
Am Fam Physician. 2022;105(1):50-54
Author disclosure: No relevant financial relationships.
Transient global amnesia (TGA) is a clinical syndrome characterized by anterograde amnesia, mild retrograde amnesia, and confusion up to 24 hours. Most commonly seen in patients older than 50 years, TGA results from the temporary impairment of short-term memory formation. Clinically, patients have time disorientation and often ask repeated questions regarding the day's events. Vomiting, headache, blurry vision, dizziness, and nausea may be present. A physically or psychologically stressful precipitating event, such as emotional stress, significant physical exertion, exposure to extreme temperatures, high-altitude conditions, Valsalva maneuver, acute illness, or sexual intercourse, is often the cause. The pathophysiology of TGA is not well understood but may be related to impaired venous drainage of the hippocampus. The diagnosis is primarily clinical, but recent studies suggest that magnetic resonance imaging may be helpful. TGA is self-limited and resolves within 24 hours. There is no established treatment for episodes. The lifetime recurrence rate is 2.9% to 23.8%. Recent evidence suggests an association between TGA and migraine headaches as well as takotsubo cardiomyopathy. No apparent increased risk of cerebrovascular events occurs in patients who have had an episode of TGA. There is conflicting evidence as to whether an episode of TGA predisposes to future seizures or dementia.
Transient global amnesia (TGA) is characterized by the sudden onset of transient, anterograde amnesia without further focal neurologic deficits.1–6 Mental status is overall normal but may include mild confusion.1,2 Research suggests that the diagnosis is missed 90% of the time at initial presentation, often resulting in extensive and perhaps unnecessary evaluations.3
| Clinical recommendation | Evidence rating | Comments |
|---|---|---|
| TGA should be considered in a patient with less than six hours of amnesia, no focal neurologic findings, and diffusion-weighted magnetic resonance imaging with hippocampal bright lesions.1,6 | C | Expert opinion and case studies |
| Any amnesic episode lasting longer than 24 hours is unlikely to be TGA and warrants additional evaluation.1 | C | Definition, expert opinion, and many case studies |
| If the diagnosis of TGA is certain, only supportive treatment is indicated.6 | C | Case studies |
Epidemiology
The incidence of TGA is three to eight cases per 100,000 person years but increases to 23.8 cases per 100,000 in patients older than 50 years.2,4–6 A TGA episode is often preceded by a recent stressful physical or psychological event, with reports in the literature ranging from 52% to 89%.4–7 The most frequently cited precipitating events include acute illness, medical procedures, significant physical exertion, sexual intercourse, high-altitude environment, extreme temperatures, and Valsalva maneuver. 5–7 Triggering emotional events can be positive or negative; TGA has been associated with birth announcements, news of suicide, and in patients learning of worsening health troubles, family concerns, financial pressures, and higher-stress urban living situations.2,6–8
A history of migraine headache is the only diagnosis definitively associated with TGA, with a relative risk of 5.98.9,10 This is most prevalent among women 40 to 60 years of age.9,10 Other recent data suggest a higher rate of TGA in patients with hypertension and hyperlipidemia.11 Case reports of takotsubo cardiomyopathy happening concurrently with TGA have occurred, with an odds ratio of 2.3 in a cross-sectional study of U.S. hospitalizations.12 There have been additional reports of troponin I elevations or other concomitant cardiac events in the setting of TGA.13 Reports of TGA associated with severe COVID-19 have recently appeared, suggesting that the hypercoagulable state of COVID-19 may precipitate thrombotic strokes in the hippocampus.14 One case-control study demonstrated a relative risk of 8.4 for TGA associated with obstructive sleep apnea.15
Presentation
Patients may have nausea, vomiting, headache, mild dizziness, or subjective visual blurring.1,2,4 Patients with TGA report feeling disoriented to time and believe that something is wrong with them.1,2 This disorientation and sensation occur because of the patient's inability to encode new information with their episodic (short-term) memory. During the TGA episode, patients commonly ask repetitive questions such as “Where am I?” or “How did I get here?” Due to maintained procedural memory, learned functions such as eating, language, and driving are not impaired. TGA may last less than an hour, usually resolves within six hours, and always resolves within 24 hours.2,16 The diagnostic criteria require that the episode be witnessed by reliable people present for most of the episode, with no reported seizure activity or recent head trauma in the patient as well as all other criteria in Table 1.1
| Anterograde amnesia must occur during the episode |
| Cognitive impairment is limited to amnesia |
| Episode must resolve within 24 hours |
| Episode must be witnessed by a reliable witness |
| No clouding of the consciousness or loss of personal identity occurs |
| No focal neurologic signs or symptoms occur |
| No occurrence of recent head injury or active seizures |
Differential Diagnosis
Other diagnoses should be considered when evaluating a patient with symptoms of amnesia. Another rare diagnosis with symptoms similar to TGA is transient epileptic amnesia. However, transient epileptic amnesia presents with short, rapid recurrences of amnesia attributable to seizure activity. Other disorders include undiagnosed concussion, metabolic or infectious encephalopathy, delirium, benzodiazepine or alcohol intoxication, encephalitis, and nonconvulsive status epilepticus.2,17,18 Atypical migraine or psychiatric disorders, such as conversion disorder or dissociative amnesia, may also be considered. Most of these diagnoses can be excluded with careful consideration of the historical presentation and a complete physical and neurologic examination. TGA is characterized by spontaneous return to baseline function, typically within hours of the event. Dissociative amnesia will often last for days or longer and be in the context of underlying psychiatric diagnoses. If nausea and dizziness are pervasive with the amnesia, consider vertebrobasilar insufficiency (Table 2).
