
Am Fam Physician. 2022;105(1):99-102
Author disclosure: No relevant financial relationships.
Key Points for Practice
• In embolic stroke of an uncertain source, further workup with long-term cardiac monitoring, transesophageal echocardiography, and cardiac magnetic resonance imaging should be considered.
• In nonembolic strokes, antiplatelet therapy and cardiovascular risk reduction can reduce recurrent stroke risk.
• Neither anticoagulation nor antithrombotic therapy appears to reduce risk in embolic stroke of uncertain source.
From the AFP Editors
Stroke is a common source of morbidity and mortality in the United States. Between 20% and 25% of strokes occur in patients with a previous stroke or transient ischemic attack. More than 90% of the global stroke burden can be traced to the modifiable risk factors of blood pressure, diet, physical inactivity, smoking, and abdominal obesity. The American Heart Association and American Stroke Association (AHA/ASA) published updated guidelines for preventing recurrent ischemic stroke, focusing on overall cardiovascular risk reduction and targeted secondary prevention.
Stroke Subtype Classification
Ischemic strokes account for nearly 90% of strokes in the United States. The TOAST (Trial of Org 10172 in Acute Stroke Treatment) classification scheme groups ischemic strokes into lacunar or nonlacunar subtypes. Lacunar strokes present with a specific syndrome pattern and can have normal imaging or subcortical ischemic areas less than 0.6 in (1.5 cm) in diameter.
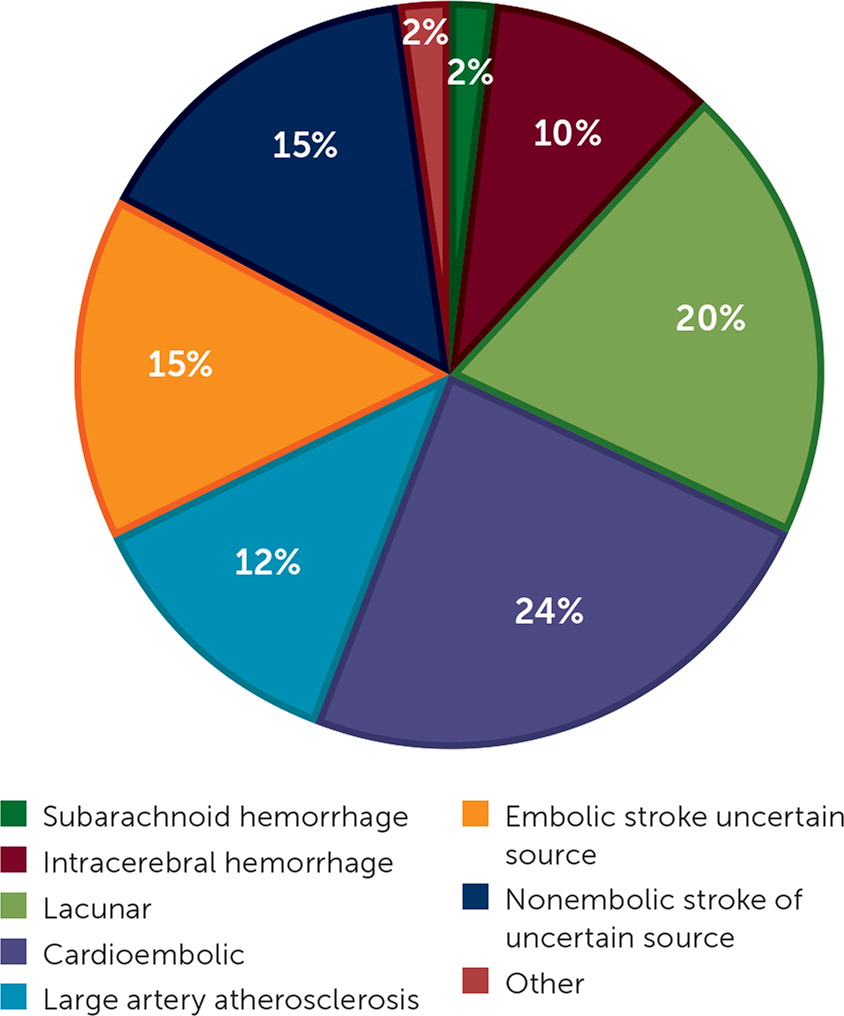
Nonlacunar strokes can be caused by cardioembolism, large artery atherosclerosis, and cryptogenic sources. Cardioembolic sources are suggested when previous or current ischemia occurs in multiple vascular territories. Large artery atherosclerotic lesions may present with cortical, brainstem, cerebellar, or larger subcortical areas of ischemia. Cryptogenic strokes defy characterization despite complete evaluations and again subdivide into embolic or nonembolic strokes of uncertain source. Embolic strokes of an uncertain source are nonlacunar and appear embolic, but no source of embolus can be identified. Figure 1 details the relative frequency of different stroke subtypes.
Diagnostic Evaluation
After a stroke, the subtype can usually be determined from initial testing, including computed tomography, magnetic resonance imaging, electrocardiography, continuous cardiovascular monitoring, echocardiography, and laboratory analyses. When initial imaging does not show ischemia after a stroke, imaging can be repeated seven days after the index event to look for ischemic changes.
