögren syndrome Nonneurogenic Endocrine Adrenal insufficiency Diabetes Hyperglycemia Hypokalemia Hypothyroidism Iatrogenic Medications Infections AIDS Distributive shock Intoxication Substance abuse (drugs or alcohol) Metabolic Vitamin B12 deficiency Trauma Blood loss Vascular Anemia Arrhythmia Congestive heart failure Dehydration Myocardial infarction Pregnancy/postpartum Venous insufficiency |
Measuring heart rate with each position change can help detect baroreflex dysfunction.2,22,24,27 The compensatory rise in heart rate is maintained in nonneurogenic orthostatic hypotension, whereas the heart rate response is markedly reduced or absent in neurogenic orthostatic hypotension.2,26 An increase in heart rate of 0.5 beats per minute or more for every mm Hg decrease in systolic blood pressure has a high sensitivity (91%) and specificity (88%) for nonneurogenic orthostatic hypotension.34,35 Additional features that differentiate the two are outlined in Table 4.2,22,34,35
| Parameter | Neurogenic | Nonneurogenic |
|---|---|---|
| Heart rate compensation ratio (change in heart rate/change in systolic blood pressure) | Decreased or absent (< 0.5 beats per minute/mm Hg) | Marked (≥ 0.5 beats per minute/mm Hg) |
| Symptoms of systemic autonomic failure | Urinary dysfunction, gastrointestinal dysfunction, postprandial hypotension; symptoms worse in the morning | None |
| Neurologic deficits | Parkinsonism, cognitive dulling, cerebellar signs, peripheral sensory abnormalities | None |
| Definition | Clinical features |
|---|---|
| Postural orthostatic tachycardia syndrome | |
| Symptoms occur with upright positioning and are relieved with laying down; symptoms commonly include lightheadedness, palpitations, generalized weakness, tremors, and fatigue and Increase in sustained heart rate ≥30 beats per minute within 10 minutes of standing from supine or head-up tilt (patients who are 12 to 19 years of age must have a heart rate increase of ≥40 beats per minute) and Absence of orthostatic hypotension (decrease in systolic blood pressure of ≤20 mm Hg) | Prevalence of 0.2% to 1% in the general population Standing heart rate is typically ≥120 beats per minute Symptoms are worse in the mornings Typically chronic (three to six months) Most prominent between 15 and 25 years of age; most cases are in those younger than 50 years Significantly affects quality of life, although there is no clear mortality risk |
| Orthostatic intolerance | |
| Syndrome defined by frequent symptoms that make it difficult to remain in an upright posture; symptoms typically include lightheadedness, palpitations, generalized weakness, tremulousness, blurred vision, and fatigue | Symptoms associated with standing position Can occur with or without orthostatic hypotension, syncope, and tachycardia |
For unclear cases of orthostatic hypotension or when patients are unable to safely stand, head-up tilt table testing is recommended. Indications and example procedures for this test are described in Table 6.20,33,35,42 Limited studies suggest that head-up tilt table testing has higher sensitivity for orthostatic hypotension than bedside orthostatic vital signs. If findings on the initial assessment for orthostatic hypotension in moving from the supine and standing postion are normal, but the clinical suspicion for orthostatic hypotension is high, head-up tilt table testing should be considered.24,28,33,43,44 Head-up tilt table testing is also recommended for detecting suspected delayed orthostatic hypotension in patients with syncope.39

| Indications |
| High index of suspicion for orthostatic hypotension despite normal bedside orthostatic vital signs (e.g., simplified Schellong test) |
| Assessment of chronic orthostatic intolerance (e.g., postural orthostatic tachycardia syndrome) |
| Unexplained transient loss of consciousness |
| Inability to tolerate assessment of standing orthostatic vital signs because of motor issues or symptoms |
| Monitoring the disease course of an autonomic disorder to guide therapy |
| Protocol* |
| Environment and patient factors should be optimized according to the goal of testing and suspected disorder. Testing room should be quiet with a temperature of 68°F to 75°F (20°C to 24°C). Time of day of testing, proximity to meals, psychological state, and prescribed medications should be adjusted to yield the highest sensitivity. |
| Patient should have an empty bladder and be secured to a tilt table using straps. A supine position should be maintained for at least 10 minutes. |
| Continuous, noninvasive blood pressure and heart rate monitoring should be assessed for the duration of the test. |
| From a horizontal plane, the patient is slowly tilted upright between 60 and 80 degrees. |
| Duration of tilting varies by clinical question. For detecting orthostatic hypotension, the typical duration is five minutes. |
| The test should be terminated when diagnostic criteria are achieved, the patient becomes intolerant of the test (severe symptoms, adverse effects,† elective termination), or the protocol is completed. |