| Diagnoses | Risk factors | Precipitating factors | Duration | Associated neurologic symptoms | Magnetic resonance imaging | Electroencephalography | Recurrence of episodes |
|---|---|---|---|---|---|---|---|
| Cerebrovascular accident/transient ischemic attack | Many (e.g., atrial fibrillation, diabetes mellitus, dyslipidemia, hypertension, smoking) | No | Minutes to permanent impairment | Usually | Positive DWI with T2 fluid-attenuated inversion recovery lesion | Normal or slowing | Low |
| Migraine headache | Genetic, dietary | Yes, numerous triggers | Four to 72 hours | Auras (visual, sensory, motor, or language abnormalities) up to 30%; occasional transient focal paralysis | Normal | Normal | High |
| Transient epileptic amnesia | None | Yes (waking) | Less than 60 minutes (often, only a few minutes) | Yes (oral automatism, olfactory or gustatory hallucinations) | Normal/hippocampal sclerosis or atrophy | Abnormal (temporal or frontotemporal regions) | High |
| Transient global amnesia | Migraine | Yes | Up to 24 hours | Visual blurring | Hippocampal DWI hyperintensity or normal | Normal | Low |
| Vertebrobasilar insufficiency | Vascular (e.g., atrial fibrillation, diabetes mellitus, dyslipidemia, hypertension, smoking) | No | Less than 24 hours | Yes | Ischemic lesions in hippocampus | No, or slowing | Rare |
Evaluation
Although TGA is diagnosed clinically, a thorough history and physical examination must be completed, and a complete blood count with differential and a complete metabolic panel, including liver function tests, C-reactive protein, ammonia level, erythrocyte sedimentation rate, urine toxicology, serum ethanol level, and thyroid-stimulating hormone, should be considered to exclude other etiologies. Although magnetic resonance imaging is not required to make the diagnosis of TGA, in the first 24 hours of symptom onset, there have been documented transient abnormalities on diffusion-weighted imaging appearing as bright punctate lesions in the hippocampus,6,18–20 and 93% of patients will demonstrate hippocampal lesions within 12 to 24 hours of amnesia onset.18 Lesions generally begin to disappear after 72 hours and achieve complete resolution within 10 days.2,18 An additional benefit of magnetic resonance imaging is in establishing or ruling out other causes of transient amnesia, including cortical or vertebrobasilar cerebrovascular accident, in which case magnetic resonance angiography should be considered. Computed tomography, electroencephalography, and positron emission tomography do not show findings specific to TGA.20,21
