CDC Reports Mixed Progress Fighting Antibiotic Resistance
November 26, 2019 11:15 am News Staff – On average, someone in the United States develops an antibiotic-resistant infection every 11 seconds, and every 15 minutes, someone dies from such an infection.
That's according to the CDC report Antibiotic Resistance Threats in the United States, 2019, which was released Nov. 13.
According to the report, antibiotic-resistant bacteria and fungi cause more than 2.8 million infections and 35,000 deaths in the United States each year.
Add in infections caused by Clostridioides difficile -- a bacterium that, although not typically antibiotic-resistant, is associated with antibiotic use -- and the annual toll of threats covered in the CDC report exceeds 3 million infections and 48,000 deaths.
The new report used data sources that weren't available when the agency first released an antibiotic-resistant infection report in 2013, and more recent recalculations of that older data have indicated that totals in the earlier report were woefully underestimated. Still, the CDC said prevention efforts have reduced deaths from antibiotic-resistant infections by 18% overall and by more than 27% in hospitals since the previous report was published.
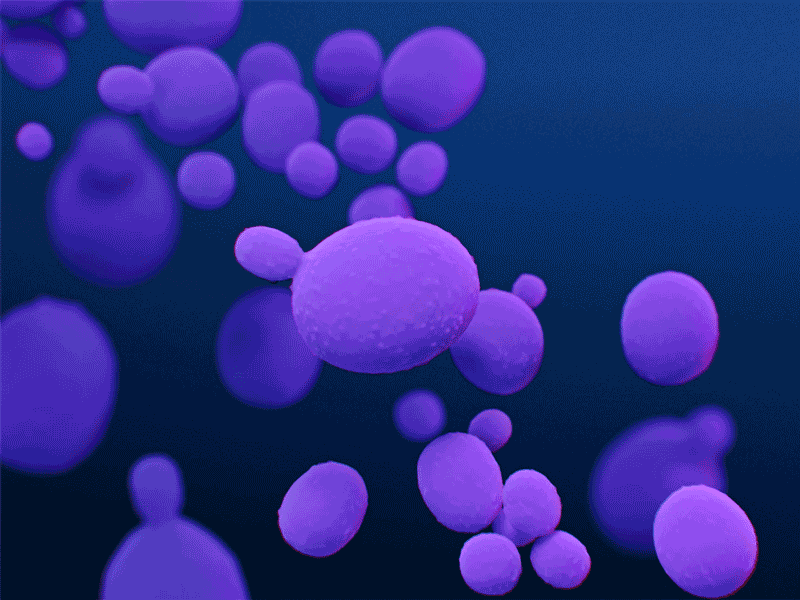
This medical illustration, presented in the CDC report Antibiotic Resistance Threats in the United States, 2019, depicts Candida auris fungal organisms.
"The 2013 report propelled the nation toward critical action and investments against antibiotic resistance," said CDC Director Robert Redfield, M.D., in an accompanying press release. "Today's report demonstrates notable progress, yet the threat is still real. Each of us has an important role in combating it. Lives here in the United States and around the world depend on it."
Report Highlights
In addition to establishing a new national baseline of infections and deaths from antibiotic-resistant pathogens, the new report has categorized the top antibiotic-resistant threats based on their relative level of hazard to human health: urgent, serious or concerning.
Like the previous report, the 2019 report assessed the relative threat level for each pathogen according to seven factors:
- clinical impact,
- economic impact (when available),
- incidence,
- 10-year projected incidence,
- transmissibility,
- availability of effective antibiotics and
- barriers to prevention.
It's worth noting that although the CDC assessment focused on each pathogen's domestic impact, the report's authors did look at international context when estimating 10-year incidence projections. Not surprisingly, they anticipate that urgent and serious threats will require greater attention and swifter action.