Supine hypertension is defined as blood pressure of 140 mm Hg or higher systolic or 90 mm Hg or higher diastolic after five minutes in the supine position and affects about 50% of patients with neurogenic orthostatic hypotension.2,21,22,25,45 Anti-hypotensive medications may worsen supine hypertension; therefore, screening for supine hypertension is recommended for all patients with neurogenic orthostatic hypotension.22,45 Because of a higher baseline blood pressure in patients with supine hypertension, orthostatic hypotension is diagnosed with a decrease in systolic blood pressure of 30 mm Hg or more.1,45 If supine hypertension is suspected, 24-hour ambulatory blood pressure monitoring can be used to assess severity (particularly nocturnal hypertension) and tailor therapies based on activities throughout the day.45
| Test | Reasoning |
|---|---|
| B12 methylmalonic acid | Evaluate for evidence of B12 deficiency |
| Basic metabolic panel | Evaluate for electrolyte disturbances, acid-base disorder, renal dysfunction, or diabetes mellitus |
| Complete blood count | Evaluate for anemia or infection |
| Electrocardiography* | Evaluate for arrhythmia that is causing symptoms of orthostatic hypotension requiring cardiology referral |
| Screening for supine hypertension | Supine hypertension affects about 50% of patients with neurogenic orthostatic hypotension; supine hypertension changes the diagnostic criteria for orthostatic hypotension; antihypotensive medications may worsen supine hypertension, requiring close monitoring |
| Thyroid-stimulating hormone | Evaluate for evidence of thyroid dysfunction |
Management
Treatment goals for orthostatic hypotension are reducing symptoms and improving quality of life, rather than normalizing blood pressure.2,22,24,46 Management begins with identifying and treating the underlying cause. The patient's current medications should be evaluated and potentially causative agents adjusted if safe to do so (Table 8).2,20,22,24,46,47
| Anticholinergic agents |
| Antihypertensives |
| Centrally acting alpha-2 agonists |
| Negative inotropic/chronotropic agents: beta-adrenergic blockers, nondihydropyridine calcium channel blockers |
| Preload reducers: diuretics, nitrates, phosphodiesterase-5 inhibitors |
| Renin-angiotensin system antagonists: angiotensin-converting enzyme inhibitors, angiotensin receptor blockers |
| Vasodilators: alpha-1 adrenergic antagonists, dihydropyridine calcium channel blockers, direct vasodilators |
| Dopaminergic agents |
| Opioids |
| Psychoactive medications: antipsychotics, sedative hypnotics, tricyclic antidepressants |
Antihypertensives can exacerbate orthostatic hypotension symptoms because they reduce intravascular volume, trigger vasodilation, and have negative chronotropic effects.22,24 Nighttime dosing of antihypertensives should be considered to reduce orthostatic hypotension symptoms.22,24,49 Use of a 24-hour ambulatory blood pressure monitor may be helpful in guiding this decision.22,45,49
NONPHARMACOLOGIC MANAGEMENT
Initiating lifestyle-based treatments, such as avoiding or modifying exacerbating activities, is the first-line approach for the management of neurogenic orthostatic hypotension.2,22,24,46 Although there is conflicting evidence of their effectiveness, expert consensus guidelines advocate the use of nonpharmacologic treatments because of minimal risk of harm.2,22,24,33
Hot and humid conditions can exacerbate symptoms via vasodilatory cooling. Patients should be vigilant in avoiding environmental exposures and exacerbating activities.2,22,24 Postprandial hypotension is common in neurogenic orthostatic hypotension because of redistribution of blood volume to the splanchnic circulation. Diets should include frequent small meals to minimize this effect.2,22,24,50 Physical fitness should be encouraged because bed rest can further exacerbate orthostatic hypotension.2 Exercise regimens in older people have been shown to improve head-up tilt table testing results.51 Modifications should be made as needed to alleviate symptoms during exercise, such as avoiding frequent position changes.2,24
Appropriate volume status is maintained by adequate hydration and sodium intake. Physicians should assess the risks of increased water and sodium intake in patients with comorbid conditions such as heart failure, cirrhosis, or chronic kidney disease. Consumption of 2 to 2.5 L of fluids per day is recommended to counteract expected urinary losses.2,20,22,24 Increased salt intake has been shown to provide short-term symptom improvement.52 Patients should aim for at least 2 to 3 g of sodium intake per day through dietary sources or salt tablets. A urinary sodium excretion of more than 170 mEq per L (170 mmol per L) every 24 hours and a urinary volume of more than 1,500 mL indicate adequate fluid and sodium intake.2,20
Physical counter maneuvers, including leg-crossing or squatting, in addition to wearing waist-high compression garments with graded pressures of 30 to 40 mm Hg, may be used to reduce venous pooling in the legs and splanchnic circulation.53,54,46 However, the use of compression garments is limited by poor compliance.22,53,54
Elevating the head of the bed by 30 to 45 degrees at night can theoretically prevent supine hypertension, which exacerbates morning orthostatic hypotension by promoting nocturnal diuresis and natriuresis. One trial demonstrated that this did not change 24-hour ambulatory blood pressure values or urinary volume.55
PHARMACOLOGIC MANAGEMENT
Two medication strategies can be used to augment nonpharmacologic management if it is insufficient alone. Midodrine and droxidopa (Northera) act to increase peripheral vascular resistance, whereas fludrocortisone expands intravascular volume.2,22 The choice of medication is guided by underlying etiology, patient preference, adverse effects, cost, and therapeutic response.22 Specific medication dosages and considerations in the management of orthostatic hypotension are summarized in Table 9.2,21,22,24,56–65