Pathophysiology
Short-term memory formation is centered around the hippocampus, and isolated injury to this region has been suspected in TGA. Events that increase intrathoracic pressure are associated with TGA and may cause jugular venous hypertension, suggesting that impedance of venous drainage from the hippocampus is involved. Impedance of venous drainage is hypothesized to cause transient ischemia from secondary poor perfusion and sludging.22–25 The association between migraine headache and TGA has not been clarified, but hippocampal migraine vascular changes have been hypothesized. The increased prevalence in older patients suggests that age-associated intracerebral changes, especially vascular changes, may increase the risk of TGA. However, individuals with a history of cerebrovascular accident, hypertension, dyslipidemia, coronary artery disease, atrial fibrillation, peripheral vascular disease, or smoking do not have an increased risk of TGA.26
Management
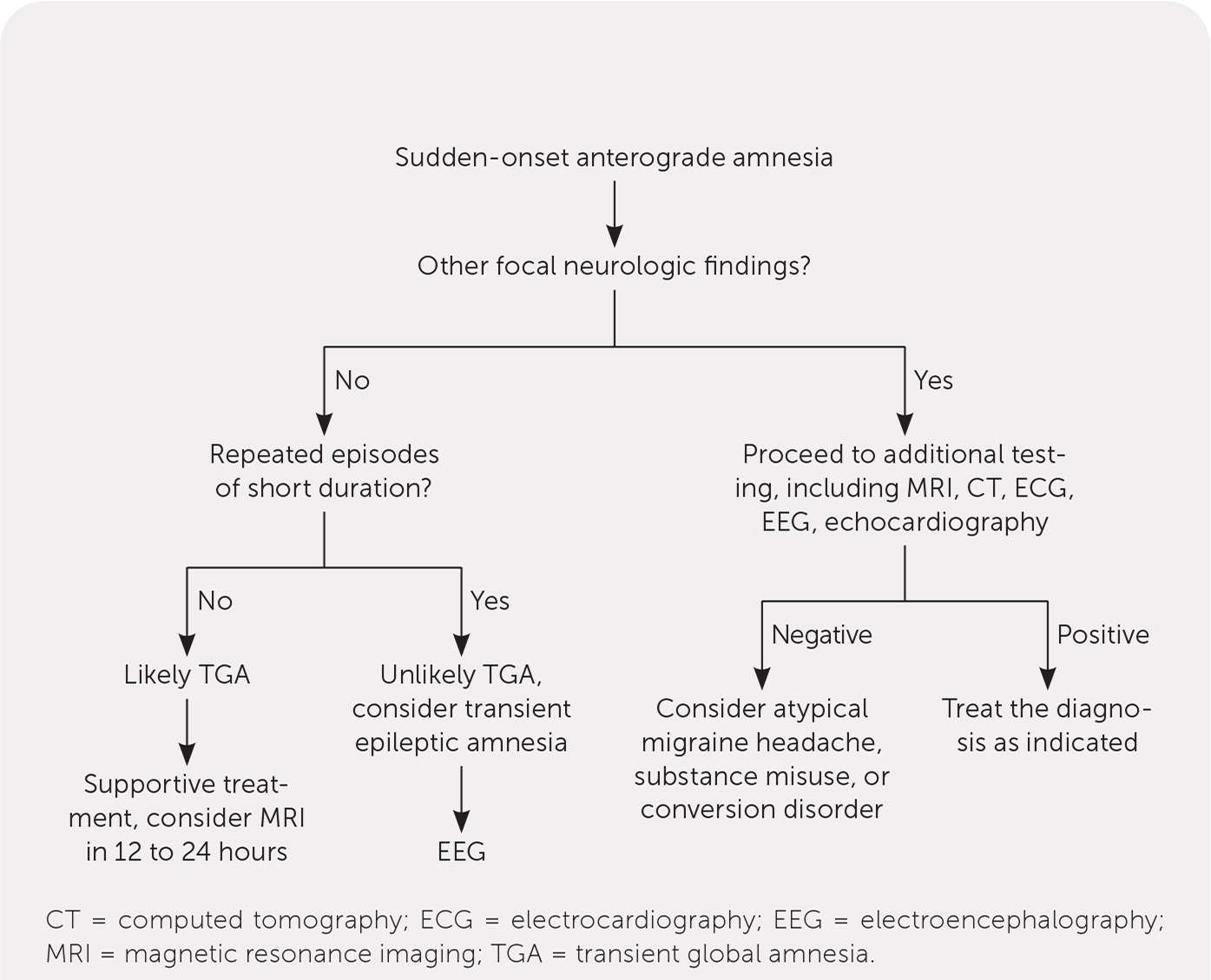
If the presentation is clear and the diagnosis is not in question, no specific intervention is necessary other than reassurance.3,6 Most patients presenting with TGA will recover within six hours and do not require imaging if they fit the diagnostic criteria.3,6 If the diagnosis is in question, then further evaluation is appropriate. If the patient presents before the resolution of amnesia, workup is essentially mandatory (Figure 1).
Prognosis
The prognosis of TGA is uniformly good. Population-based studies do not demonstrate an increased risk of cerebrovascular accident after an episode of TGA.27 Some retrospective studies suggest an increased subsequent risk of dementia28 and seizure,29 but older studies do not agree. The published TGA recurrence rate ranges from 2.9% to 23.8%.1,2 The largest retrospective study on TGA indicated that the recurrence rate is increased for patients with a history of migraines, a family history of migraine, or onset of the initial episode at younger than 50 years.26
Data Sources: A PubMed search was conducted multiple times from 2018 through January 2021, with key words transient global amnesia, transient amnesia, migraine and amnesia, transient epileptic amnesia, and diffusion-weighted imaging. Additional searches included our local MRI database, the Cochrane Database of Systematic Reviews, and Essential Evidence Plus. Search date: September 11, 2021.