Extracranial carotid imaging and contrast imaging studies can be performed with the initial evaluation. Carotid imaging is vital for strokes affecting the anterior circulation, and vertebrobasilar imaging is recommended for strokes outside of the anterior circulation.
For cryptogenic stroke without a suspected embolic source, testing for hypercoagulation and vasculitis should be considered. If an embolic source is suspected, further testing with long-term or implantable cardiac rhythm monitoring, transesophageal echocardiography, or cardiac magnetic resonance imaging is recommended. In embolic strokes of an uncertain source, findings from transesophageal echocardiography will change management in 14% of patients. Up to 16% of patients with embolic strokes of an uncertain source will have paroxysmal atrial fibrillation identified with prolonged cardiac monitoring. Evidence is insufficient to recommend a specific prolonged cardiac monitoring strategy for these patients.
Secondary Cardiovascular Prevention
Secondary stroke prevention includes cardiovascular risk reduction, as shown in Table 1. AHA/ASA guidelines recommend a blood pressure treatment goal of less than 130/80 mm Hg after all strokes and low-density lipoprotein cholesterol goals of less than 70 mg per dL (1.81 mmol per L) for nonembolic strokes. If triglycerides are greater than 135 mg per dL (1.53 mmol per L) in nonembolic strokes, adding icosapent ethyl can reduce the risk of current stroke but increase the risk of atrial fibrillation. A Mediterranean-type diet is the primary dietary recommendation, and limiting salt to 2.5 g daily is reasonable. AHA/ASA recommends at least four weekly 10-minute periods of moderate-intensity physical activity or two high-intensity 20-minute periods. Smoking cessation is strongly recommended, and alcohol cessation or reduction to no more than two drinks per day for men and no more than one per day for women is recommended.
| Risk domain | Management strategy | Explanation |
|---|---|---|
| Alcohol | Elimination or reduction in alcohol consumption in males drinking more than two and females drinking more than one alcoholic drink a day | 3.8% of strokes are estimated to be attributed to alcohol intake |
| Drugs | Cessation | Especially intravenous drug users treated for infective endocarditis |
| Glycemic control | Goal A1C of 7% or less to decrease microvascular complications | Metformin combined with a glucagon-like peptide-1 agonist or a sodium-glucose cotransporter 2 inhibitor are recommended |
| Hyperlipidemia | After nonembolic stroke, treat with atorvastatin (Lipitor), 80 mg daily, if low-density lipoprotein cholesterol level is greater than 100 mg per dL (2.59 mmol per L);in high-risk patients, consider adding ezetimibe (Zetia) and proprotein convertase subtilisin/kexin type 9 inhibitor to lower stroke risk | Consistent with 2018 American College of Cardiology/American Heart Association hyperlipidemia guidance |
| Hypertension | Lower blood pressure to less than 130/80 mm Hg | Evidence for secondary prevention in patients previously diagnosed with hypertension; lowering blood pressure to 130/80 mm Hg in most patients with a history of ischemic stroke seems safe based on trial data |
| Hypertriglyceridemia | When triglycerides are 135 to 499 mg per dL (1.53 to 5.64 mmol per L) in patients already taking a moderate- or high-intensity statin, consider adding icosapent ethyl | In one study, icosapent ethyl reduced cardiovascular events including stroke complicated by increased atrial fibrillation |
| Nutrition | Mediterranean-style diet, consider reducing sodium to 1 g per day | — |
| Obesity | Weight loss | Risk improves with modest weight loss, although evidence is limited |
| Physical activity | Moderate-intensity exercise for 10 minutes four times per week or 20 minutes of vigorous activity twice a week | In one study, exercise reduced recurrent stroke by an odds ratio of 6.7 |
| Smoking | Cessation using multibehavioral and evidence-based interventions, including avoidance of secondhand smoke | Smoking doubles the risk of a recurrent event |
| Stimulants | Cessation | Methamphetamine and cocaine increase risk |
Stroke-Specific Secondary Prevention
Stroke-specific secondary prevention depends on the stroke subtype and identified cause as described in Table 2.