| Drug* | Dosage | Comments | Cost† |
|---|---|---|---|
| Midodrine | Start at 2.5 mg three times per day orally, and titrate up to 10 mg three times per day | Dosage of 10 mg three times per day improves standing blood pressure measurements and symptom scores during a six-week course56–58 Avoid three to five hours before bedtime22,24 | 10 mg: $33 (—) for 60 tablets |
| Droxidopa (Northera) | Start at 100 mg three times per day orally, and titrate up to 600 mg three times per day | Improvement in symptom score based on validated assessment tool with medication titrated to symptom and blood pressure response over 14 days (mean dose = 430 mg)60 Avoid five hours before bedtime24 Effects may be blunted if coadministered with carbidopa22 | Only available at specialty pharmacies |
| Fludrocortisone | Start at 0.1 mg once per day orally, and titrate up to 0.2 mg once per day | Improvement in symptoms based on validated assessment over three-week treatment period with 0.1 mg once per day orally62 Use caution in heart failure Potassium level should be monitored 2,22,24 | 0.1 mg: $13 (—) for 30 tablets |
| Atomoxetine (Strattera) | 18 mg once per day orally | Improvement in standing blood pressure and validated symptom scores2,64,65 | 18 mg: $27 ($392) for 30 tablets |
| Pyridostigmine (Mestinon) | 60 mg once per day orally | Improved postural diastolic blood pressure reduction with 60-mg dosage63 | 60 mg: $9 ($508)for 30 tablets |
Midodrine, a short-acting alpha-1 adrenergic agonist that acts via vasoconstriction, has been shown to alleviate symptoms of orthostatic hypotension and elevate blood pressure in multiple randomized placebo-controlled trials.22,24,56–58,64,66 It is approved by the U.S. Food and Drug Administration for the treatment of orthostatic hypotension and is a recommended first-line medication.2,22,24,56–58,64,66 A double-blind, multicenter, randomized controlled trial of 171 patients demonstrated significant improvement in global symptom scores and standing systolic blood pressure in patients treated with midodrine, 10 mg, three times per day.56 Midodrine can cause supine hypertension and should be avoided within three to five hours of bedtime.2,22,24,66 Other common adverse effects include piloerection, scalp itching, and urinary retention.2,22,24,64,66
Droxidopa, a short-acting norepinephrine precursor, is another first-line medication approved by the U.S. Food and Drug administration for the treatment of orthostatic hypotension. Based on validated symptom scores, this medication increases standing systolic blood pressure and alleviates orthostatic hypotension symptoms.2,24,59,66 Droxidopa should also be avoided before bedtime because it can cause supine hypertension.2,24,59 The most common adverse effects are headaches and nausea. Falls, dizziness, and urinary tract infections have also been reported.65 Patients with neurogenic orthostatic hypotension secondary to Parkinson disease who are treated with droxidopa have a reduced risk of falls.67
Fludrocortisone is a synthetic mineralocorticoid that promotes renal sodium reabsorption, thereby increasing intravascular volume.2,24 Additionally, it increases vascular alpha-adrenergic receptor sensitivity, promoting vasoconstriction.2,24 Expert consensus recommends the off-label use of fludrocortisone in the treatment of orthostatic hypotension.2,22,24 One small (n = 17), short-term (three weeks) study demonstrated an improvement in symptom scores with the use of this medication.60 There are significant adverse effects,2,22,24,66 and its use is cautioned in patients with heart failure. Fludrocortisone has long-term risks, including left ventricular hypertrophy, renal failure, and hospitalization.22,68
Referral
There are limited evidence-based referral criteria for orthostatic hypotension. Symptoms that are incapacitating or severely impact activities of daily living and a 30 mm Hg or more drop in systolic blood pressure may warrant a specialist evaluation.24 Cardiology referral may be considered for known heart disease or abnormal electrocardiogram findings.33,70 Other reasons for referral include treatment failure, significant gastrointestinal impairment, or physician discomfort in treatment.24,46
This article updates previous articles on this topic by Lanier, et al.,20 and Bradley and Davis.71
Data Sources: PubMed searches were completed using the key terms orthostatic hypotension, neurocardiogenic syncope, neurogenic orthostatic hypotension, tilt table test, Schellong test, synucleinopathies, neurocardiogenic syncope, orthostatic intolerance, postural orthostatic tachycardia, syncope, supine hypertension, neuropathy. The searches included systematic reviews, meta-analyses, randomized controlled trials, cohort studies, and review articles. We also searched Essential Evidence Plus and Clinical Evidence, Trip database, and Agency for Healthcare Research and Quality. Search dates: September 2020, October 2020, December 2020, and September 2021.
The opinions and assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the Department of Defense, Uniformed Services University of the Health Sciences, or the Department of the Air Force.