Story Highlights
Here's the full list of antibiotic-resistant threats by category:
Urgent Threats
- carbapenem-resistant Acinetobacter (listed as serious in the 2013 report)
- Candida auris (not previously listed)
- C. difficile
- carbapenem-resistant Enterobacteriaceae
- drug-resistant Neisseria gonorrhoeae
Serious Threats
- drug-resistant Campylobacter
- drug-resistant Candida
- extended spectrum β-lactamase-producing Enterobacteriaceae
- vancomycin-resistant Enterococci
- multidrug-resistant Pseudomonas aeruginosa
- drug-resistant nontyphoidal Salmonella
- drug-resistant Salmonella serotype Typhi
- drug-resistant Shigella
- methicillin-resistant Staphylococcus aureus
- drug-resistant Streptococcus pneumoniae
- drug-resistant tuberculosis
Concerning Threats
- erythromycin-resistant group A Streptococcus
- clindamycin-resistant group B Streptococcus
Vancomycin-resistant S. aureus, which was listed as concerning in 2013, doesn't appear at all in the 2019 report. Only 14 cases have been seen in the United States since 2002, and they were all isolated, with no documented patient-to-patient spread. Still, the CDC said it will continue to monitor VRSA as part of the agency's ongoing work to reduce Staphylococcus infections in health care facilities and the community.
The report did call out three additional threats, placing them on a so-called Watch List. These pathogens -- azole-resistant Aspergillus fumigatus, drug-resistant Mycoplasma genitalium and drug-resistant Bordetella pertussis -- are currently responsible for few, if any, U.S. infections. However, they either are known to be causing infections in other parts of the world, have the potential to rapidly spread or simply are not well understood at this time. Early detection and prevention of infections caused by these agents could have a significant public health impact.
Regarding estimated numbers of infections, drug resistant S. pneumoniae was the top offender, with 900,000 infections. Next was drug-resistant N. gonorrhoeae, with 550,000 infections, followed by drug-resistant Campylobacter, with 448,400 infections; MRSA, with 323,700 cases; and C. difficile, with 223,900 cases in hospitalized patients. C. difficile was responsible for the highest estimated number of deaths, at 12,800, followed by MRSA, with 10,600; ESBL-producing Enterobacteriaceae, with 9,100; VRE, with 5,400; and drug-resistant S. pneumoniae, with 3,600.
Mixed Progress
Despite the fact that resistance to essential antibiotics appears to be increasing in seven of the 18 pathogens examined, according to the CDC, significant progress has been made in preventing infections and deaths from resistant threats typically associated with hospitals. As noted above, deaths from antibiotic-resistant infections in hospitals dropped nearly 28% between 2012 and 2017.
Nevertheless, antibiotic-resistant threats often found in health care -- including CRE, MRSA and others -- were responsible for more than 85% of the total deaths calculated in the report.
A number of CDC strategies -- preventing the spread of resistant threats, preventing device- and procedure-related infections, implementing its containment strategy to stop the spread of emerging threats, and improving antibiotic use in outpatient settings -- have helped hospitals and public health departments combat the antibiotic-resistant threats across the nation.
However, the agency said it remains concerned about three antibiotic-resistant infections that are on the rise in the community:
- More than half a million resistant gonorrhea infections occur each year, double the number reported in 2013. N. gonorrhoeae has developed resistance to all but one class of antibiotics, and half of all infections are resistant to at least one antibiotic.
- As one of the leading causes of death among drug-resistant pathogens, ESBL-producing Enterobacteriaceae exacerbate urinary tract infections, especially in women, and could undo progress made in hospitals if allowed to spread there.
- Invasive infections from erythromycin-resistant group A Streptococcus have quadrupled since the 2013 report. If resistance continues to grow, infections and deaths could rise.
CDC Actions
The CDC's Antibiotic Resistance Solutions Initiative is designed to take a comprehensive approach to overcoming antibiotic resistance by
- significantly investing in each state through programs such as the AR Laboratory Network, which aims to rapidly detect and prevent antibiotic-resistant infections;
- partnering with groups such as CMS, the Agency for Healthcare Research and Quality, and other federal partners, data experts and health care professionals to improve the use of currently available antibiotics;
- continuing to supply samples of resistant pathogens from the AR Isolate Bank to drug and diagnostic test developers to find new drugs and treatments;
- investing millions of dollars to find prevention strategies that can be scaled up across the nation;
- working with private industry to enhance food product safety, medical devices and surveillance capabilities; and
- coordinating with domestic partners to expand national response and prevention capacity, as well as with global partners to enhance the ability to combat antibiotic resistance worldwide.
Related AAFP News Coverage
AHRQ Recruiting Clinics for Antibiotic Stewardship Program
(8/2/2019)
Study Shows Antibiotic Prescribing Lowest in Medical Offices
(8/2/2018)
More From AAFP
Choosing Wisely: Antibiotics for Otitis Media