| Cause of ischemic stroke | Recommended management |
|---|---|
| Antiphospholipid syndrome | In confirmed cases, warfarin (Coumadin) titrated to an international normalized ratio of 2 to 3 is recommended If antibody test is positive only once, antiplatelet therapy is recommended |
| Cardiac tumor | Tumor resection reduces recurrent stroke |
| Cardiomyopathy with or without a left ventricular assist device | Anticoagulation with warfarin for 3 months If a mechanical assist device is in place, combination therapy with warfarin and aspirin is recommended |
| Congenital heart disease after Fontan palliation | Anticoagulation with warfarin |
| Dissection of carotid or vertebral arteries | Anticoagulation is recommended for 3 months to prevent embolism despite lack of evidence Warfarin or aspirin offers similar benefit over the following 3 months |
| Extracranial carotid stenosis | If severe carotid artery stenosis (≥ 70%), carotid endarterectomy recommended within 7 days If moderate carotid artery stenosis, consider carotid endarterectomy Carotid artery stenting is a reasonable alternative in limited situations |
| Extracranial vertebral stenosis | Antiplatelet therapy and cardiovascular risk reduction Neither stenting nor surgery has shown benefit |
| Fibromuscular dysplasia | Urgent cardiovascular risk reduction per Table 1 Consider antiplatelet therapy if dissection |
| Giant cell arteritis | High-dose oral glucocorticoids Consider adjunctive methotrexate or tocilizumab (Actemra), but avoid infliximab (Remicade) |
| Hypercoagulable states (prothrombin 20210A, activated protein C resistance, elevated Factor VIII levels, or protein C, protein S, or antithrombin III deficiencies) | Antiplatelet therapy is reasonable |
| Infective endocarditis | Surgery recommended without intracranial hemorrhage or a major ischemic stroke |
| Intracranial atherosclerosis | Aspirin; for minor stroke or transient ischemic attack, consider adding clopidogrel (Plavix) for up to 90 days with severe stenosis or ticagrelor (Brilinta) for up to 30 days |
| Left ventricle thrombus | Anticoagulation with warfarin for 3 months, most often due to acute myocardial infarction |
| Moyamoya disease (occlusive disease of the circle of Willis) | Surgical revascularization with direct or indirect extracranial-intracranial bypass |
| Sickle cell disease | Blood transfusions to reduce hemoglobin S to less than 30% of total hemoglobin If transfusion is not practical, hydroxyurea (Siklos) therapy appears to reduce risk |
Antithrombotic therapy recommendations after a stroke depend on the stroke subtype and complicating conditions. In patients with stroke secondary to atrial fibrillation, direct-acting oral anticoagulants are preferred unless atrial fibrillation is complicated by moderate or severe mitral stenosis or a mechanical heart valve. Patients with minor nonembolic strokes and high-risk transient ischemic attacks should receive dual antiplatelet therapy with aspirin and clopidogrel (Plavix) for 21 to 90 days, followed by continued treatment with either medication alone. Although antiplatelet therapy reduces recurrent stroke after all nonembolic strokes, embolic strokes of an uncertain source do not appear to benefit from antiplatelet or anticoagulant therapy.
Carotid endarterectomy is beneficial after stroke when ipsilateral extracranial internal carotid stenosis is 70% or greater. Endarterectomy is reasonable with ipsilateral stenosis of 50% to 69% in patients who are at lower surgical risk. Carotid artery stenting may be a reasonable alternative to endarterectomy in certain low-risk patients.
When a patent foramen ovale is found after an embolic stroke of an uncertain source in an adult up to 60 years of age, closure may be beneficial if an exhaustive workup has been performed. Evaluation may include intracranial contrast imaging, advanced cardiac imaging, lower extremity venous ultrasonography, prolonged cardiovascular rhythm monitoring, and evaluation for infective endocarditis, hypercoagulable syndromes, antiphospholipid syndromes, and vasculitis syndromes. If the stroke is still unexplained, small trials suggest benefit from foramen ovale closure, especially with an atrial septal aneurysm or large right-to-left shunting.
Behavioral Interventions
Behavioral change interventions focusing on health and stroke literacy, lifestyle risk factors, and adherence to therapeutic strategies decrease stroke recurrence.
The views expressed are those of the authors and do not necessarily reflect the official policy or position of the Department of the Navy, Uniformed Services University of the Health Sciences, Department of Defense, or the U.S. government.
Editor's Note: The key changes to this AHA/ASA guideline update are new recommendations for diagnostic workup after ischemic stroke and grouping of recommendations by ischemic stroke type. Angioplasty and stenting of intracranial lesions are no longer recommended, with aggressive medical management recommended instead. Closure of a patent foramen ovale is now an option in younger patients with nonlacunar stroke after a negative extended evaluation. Only anticoagulants and ticagrelor have been studied after embolic strokes of an uncertain source, and neither appears to reduce rates of recurrent stroke.
The recommendation for icosapent ethyl is controversial because benefit was demonstrated in a single trial with possible flaws, as discussed in a previous dyslipidemia guideline summary. (https://www.aafp.org/afp/2021/0415/p507.html). A subsequent large trial failed to show any benefit of icosapent ethyl, making this recommendation more questionable.1
The most recent AFP article on recurrent stroke prevention (https://www.aafp.org/afp/2017/1001/p436.html) was based on the 2015 AHA/ASA guideline.—Michael J. Arnold, MD, Contributing Editor
Reference
1. Nicholls SJ, Lincoff AM, Garcia M, et al. Effect of high-dose omega-3 fatty acids vs. corn oil on major adverse cardiovascular events in patients at high cardiovascular risk: the STRENGTH randomized clinical trial. JAMA. 2020;324(22):2268–2280.
Guideline source: American Heart Association/American Stroke Association
Evidence rating system used? Yes
Systematic literature search described? Yes
Guideline developed by participants without relevant financial ties to industry? No
Recommendations based on patient-oriented outcomes? Yes
Published source: Stroke. July 2021;52(7):e364–e467 (published correction appears in Stroke. 2021;52[7]:e483–e484)
